 Case Report
Case Report
Tiny Limb, Giant Challenge: Management of A Neonatal Arteriovenous Malformation of the Upper Extremity
Jael Carbajal1, Maria Matuszczak1, Rhashedah Ekeoduru1, Elizabeth Rugutt1, Matthew Greives2, Jose Espinoza3 and Sabina Khan1*
1Department of Anesthesiology, Critical Care, and Pain Medicine, McGovern Medical School at UT Health, Texas Medical Center Houston, Texas, USA
2Department of Pediatric Plastic and Reconstructive Surgery, McGovern Medical School at UT Health, Texas Medical Center Houston, Texas Medical Center Houston, Texas, USA
3McGovern Medical School at UT Health, Texas Medical Center Houston, Texas, USA
Sabina Khan, Division of Pediatric Anesthesiology, Critical Care, and Pain Medicine, McGovern Medical School at UT Health, Texas Medical Center Houston, Texas, USA
Received Date:March 18, 2024; Published Date:April 16, 2024
Abstract
We present a case report detailing the perioperative management of a neonate with a congenital giant arteriovenous malformation (AVM) in the right upper extremity (RUE) undergoing surgical resection. The case was complicated by the necessity for rapid and massive transfusion in the context of high-output cardiac failure and pulmonary hypertension.
Introduction
Arteriovenous malformations (AVM) are rare vascular anomalies that can lead to high output cardiac failure [1]. AVMs represent high-flow shunts, causing increased cardiac output, high stroke volume, and ventricular dilation [2]. Left ventricular failure can result in secondary pulmonary hypertension due to elevated pulmonary venous pressure [3]. During AVM resection, massive transfusion can worsen preexisting heart failure and pulmonary hypertension.
AVMs cause ischemia by diverting blood flow from affected structures, leading to pain, ulceration, and bleeding. Treatment involves embolization or surgical resection, but surgery poses risks like significant blood loss and potential AVM recurrence [4].
In this case, we describe the anesthetic management of a giant AVM resection, highlighting the challenge of balancing transfusion needs with cardiac and pulmonary concerns.
Case Description
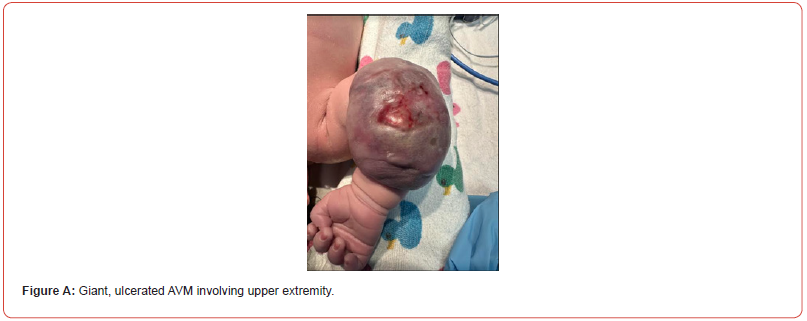
A 14-day old, 3.6 kg infant presented for resection of a right upper extremity giant ulcerated AVM with abnormal coagulation studies. Despite initial treatment with sirolimus, the malformation expanded from 14 cm at birth to 17 cm by the time of surgical presentation. Initial attempts at IR embolization were unsuccessful due to inability to identify a feeding artery. CT and MRI findings revealed a large forearm AVM with enlarged brachial artery and veins extending from the right axilla throughout the right upper extremity. Due to pulmonary hypertension causing increasing work of breathing and eventual hypoxic respiratory failure, the infant was intubated and treated with inhaled nitric oxide at 20 parts per million. A preoperative echocardiogram revealed supra-systemic right sided pressures with moderate hypertrophy, right ventricular dilation and moderately depressed systolic function, while on milrinone and furosemide.
Preoperatively, a multidisciplinary team discussion focused on the risks of acute blood loss, challenges utilizing a tourniquet due to the AVM location, potential limb ischemia, venous air embolism, and exacerbation of pulmonary hypertension. Two units of packed red blood cells (PRBC) and fresh frozen plasma (FFP), and one unit of platelets were available.
The child arrived to the operating room intubated with an existing 22 g left arm peripheral IV, a right leg peripherally inserted central catheter (PICC) and a left posterior tibial arterial line. After an uneventful intravenous anesthesia induction, an esophageal stethoscope was inserted. Additional access was obtained via placement of a right femoral 4 Fr central line. Prior to surgical start, a warmed PRBC infusion was initiated pre-emptively. Additionally, Tranexamic acid was initiated at a rate of 10 milligram/kilogram/ hour to decrease expected blood loss.
