 Review Article
Review Article
The Role of Psychosocial Interventions In Breast Cancer Patients
Jessica Dowling* and Lara Rapa
Department of Surgery, Mater Dei Hospital, Malta
Jessica Dowling, Department of Surgery, Mater Dei Hospital, Malta
Received Date:October 29, 2024; Published Date:November 05, 2024
Abstract
Breast cancer is the leading tumor within the female population worldwide [1]. It is a difficult diagnosis, and patients often feel anxious about treatment, distressed of the high mortality, nervous about recurrence and troubled with physical symptoms. All these factors significantly affect their daily lives [2].
The target of breast cancer care has shifted from diagnosis to survivorship, a term which encompasses the physical, mental, social, and economic aspects of cancer [3]. A range of non-technical skills have been tested and found to be beneficial in alleviating breast cancer distress. These include meditation, music therapy, relaxation and hypnosis [4]. Pre-procedural information is an asset in breast cancer screening, aids in obtaining informed consent and is a vital tool when offering breast reconstruction options. CBT is the most frequently used technique in allaying distress in breast cancer patients [5].
Keywords:Breast cancer; Preprocedural information; Cognitive behavioural therapy; Hypnosis
Abbreviations:CBT: Cognitive behavioural therapy; RCT: Randomised controlled trial; MBI: Mindfulness-based intervention; MBCT: Mindfulnessbased cognitive therapy; MBSR: Mindfulness-based stress reaction
Introduction
Treatment of breast cancer has seen major advancements in medical care but can fail to tackle psychosocial issues [6]. Cancer patients may experience a range of psychosocial issues like anxiety, depression, fear and problems with coping and clinicians should ensure that these problems are identified and adequately addressed through a range of techniques to alleviate patient distress [7]. As treatments advance and survivorship increase, it is of utmost importance to treat the impact of breast cancer with evidence-based techniques [8].
Preprocedural information
Evidence based information is a precondition for informed decisions in any healthcare setting. Patients should be objectively informed about the pros and cons of any intervention to gain a good understanding and satisfy their informational needs [9]. This is in line with the European Charter of Patients’ Rights [10] which states that individuals should have the right to access all kinds of information relating to health to be able to take the best decisions about their health issues.
Breast cancer screening is a modern effective strategy to detect cancers at an early stage. However, some patients are not aware of the risks and benefits of screening mammography leading to unnecessary confusion [11] Emphasis is shifting from uninformed and persuasive approaches to informed decisions relating to specific outcomes [12]. Hersch et al. [13] suggested that decision aids provided evidence-based information regarding mortality risk, over detection and false positive risks and enabled women to have more awareness prior to participating in screening.
Through the InforMa RCT, Pérez-Lacasta et al. [14] advised that providing information on the benefits and harms of screening has produced better informed choices, increased acceptance of informational material and lower rates of conflicts when compared to the non-informed control group. Another study by Fernández- Feito et al. [15] evaluated the acceptability of patient information leaflets related to breast cancer screening. Their study concluded that women provided with information leaflets had a better understanding and acceptance of screening. They also suggested revision of information material with participants to improve existent content and format.
Patient information leaflets may also be used in obtaining informed consent for breast core biopsies. Although it is a minor procedure, principles of informed consent still apply. Pollard et al. [16] analysed the impact of detailed information on breast biopsy patients through two arm studies – patients with or without preprocedural information. Despite concerns at the introduction of the study relating to increased anxiety, most patients reported an improved experience thanks to the information provided. The authors also suggested information leaflets for one-stop breast assessment clinics as part of their recommendations [16].
Another sensitive topic that breast cancer patients may encounter in their treatment is breast reconstruction. Many patients undergoing mastectomy are offered breast reconstruction which may entail immediate or delayed reconstruction, implantbased, autologous or a combination of both. All options have their advantages and disadvantages, and patients should be made aware of these conditions for an informed decision [17]. Stege et al. [18] conducted an RCT where they created an online patient decision aid to assist patients that opt for breast reconstruction. They analysed decision conflicts and outcomes of patients with or without information aids and concluded that this new tool contributes significantly to improved outcomes.
As information and communication technologies advance and develop we must ensure that information is disseminated adequately to reach all populations including elderly, patients with different ethnic origins, patients with different literacy status and non-English speakers [16]. This empowers all patients presenting to any breast unit and provides equal access to information.
