 Case Report
Case Report
Maxillary Reconstruction using Autologous Bone Graft: A Case Report
Lilian Cornejo Valdez1, Louis Hardan2,3, Nicolas Nassar3,4,5, Jose Manuel Rios Alcantara6, Horacio Islas Granillo7, Ana Josefina Monjaras Avila7, Sleman Alkhouri8, Souheir khafaja9, Faisal Alsaid10, Naji Kharouf11,12, Vanderlim Branco Camargo2,9,11*, and Carlos Enrique Cuevas-Suarez7
1Student of the bachelor’s degree in Dental Surgeon of the Academic Area of Dentistry of the Institute of Health Sciences of the Autonomous University of the State of Hidalgo; Pachuca 42039, México
2Department of Restorative and Esthetic Dentistry, Faculty of Dental Medicine, Saint-Joseph University of Beirut, Beirut, Lebanon
3Department of Digital Dentistry, AI, and Evolving Technologies, Faculty of Dental Medicine, Saint-Joseph University of Beirut, Beirut, Lebanon
4Department of Orthodontics, Faculty of Dental Medicine, Saint-Joseph University of Beirut, Beirut, Lebanon
5Craniofacial Research Laboratory, Faculty of Dental Medicine, Saint-Joseph University of Beirut, Beirut, Lebanon
6Dental Specialties Unit; SEDENA, México
7Dental Materials Laboratory, Academic Area of Dentistry, Autonomous University of Hidalgo State, San Agustín Tlaxiaca, Mexico
8Independent Researcher, Bismarckstr, Germany
9Department of Restorative Sciences, Faculty of Dentistry, Beirut Arab University, Beirut, Lebanon
10Esthetic and Prosthetic Dentistry Resident, Faculty of Dental Medicine, Saint-Joseph University of Beirut, Beirut, Lebanon
11Department of Biomaterials and Bioengineering, INSERM UMR_S 1121, University of Strasbourg, Strasbourg, France
12Department of Endodontics and Conservative Dentistry, Faculty of Dental Medicine, University of Strasbourg, Strasbourg, France
Vanderlim Branco Camargo, Department of Restorative and Esthetic Dentistry, Faculty of Dental Medicine, Saint-Joseph University of Beirut, Beirut, Lebanon
Received Date: June 28, 2025; Published Date: July 09, 2025
Abstract
The use of autologous ulna bone for the reconstruction of atrophic bone crest could be a viable resource to obtain cortico-cancellous bone graft blocks, since the extraction of this donor site is associated with low morbidity. the objective of this case report was to describe the technique used to achieve three-dimensional regeneration of the atrophic maxillary alveolar process with significant bone defects using an ulna autograft. A 70-yearold male patient, diagnosed with hypertension and controlled diabetes, presented with complete edentulism and a Cawood and Howell Class IV atrophic maxilla. It was decided to reconstruct the upper jaw using an anterior ulna autologous onlay bone graft, in order to place implants for their rehabilitation with implant-supported prosthesis. It began with a linear incision was made in the forearm to harvest two cortico-cancellous bone blocks, anatomical conformation was performed in the oral receptor bed by placing a collagen membrane to maintain the cancellous bone, which was not fully osseo integrated, complementing with bone xenograft. Finally, four implants are placed, two in each quadrant.
Keywords:Autograft; ulna; atrophic bone crest; elderly; implant-supported prosthesis; systemically compromised
Introduction
Bone volume deficit in completely edentulous patients creates both surgical and prosthetic challenges in implantology. Its pathophysiology involves a combination of metabolic factors—such as nutritional deficiencies, endocrine disorders, and associated osteopenias—and local factors, the most common being the absence of dental organs [1]. This absence causes bone resorption in the maxillary bone due to lack of intraosseous stimulation, affecting the proportions of medullary and cortical bone, with the latter showing less loss. Given this physiological process, identifying the resorption pattern affecting the maxillary and mandibular bones is crucial for adequate reconstruction. In the maxilla, resorption is centripetal, resulting in collapse, whereas in the mandible it is centrifugal [2].