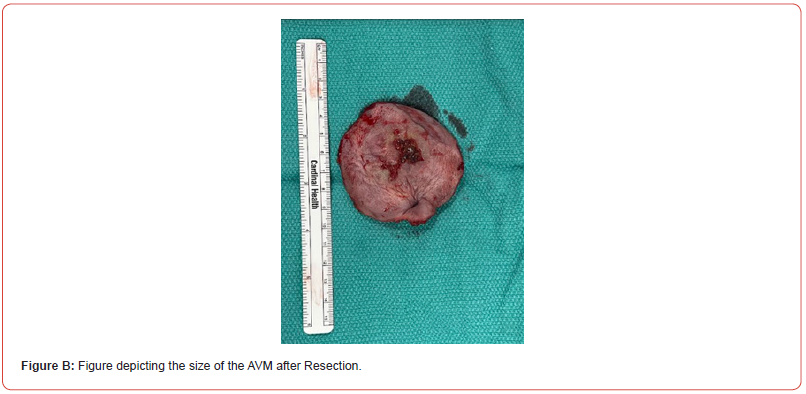
Despite efforts to curtail blood loss, the infant lost over half blood volume within ten minutes of incision. Aggressive volume resuscitation and electrolyte repletion was initiated. The AVM surgical resection took approximately 2 hours to complete. Total blood loss was 350 ml, the patient’s total blood volume, over the course of the operation. Total blood products administered included 243 ml of PRBC (66.6 ml/kg), 175 ml of FFP (47.9 ml/kg), and 70 ml of platelets (19.2 ml/kg). Successful resuscitation was evidenced at closure by an arterial blood gas showing a pH of 7.35, hematocrit of 35, potassium level of 5 mEq/L, and normal lactate and base excess levels. A post-closure Doppler ultrasound by the surgical team confirmed the vascular integrity of the right upper extremity.
The infant’s post-surgical course showed promising outcome as evidenced by significant improvement in cardiac and pulmonary dynamics on echocardiogram. Allograft placement and closure of the right arm was performed without complications 2 weeks after primary AVM resection. The patient was discharged home on room air on day 41 of life.
Discussion
AVMs represent high-flow shunts either through direct arteriovenous fistulas or niduses of arteries connecting to veins. These abnormal connections may lead to pulmonary over circulation and eventually to pulmonary hypertension. The consequence echocardiogram is high output, right ventricular cardiac failure [4].
The treatment for symptomatic AVMs often necessitates embolization before surgery to reduce the lesion’s size and minimize blood loss during surgical resection [4]. However, in our patient’s case, interventional radiology failed to identify a feeding artery for embolization. Consequently, the surgical and anesthesiology teams anticipated significant blood loss during AVM resection.
This case’s significance lies in the abrupt loss of over half the infant’s blood volume within the first ten minutes of resection. Such rapid and massive transfusion requirements in a short time can exacerbate high-output cardiac failure and pulmonary hypertension by increasing fluid load. This phenomenon, termed transfusionassociated circulatory overload (TACO), can lead to pulmonary edema, worsening dyspnea, and respiratory compromise [5]. Additionally, the patient was at risk of venous air embolism, therefore, esophageal stethoscope was placed as a monitoring tool. Fortunately, the patient did not exhibit any evidence of a venous air embolism.
This case outlines the need for meticulous surgical and anesthetic planning when managing medically complex neonates suffering from the complications of a congenital giant AVM. Continuous communication between surgical and anesthesiology teams is paramount. Care team members should be prepared to address significant blood loss during surgical resection efficiently. A multidisciplinary, coordinated approach must be implemented to care of these fragile patients.

Consent
Parental consent to use non-identifiable pictures was obtained prior to surgery as part of the surgical consent.
Acknowledgement
None.
Conflict of interest
No conflict of interest.
References
- Webb JB, Obrien M, John PR, Nishikawa H (2004) Early presentation of an extremity arteriovenous malformation. The British Association of Plastic Surgeons 57(8): 785-788.
- Federico Liberman, Roberto Cooke, María J Cabrera, Santiago Vigo, Guillermo Allende, et al. (2002) High-output heart failure due to arteriovenous malformation treated by endovascular embolization. Br J Cardiol 29(3): 26.
- Moraes DL, Colucci WS, Givertz MM (2000) Secondary Pulmonary Hypertension in Chronic Heart Failure, The Role of the Endothelium in Pathophysiology and Management. Circulation 102(14): 1718-1723.
- Greene AK, Orbach DB (2011) Management of Arteriovenous Malformations. Clinics in Plastic Surgery 38(1): 95-106.
- Lanzkowsky P (2011) Chapter 31-Supportive Care of Patients with Cancer. Manual of Pediatric Hematology and Oncology 5th edition pp. 857-920.
-
Jael Carbajal, Maria Matuszczak, Rhashedah Ekeoduru, Elizabeth Rugutt, Matthew Greives, Jose Espinoza and Sabina Khan*. Tiny Limb, Giant Challenge: Management of A Neonatal Arteriovenous Malformation of the Upper Extremity. Anaest & Sur Open Access J. 4(5): 2024. ASOAJ.MS.ID.000600.
-
Arteriovenous malformations, Pulmonary hypertension, Surgical resection, Feeding artery, Ventricular cardiac failure, Anesthesiology, Pulmonary edema, Surgery
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