In summary, pre-procedure information has become an essential tool in any consultation. Leaflets are targeted at patients’ expectations, consider the most common preferences of the target population, and contain objective data for an informed decision [19]. They are valuable for breast patients as they allow dissemination of information to different groups of patients, across different platforms and about any intervention.
Cognitive behavioural therapy
Breast cancer is the commonest tumor among the female population [1]. Patients are concerned about mortality rates, anxious about their treatment, fear of recurrence and physical symptoms [2]. A few psychosocial factors can deal with these distressing thoughts, with CBT being the most frequently used technique [5].
CBT incorporates a hybrid of techniques and interventions to bring about cognitive, emotional, behavioural and social change. The interventions used in CBT include role play, problem solving interventions, coping mechanisms and offering separate ways of perception [20]. CBT may be particularly useful in breast cancer patients due to the psychological trauma that they might be going through upon diagnosis. Mastectomy can be very stressful as patients experience reduced self-worth and loss of femininity [21].
MBIs aids patients focusing on a particular moment, increasing awareness and instills compassionate attitudes through yoga, group discussion and meditation. These mechanisms lead to better control of emotions, behaviour, cognition and stability of the mind. The two common MBIs are MBCT and MBSR [22].
Park et al. [22] carried out a RCT of seventy-four ambulatory nonmetastatic breast cancer patients in Tokyo, Japan comparing eight weeks MBCT intervention versus wait-list control. The subjects in MBCT group had better outcomes in psychological distress, fatigue, quality of life and spiritual wellbeing when compared to the control group. Participants were analysed at baseline, week eight and week twelve of the trial. The difference between groups remained significant till four weeks post-intervention.
A RCT trial by Jelvehzadeh et al. [23] in Tehran, Iran evaluated the effect of CBT on quality of life and emotional disturbance in breast cancer patients. The authors recruited forty-eight women post mastectomy and chemotherapy and subjects were randomly assigned to a CBT arm (twenty-four patients) or a control group (twenty-four patients). Subjects were assessed before and after intervention and at one month after end of treatment as follow-up. CBT was found to improve emotional disturbance and quality of life. The best outcomes in CBT group were related to decreased level of anxiety, stress, depression and improved quality of life with no effect on death anxiety.
Insomnia and pain are two other psychosocial factors that influence breast cancer care. Insomnia is associated with mood disorders, reduced quality of life, immune function, inflammation and mortality rates. Insomnia and pain are intertwined in that lack of sleep worsens pain outcomes while prolonged pain alters sleep cycle and may lead to sleep deprivation [24]. CBT involves education, controlling stimuli, sleep restriction and good sleep hygiene to obtain an ideal sleep schedule. Ma et al. [25] evaluated the effect of CBT for insomnia by conducting a meta-analysis of fourteen RCTs. This main conclusion was that CBT is efficacious for reducing insomnia and improves sleep in breast cancer patients.
Padron et al. [26] imply that there is lack of research in CBT effects on insomnia and pain in gynaecology, particularly in breast. The first meta-analysis to evaluate CBT for distress and pain was carried out by Tatrow & Montgomery [27]and involved twenty studies. The analysis inferred that 62% and 69% of breast cancer patients in CBT treatment groups experienced less distress and pain respectively when compared to the control groups. The authors recommended more well-designed studies to reach better conclusions. Moorthy et al. [28] devised a protocol for a double blinded RCT in Dublin, Ireland to assess the effect of perioperative CBT on chronic post-surgery pain in breast cancer subjects.
A major benefit of CBT is its versatility in methods of delivery. Akkol-Solakoglu & Hevey [29] carried out a RCT in Ireland about internet-delivered CBT for anxiety and depression in breast cancer survivors. They recruited seventy-two participants randomised to two groups – a seven-module guided internet -based CBT in one arm and treatment as usual in the other arm. The intervention had 52.8% adherence rate. A lower depression rate was noted postintervention.
Another RCT by Savard et al. [30] in Quebec comparing videobased and professionally delivered CBT had conflicting findings with Akkol-Solakoglu & Hevey [29]. Two hundred forty-two women with nonmetastatic breast cancer who received radiotherapy in the previous eighteen months and had insomnia symptoms were included. Participants were randomly allocated into three groups – professionally administered CBT, video-based CBT and control group. All were assessed at three, six and twelve months. Nonvideo assistance by CBT resulted in greater improvements in insomnia, depression and fatigue.