Autologous bone graft surgery requires consideration of both donor site selection and the potential morbidity involved, as well as patient-specific comorbidities that may influence the procedure. of alveolar atrophy, a wide range of preprosthetic surgical techniques have been developed [3], including the use of autografts, allografts, and xenografts. These approaches have evolved into hybrid techniques such as onlay grafts, interposition with Le Fort I osteotomy, maxillary sinus augmentation, nasal floor grafting, application of morphogenetic proteins, microvascular grafts, dental implants, zygomatic implants, and osteogenic distraction [4]. In cases of unitary tooth loss or up to three to four teeth, it is possible to perform grafting techniques with intraoral donor sites such as chin, mandibular ramus, and maxillary tuberosity. Alternatively, in cases of total edentulous atrophic maxillary processes, the bone volume offered by these sites is insufficient for reconstruction. Thus, an extra-oral donor site that offers the option of complete maxillary reconstructions with enough bone to obtain the desired volume is required [5].
Both intraoral and extraoral bone grafting techniques present certain limitations and advantages worth considering. Harvesting grafts can lead to various complications, including postoperative pain, nerve injury, and scarring [5]. However, these risks are significantly reduced when the clinician possesses extensive surgical experience and anatomical knowledge. surgical anatomical knowledge. Autologous bone grafts offer the benefit of being rich in viable cellular components, delivering a sufficient volume of cortico-cancellous bone—an essential requirement for successful preprosthetic reconstruction [6]. When planning the construction of atrophic ridges for implant placement, it is critical to evaluate the extent and origin of bone loss. This ensures the formulation of an appropriate treatment plan to be able to increase both the heigh and the thickness of the alveolar process in the long-term [7].
Despite the numerous reported advantages of autografts, there is still limited evidence on the use of ulna bone as a donor site for intraoral ridge augmentation procedures [8,9]. Therefore, the main objective of this report is to describe a technique for regenerating the alveolar process in atrophic maxillae using ulna autograft in an outpatient setting for patients with systemic compromise, aiming for a successful prosthetic rehabilitation. Additionally, a review of the available evidence on the use of ulna grafts for reconstructing alveolar ridges is needed.
Case report
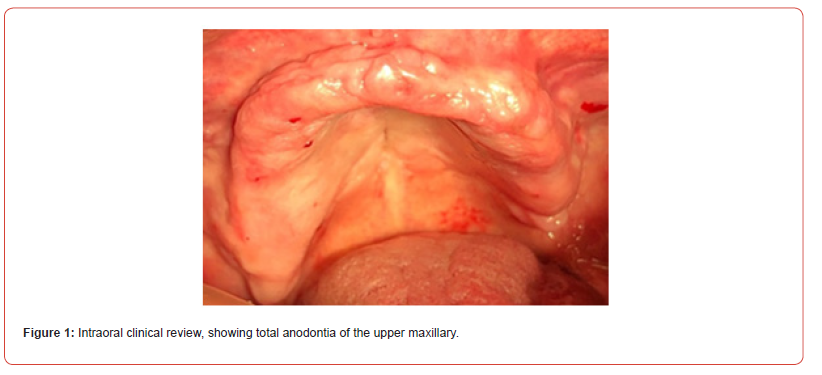
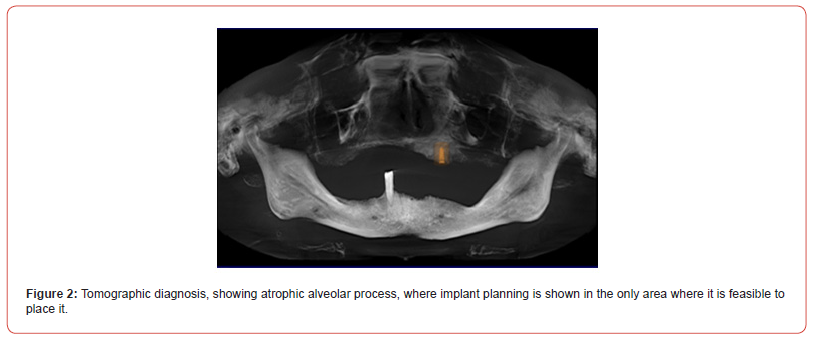
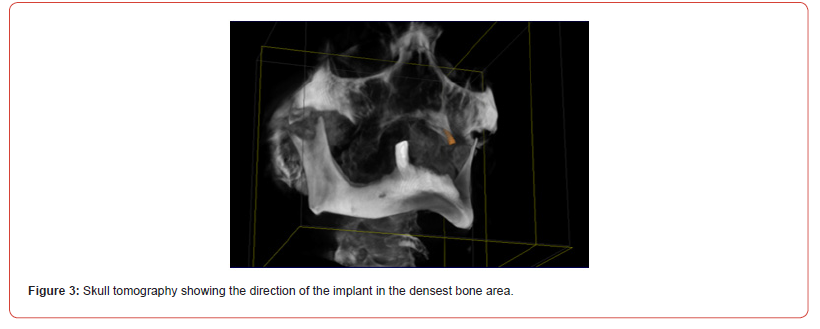
Type 2 diabetes, presented with the desire to regain the ability to eat through dental rehabilitation. Intraoral examination revealed total edentulism and a severely atrophic alveolar ridge, classified as Class IV according to Cawood and Howell [10] (Figure 1), with a clinically measured ridge thickness of approximately 3 mm It was decided to perform the reconstruction of the alveolar process with an autologous anterior ulna bone graft type onlay, in order to place implants for their rehabilitation in a second surgical stage. All steps of the procedure and possible associated risks were explained to the patient, and an informed written consent was granted.
Surgical Technique of Ulnar Autograft in the maxilla
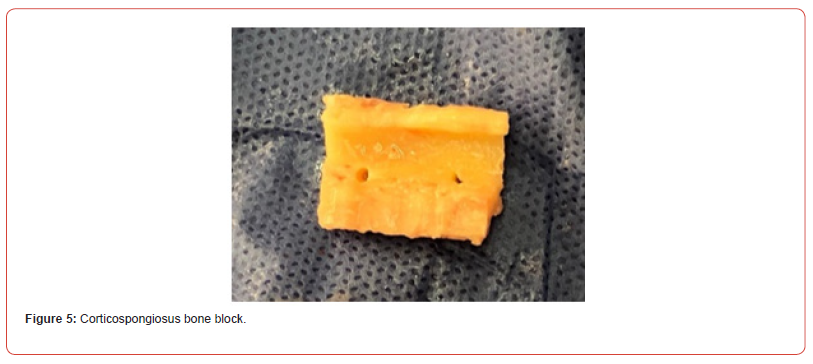
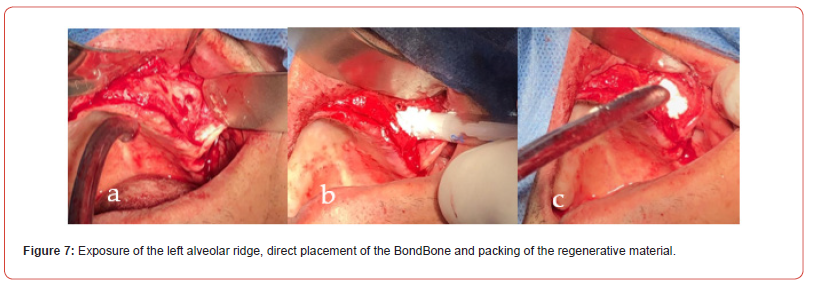
This reconstructive surgery was performed by a multidisciplinary team in an outpatient setting under local anesthesia. Four cartridges of 4% articaine (turbocaine, 4% articaine HCl, 1 : 100,000 epinephrine Aleaciones Dentales Zeyco, SA de C.) were administred throughout the maxilla and five cartridges of the same in the forearm region. A linear mucoperiosteal incision was made with a # 3 scalpel handle and a # 15 blade (B | BRAUN, Germany by Aesculap AG). Once the alveolar process was exposed, decortication of the vestibular cortex was performed, and hemostasis was achieved using gauze and bone wax (Ind and Com Brand, Ethicon). Subsequently, a linear approach to the forearm was made using a #3 scalpel handle with a #22 blade (BBRAUN AG, Germany) (Figure 4). Two blocks of cortico-spongy bone were harvested using a lowering piece and a long-stem carbide fissure bur under irrigation with physiological solution. A chisel and hammer were also employed during the process, yielding approximately 7 cc of graft material. The exposed forearm was sutured using simple continuous stitches with Vicryl #000 (Ind and Com Brand, Ethicon) (Figure 6). Cortical perforations were made to promote graft revascularization, and sharp edges of the bone blocks were smoothed under copious irrigation with sterile saline solution. In the surgical bed of the left maxillary quadrant, 0.5 cc of Bond Bone (SEVEN, Mis México) was applied due to extensive bone loss (Figure 7). Following this, the graft blocks were carefully positioned.