There are only a few studies comparing traditional and more innovative ways to deliver CBT. Patient characteristics including education level, marital status, occupation, co-morbidity and cancer stage play a vital role in delivery methods. These factors could all influence the preferred method of CBT and further research is essential to determine the ideal mode of CBT for each specific group to be able to provide optimum patient care.
CBT has proven to be beneficial in allaying psychosocial factors that breast cancer survivors experience daily. Physical and human resources are to be properly allocated to implement this valuable option in any breast care unit.
Hypnosis
Breast cancer patients treated by surgery, chemotherapy or radiotherapy are vulnerable individuals from diagnosis to treatment. At the onset of disease, patients suffer from increased anxiety, distress and perceived cognitive decline and these factors subsequently have negative effects on quality of life, social and emotional function [31]. These cognitive aspects may influence acceptability and tolerance of treatment. A range of non-technical skills like meditation, yoga, music therapy, relaxation and hypnosis have been studied and found to be an integral part of breast cancer treatment [4].
Hypnosis is a state of inner absorption, concentration, and focused attention. It involves two key players, the hypnotist and the client who engage in hypnosis, a psychotherapeutic technique in the medical field. Self-control is an important aspect in hypnosis and the patient must be willing to participate with little to no resistance in the process to have a fruitful experience [32]. In hypnosis, the professional changes the patient’s consciousness level by shifting attention from the current situation to another more enjoyable setting. This state allows the client to step away from the situation and focus only on emotion, thoughts or images [33].
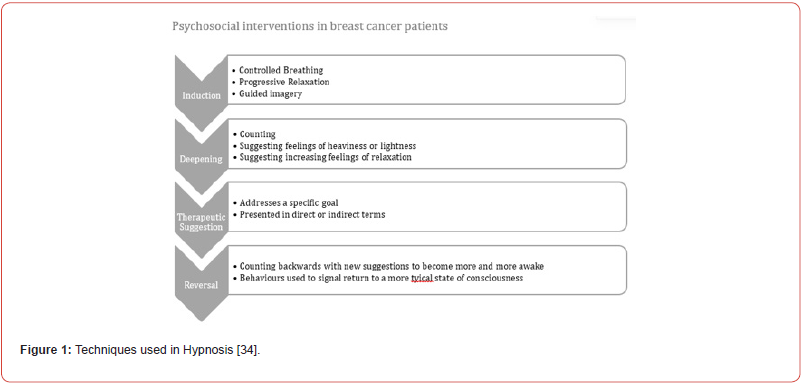
Hypnosis may be divided into four stages as per Figure 1 below.
Hypnosis can alleviate stress in any medical procedure. Benefits have been demonstrated in the preoperative, operative and postoperative phases. A meta-analysis by Schnur et al. [35] concluded that hypnosis reduced emotional upset, depression and anxiety and improved relaxation. Montgomery et al. [36] illustrates some findings from a prospective RCT carried out in Mount Sinai Medical Centre USA comprising two hundred breast patients who were randomised to hypnosis versus non-hypnosis study arms. A pre-surgical hypnotic session was found to reduce anaesthetic requirements, limit post-operative analgesia, nausea and vomiting and decrease emotional disturbance.
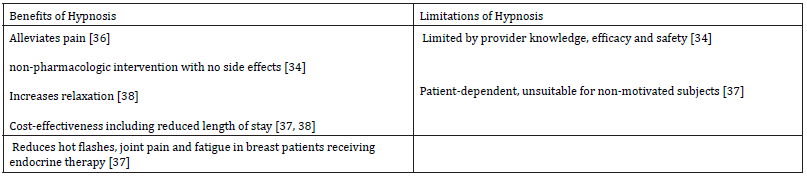
Berliere et al. [37] analysed the advantages of hypnosis in breast cancer patients. They carried out an observational non-RCT that recruited three hundred patients from a single centre in Belgium. One hundred fifty consecutive patients underwent breast surgery on general anesthesia while the rest underwent the procedure on hypnosis sedation. The study had some positive inferences as indicated in Table 1, however larger RCTs over multiple centers were suggested by the authors themselves.
Table 1 summarizes benefits and limitations of hypnosis from different studies.
Table 1:Benefits and Limitations of Hypnosis in Breast Patients.