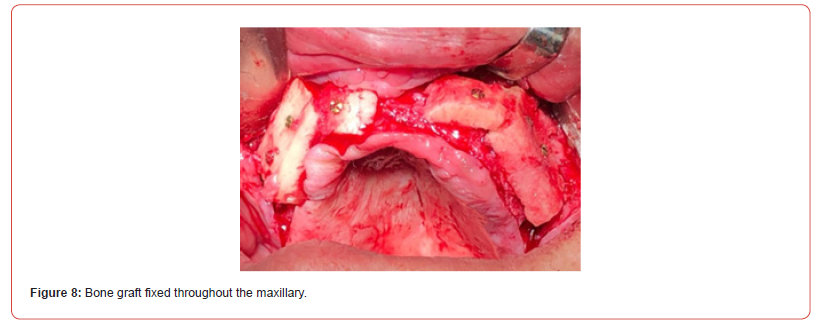
In both quadrants of the upper jaw, the graft blocks were secured using screws (SEVEN, Mis México) measuring 1.5 mm in diameter and 10 mm in length, oriented buccally along the alveolar process. Once the blocks were fixed, a cancellous graft was placed to achieve anatomical conformation of the alveolar ridge. A 0.3 mm collagen membrane (SEVEN, Mis México) was then positioned as both a shaper and stabilizer for the cancellous bone. To minimize graft exposure, the buccal mucosa was elevated and periosteal tension reduced. The area was subsequently sutured using simple stitches with Vicryl #000 (Ind and Com Brand, Ethicon) (Figures 8 & 9).



The surgery was completed successfully without postoperative complications. The patient was provided with comprehensive postoperative instructions, including avoidance of sun exposure and refraining from tooth brushing during the first 24 hours following surgery. Additional recommendations included avoiding bending, physical exertion, greasy, spicy, or hot foods, as well as alcoholic beverages and tobacco use. Antibiotic therapy was initiated with amoxicillin 300 mg. For pain management, sulindac was prescribed every eight hours for three days, or as needed. A follow-up appointment was scheduled one week after the procedure.
Implant Surgical Procedure
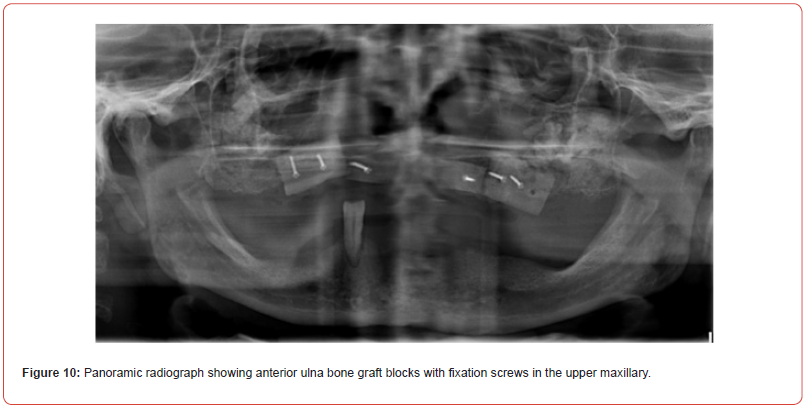
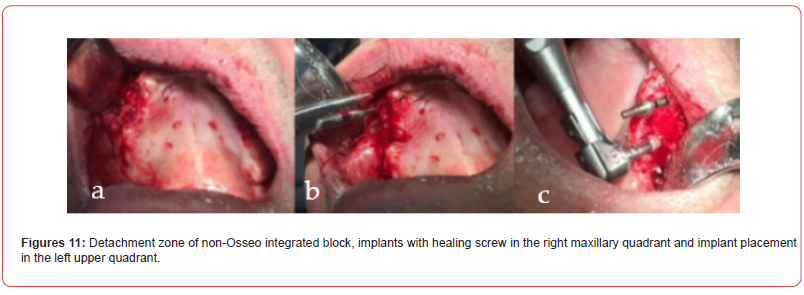
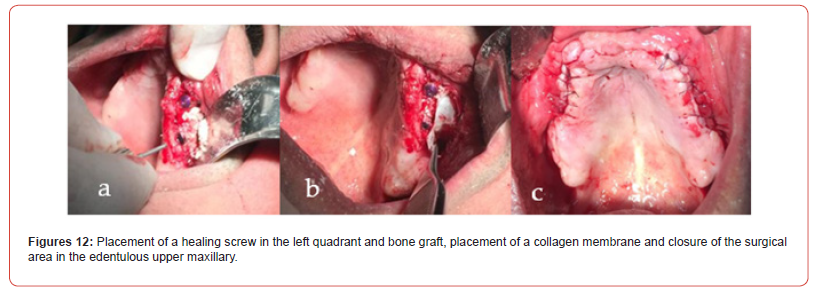
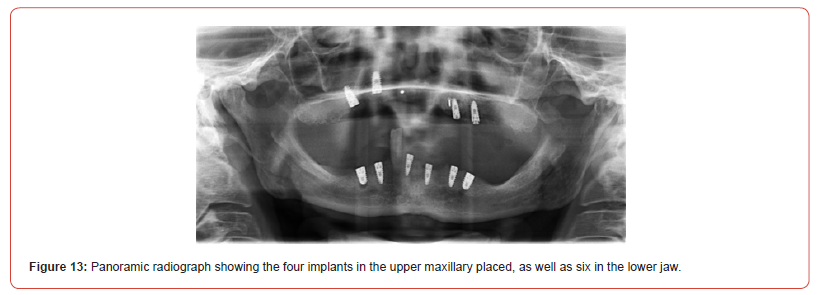
Four and a half months after graft placement (Figure 10), the patient was scheduled to place his implants. For this procedure, the entire maxillary region was anesthetized with The patient was anesthetized with seven cartridges of 4% articaine. A linear incision was made using a #3 scalpel handle and a #15 blade (BBRAUN, Germany by Aesculap AG), exposing the grafted bone blocks and allowing removal of the fixation screws. During this procedure, partial detachment of one graft was observed due to failed osseointegration, necessitating its removal. To address this, fixation screws were repositioned into areas with successfully integrated bone (Figure 11). The surgical bed was irrigated with 12% chlorhexidine (Lacer, Spain) using a micromotor. Four implants were placed in the maxilla and six in the mandible. Healing screws were fixed using a submerged approach (Figure 12). Due to residual bone loss, a bone xenograft and a collagen membrane (SEVEN, Mis México), measuring 0.20 mm × 0.30 mm, were placed. The surgical site was closed using simple continuous sutures with Vicryl #000 (Ind and Com Brand, Ethicon) (Figure 12). Postoperative instructions were provided, and a computed tomography scan was scheduled to confirm implant positioning (Figure 13). The patient was prescribed amoxicillin 300 mg every 8 hours for 7 days and sulindac every 8 hours for 3 days as needed for pain control. An appointment was scheduled for impression taking and placement of the implant-supported prosthesis.
Discussion
In geriatric implantology, treatment planning must be highly individualized, as anatomical and physiological differences become more pronounced with age [11]. Three-dimensional cone beam computed tomography is a highly effective diagnostic and planning tool in minimally invasive implant surgery. From a surgical perspective, two critical factors must be considered when operating on elderly patients: the ongoing effort to minimize morbidity, and the increased prevalence of coexisting medical risk factors in this population [12]. Current literature identifies bone autografts as one of the most reliable and successful techniques for maxillary ridge reconstruction [13]. However, donor site morbidity has prompted many surgeons to seek the most efficient and least traumatic options, including the calvaria, tibia, rib, olecranon, anterior iliac crest, mandibular ramus, and symphysis [4,14,15]. Sjöström et al. highlight that an onlay-type ulna bone graft allows for harvesting a substantial volume of cortical and cancellous bone, making it suitable for reconstructing the atrophic edentulous maxilla and providing sufficient volume for predictable implant placement [4].
In geriatric implantology, treatment planning must be highly individualized, as anatomical and physiological differences become more pronounced with age [11]. Three-dimensional cone beam computed tomography is a highly effective diagnostic and planning tool in minimally invasive implant surgery. From a surgical perspective, two critical factors must be considered when operating on elderly patients: the ongoing effort to minimize morbidity, and the increased prevalence of coexisting medical risk factors in this population [12]. Current literature identifies bone autografts as one of the most reliable and successful techniques for maxillary ridge reconstruction [13]. However, donor site morbidity has prompted many surgeons to seek the most efficient and least traumatic options, including the calvaria, tibia, rib, olecranon, anterior iliac crest, mandibular ramus, and symphysis [4,14,15]. Sjöström et al. highlight that an onlay-type ulna bone graft allows for harvesting a substantial volume of cortical and cancellous bone, making it suitable for reconstructing the atrophic edentulous maxilla and providing sufficient volume for predictable implant placement [4]. This donor site is associated with minimal complications and yields highly satisfactory outcomes for both clinicians and patients.”