Breast cancer surgery is usually followed by pain. In fact, around 25% of breast cancer patients experience pain up to nine months post-operatively [39]. Hypnosis has been tested and found to be useful in reducing post-operative pain. Hernandez et al. [40] carried out a RCT in Mexico to assess the effect of hypnosis on pain severity and interference with activities of daily living premastectomy and postmastectomy. They recruited forty patients who were randomly assigned to test or control group. Pain scores were evaluated at baseline, after clinical hypnosis, before surgery, one day after surgery and one week after surgery. The authors concluded that hypnosis gave reduced intensity of post-mastectomy pain, pain interfered less with patients’ daily activities and allowed for improved sleep and life enjoyment when compared to the group without intervention.
This finding does not correspond to the primary outcome of a RCT by Amraoui et al. [41]. The HYPNOSEIN RCT was a prospective clinical trial carried out over multiple centers in France [41]. One hundred fifty women who underwent breast cancer surgery were split randomly into hypnosis and control arms of the study. A hypnosis session was done in the anaesthetic room before surgery. The primary endpoint tested was assessment of pain reduction whereby hypnosis showed no improved pain score over the control group. Secondary targets were analysis of post-operative nausea and vomiting, fatigue, overall wellbeing and length of stay at postanesthesia care unit. Patients were assessed before discharge from post anesthesia care unit and at different points in the first thirty days of recovery. Secondary endpoints had positive outcomes in the hypnosis cohort when compared to the control group. The median length of stay at post-anesthesia care unit was also shorter in patients in the hypnosis study arm.
Hypnosis is a great tool to alleviate pain, fatigue and anxiety in breast cancer patients [41]. It prioritizes patients’ comfort, reduces emotional discomfort, enhances patient satisfaction and ameliorates quality of life [42]. Evidence is limited to this innovative technique yet results already point towards success and any opportunity to introduce or improve hypnosis as part of psychosocial therapy for breast cancer patients should not be overlooked.
Conclusion
The psychosocial techniques discussed ensure patient comfort, reduce emotional distress, enhance patient satisfaction and improve quality of life [42]. All interventions are non-pharmacological and easily accessible to both patients and clinicians. Efforts to introduce new psychosocial techniques should be driven forward in any Breast Care Unit to improve the patient’s experience in breast cancer treatment.
Acknowledgment
None.
Conflict of Interest
No conflict of interest.
References
- Feng Y, Mia Spezia, Shifeng Huang, Chengfu Yuan, Zongyue Zeng, et al. (2018) Breast cancer development and progression: Risk factors, cancer stem cells, signaling pathways, genomics, and molecular pathogenesis. Genes and Diseases 5(2): 77-106.
- Liu JK, Amy H Kaji, Katherine G Roth, Danielle M Hari, James J Yeh, et al. (2022) Determinants of Psychosocial Distress in Breast Cancer Patients at a Safety Net Hospital. Clinical breast cancer 22(1): 43-48.
- Bell K, Ristovski-Slijepcevic S (2013) Cancer Survivorship: Why Labels Matter. Journal of Clincial Oncology 31(4): 409-411.
- Lyman GH, Heather Greenlee, Kari Bohlke, Ting Bao, Angela M DeMichele, et al. (2018) Integrative Therapies During and After Breast Cancer Treatment: ASCO Endorsement of the SIO Clinical Practice Guideline. Journal of clinical oncology: official journal of the American Society of Clinical Oncology 36(25): 2647-2655.
- Zhang L, Xiaohong Liu, Fei Tong, Ran Zou, Wanglian Peng, et al. (2022) Cognitive behavioral therapy for anxiety and depression in cancer survivors: a meta-analysis. Sci Rep12(1):21466.
- Culbertson MG, Bennet K, Kelly CM, Sharp L, Kahir C (2020) The psychosocial determinants of quality of life in breast cancer survivors: a scoping review. BMC Cancer 20(1): 948.
- Jansen F, Van Zwieten V, Coupe V, Leemans CR, (2016) A Review on Cost-Effectiveness and Cost-Utility of Psychosocial Care in Cancer Patients. Asia-Pacific Journal of Oncology Nursing 3(2): 125-136.
- Gudenkauf LM, Ehlers SC (2018) Psychosocial interventions in breast cancer survivorship care. The Breast: Official Journal of the European Society of Mastology 38: 1-6.
- Hirschberg I, Seidel G, Strech D, Bastian H (2013) Evidence-based health information from the users' perspective - A qualitative analysis. BMC Health Services Research 13(1): 405.
- (2002) Active Citizenship Network, European Charter of Patients’ Rights, Presented in Brussels on 15 November.
- Elkin E, Valerie H Pocus, Alvin I Mushlin, Tessa Cigler, Coral L Atoria, et al. (2017) Facilitating informed decisions about breast cancer screening: development and evaluation of a web-based decision aid for women in their 40s. BMC Medical Informatics and Decision Making, 17(1): 29.
- Woloshin S, Schwartz LM, Black WC, Kramer BS (2012) Cancer screening campaigns - getting past uninformative persuasion. The New England journal of medicine 367(18): 1677-1679.
- Hersch J, Alexandra Barret, Jesse Jansen, Les Irwig, Kevin McGeechan, et al. (2015) Use of a decision aid including information on over detection to support informed choice about breast cancer screening: a randomised controlled trial. The Lancet 385(9978): 1642-1652.
- Pérez-Lacasta MJ, Montserrat Martínez-Alonso, Montse Garcia, Maria Sala, Lilisbeth Perestelo-Pérez, et al. (2019) Effect of information about the benefits and harms of mammography on women's decision making: The InforMa randomised controlled trial. PLoS One 14(3): e0214057.
- Fernández-Feito A, Canga-Gutiérrez C, Paz-Zulueta M (2021) A mixed-methods study to evaluate the acceptability of information leaflets for breast cancer screening. Journal of Clinical Nursing 30(11-12): 1760-1772.
- Pollard J, Rose H, Mullen R, Abbott N (2021) Breast Core Biopsy Information and Consent: Do we Prepare or do we Scare?. Journal of Patient Experience 8(58).
- Lee GK, Sheckter CC (2018) Breast Reconstruction Following Breast Cancer Treatment-2018. Journal of the American Medical Association 320(12): 1277-1278.
- Ter Stege JA, Leonie A E Woerdeman, Daniela EE Hahn, Martine A van Huizum, Frederieke H van Duijnhoven, et al. (2019) The impact of an online patient decision aid for women with breast cancer considering immediate breast reconstruction: study protocol of a multicenter randomized controlled trial. BMC Medial Informatics and Decision Making 19(1): 165.
- Sustersic M, Gauchet A, Foote A, Bosson J (2017) How best to use and evaluate Patient Information Leaflets given during a consultation: a systematic review of literature reviews. Health Expectations 20(4): 531-542.
- Sun H, Hualei Huang, Shengjun Ji, Xiaochen Chen, Yongqing Xu, et al. (2019) The Efficacy of Cognitive Behavioral Therapy to Treat Depression and Anxiety and Improve Quality of Life Among Early-Stage Breast Cancer Patients. Integrative cancer therapies Vol 18.
- Türk KE, Yilmaz M (2018) The Effect on Quality of Life and Body Image of Mastectomy Among Breast Cancer Survivors. European journal of breast health 14(4): 205-210.
- Park S, Yasuko Sato, Yuka Takita, Noriko Tamura, Akira Ninomiyaet al. (2020) Mindfulness-Based Cognitive Therapy for Psychological Distress, Fear of Cancer Recurrence, Fatigue, Spiritual Well-Being, and Quality of Life in Patients with Breast Cancer-A Randomized Controlled Trial. Journal of pain and symptom management 60(2): 381-389.
- Jelvehzadeh F, Dogaheh ER, Bernstein C, Shakiba S, Ranjbar H (2022) The effect of a group cognitive behavioral therapy on the quality of life and emotional disturbance of women with breast cancer. Supportive care in cancer 30(1): 305-312.
- Husak AJ, Bair MJ (2020) Chronic Pain and Sleep Disturbances: A Pragmatic Review of Their Relationships, Comorbidities, and Treatments. Pain medicine 21(6): 1142-1152.
- Ma Y, Daniel L Hall, Long H Ngo, Qingqing Liu, Paul A Bain, et al. (2021) Efficacy of cognitive behavioral therapy for insomnia in breast cancer: A meta-analysis. Sleep medicine reviews 55: 101376.
- Padron A, Christina S McCrae, Michael E Robinson, Lori B Waxenberg, Michael H Antoni, et al. (2022) Impacts of Cognitive Behavioral Therapy for Insomnia and Pain on Sleep in Women with Gynecologic Malignancies: A Randomized Controlled Trial. Behavioural sleep medicine 20(4): 460-476.
- Tatrow K, Montgomery GH (2006) Cognitive behavioral therapy techniques for distress and pain in breast cancer patients: a meta-analysis. Journal of behavioral medicine 29(1): 17-27.
- Moorthy A, Lowry D, Edgley C, Casey M, Buggy D (2022) Effect of perioperative cognitive behavioural therapy on chronic post-surgical pain among breast cancer patients with high pain catastrophizing characteristics: protocol for a double-blinded randomised controlled trial. Trials 23(1): 66.
- Akkol-Solakoglu S, Hevey D (2023) Internet-delivered cognitive behavioural therapy for depression and anxiety in breast cancer survivors: Results from a randomised controlled trial - PubMed (nih.gov). Pyschooncology 32(3): 446-456.
- Savard J, Ivers H, Savard MH, Morin CM (2014) Is a video-based cognitive behavioral therapy for insomnia as efficacious as a professionally administered treatment in breast cancer? Results of a randomized controlled trial - PubMed (nih.gov). Sleep 37(8): 1305-1314.
- Kaiser J, Joerg D, Miena A, Isa R, Hazal A, et al. (2019) Cognitive Performance and Psychological Distress in Breast Cancer Patients at Disease Onset. Frontiers in psychology 10: 2584.
- Montgomery GH, Schnur JB, Kravits K (2013) Hypnosis for cancer care: over 200 years young. CA: a cancer journal for clinicians 63(1): 31-44.
- Fabbro M, William Jacot, Marta Jarlier, Séverine Guiu, Véronique Dhondt, et al. (2023) Hypnosis on patients treated with adjuvant chemotherapy for breast cancer: A feasibility study. Cancer Reports 6(1): e1732.
- Kravits K (2013) Hypnosis: adjunct therapy for cancer pain management. Journal of the advanced practitioner in oncology 4(2): 83-88.
- Schnur JB, Guy H Montgomery, Michael N Hallquist, Alisan B Goldfarb, Jeffrey H Silverstein, et al. (2008) Anticipatory psychological distress in women scheduled for diagnostic and curative breast cancer surgery. International journal of behavioral medicine 15(1): 21-28.
- Montgomery GH, Dana H Bovbjerg, Julie B Schnur, Daniel David, Alisan Goldfarb, et al. (2007) A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery. Journal of the National Cancer Institute 99(17): 1304-1312.
- Berliere M, Nathan Piette 2, Marion Bernard 1, Camille Lacroix 1, Amandine Gerday, et al. (2021) Hypnosis Sedation Reduces the Duration of Different Side Effects of Cancer Treatments in Breast Cancer Patients Receiving Neoadjuvant Chemotherapy. Cancers 13(16): 4147.
- Potié A, Roelants F, Pospiech A, Momeni M, Watremetz C (2016) Hypnosis in the Perioperative Management of Breast Cancer Surgery: Clinical Benefits and Potential Implications. Anesthesiology research and practice.
- Bruce J, Thornton AJ, Powell R, Johnston M, Wells M, et al. (2014) Psychological, surgical, and sociodemographic predictors of pain outcomes after breast cancer surgery: A population-based cohort study. Pain 155(2): 232-243.
- Hernández DM, Arnoldo Téllez, Teresa Sánchez-Jáuregui, Cirilo H García, Manuel García-Solís, et al. (2022) Clinical Hypnosis for Pain Reduction in Breast Cancer Mastectomy: A Randomized Clinical Trial. The international journal of clinical and experimental hypnosis 70(1): 4-15.
- Amraoui J, Camille Pouliquen, Julien Fraisse, Jacques Dubourdieu, Sophie Rey Dit Guzer, et al. (2018) Effects of a Hypnosis Session Before General Anesthesia on Postoperative Outcomes in Patients Who Underwent Minor Breast Cancer Surgery: The HYPNOSEIN Randomized Clinical Trial. Jama Network Open 1(4): 181164.
- Sánchez-Jáuregui, T., Téllez, A., Juàrez-García, D., García, C.H. & García, F.E., 2019. Clinical Hypnosis and Music In Breast Biopsy:A Randomized Clinical Trial. The American journal of clinical hypnosis, 61(3), pp. 244-257.
-
Jessica Dowling* and Lara Rapa. The Role of Psychosocial Interventions In Breast Cancer Patients. Anaest & Sur Open Access J. 5(4): 2024. ASOAJ.MS.ID.000620.
-
Breast cancer, Preprocedural information, Cognitive behavioural therapy, Hypnosis, Cognitive behavioural therapy, Randomised controlled trial, Mindfulness-based intervention, Mindfulness-based cognitive therapy, Mindfulness-based stress reaction
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