In this clinical case report, an autologous bone graft was utilized-recognized as the gold standard for alveolar ridge augmentation due to its intrinsic osteogenic potential [16] and consistently high survival rate, regardless of donor site [17]. Ulna bone from the forearm was selected as the graft source, given its viability in providing cortico-cancellous bone conducive to optimal regeneration and early implant placement. This approach was particularly suitable considering the patient’s advanced age and systemic conditions.
In systemically compromised individuals, complications can be more severe; therefore, a thoroughly updated clinical history is essential to formulate an appropriate treatment plan for outpatient management [18]. In this case, a lack of integration was observed in a portion of the graft placed in the right maxillary quadrant, which necessitated removal during implant placement to proceed with the surgical protocol.
Several factors may have contributed to the partial failure of graft osseointegration, including the patient’s systemic condition and associated medications. Intraoperative management may also play a role, particularly the molding of the graft at the recipient site, which can prolong surgical time and require greater manipulation to ensure full coverage and attachment. Moreover, age-related vascular decline and a reduced population of osteoprogenitor cells at the donor site may limit cortical bone revascularization, increasing the risk of delayed healing or graft failure [19].
The implants were initially allowed to heal with a submerged approach for six weeks, followed by an additional six weeks of osseointegration prior to loading. This protocol was essential for achieving aesthetic and functional success, as bone contour, continuity, and volume restoration are key determinants of favorable implant outcomes [19].
The postoperative period was uneventful—no impairment of forearm muscle motility or nerve function was observed. The scar did not affect the patient’s aesthetics and was outweighed by the substantial improvement in quality of life, especially dietary rehabilitation, which holds direct relevance for managing systemic conditions.
However, further clinical research is needed to evaluate the performance of various donor sites for ridge augmentation. In reviewing the literature specific to ulna graft use for maxillary defects, only three clinical reports were identified [20-22], underscoring the need for more robust evidence.
In cases where oral aesthetics carry greater significance, such as anterior sector implants following substantial bone loss, the ulna graft offers promising advantages. These include minimizing soft tissue resections and avoiding sensory disturbances to adjacent teeth, which are more common with intraoral harvesting. Although scarring and potential delays in forearm muscle motility may occur, the use of an extraoral donor site reduces complications such as facial neurosensory alterations.
Implant failure may also be closely linked to surgical technique, anatomical placement, and patient factors such as age, nutritional status, smoking, and alcohol consumption. These variables should be carefully considered in treatment planning to mitigate procedural risks.
Conclusion
Autografts offer significant advantages for the reconstruction of maxillary bone defects. These procedures can often be performed on an outpatient basis under local anesthesia in the dental chair, allowing the surgeon to carry them out successfully and efficiently. Therefore, the choice of donor site is typically left to the surgeon’s discretion. Based on the clinical outcomes presented in this case report, it can be concluded that the anterior ulna autograft is a viable option for harvesting autogenous bone to reconstruct medium- to large-sized alveolar bone defects.
Data Availability Statement
The data presented in this study are available upon reasonable request from the author (C.E.C.-S.).
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Khan SN, Cammisa Jr FP, Sandhu HS, Diwan AD, Girardi FP, et al. (2005) The Biology of Bone Grafting. J Am Acad Orthop Surg 13(1): 77-86.
- Villaseñor JP, Jurado DV (2014) Reconstruction of the Maxillary Alveolar Process with Autologous Iliac Crest Graft. Rev Odontológica Mex 18: 263-270.
- Cawood JI, Howell RA (1991) Reconstructive Preprosthetic Surgery. I. Anatomical Considerations. Int J Oral Maxillofac Surg 20(2): 75-82.
- Sjöström M, Sennerby L, Nilson H, Lundgren S (2007) Reconstruction of the Atrophic Edentulous Maxilla with Free Iliac Crest Grafts and Implants: A 3-Year Report of a Prospective Clinical Study. Clin Implant Dent Relat Res 9(1): 46-59.
- Stenport VF, Rtorp A, Thor A (2011) Onlay and Inlay Bone Grafts with Platelet-Rich Plasma: Histologic Evaluations from Human Biopsies. J. Oral Maxillofac. Surg 69(4): 1079-1085.
- Beirne JC, Barry HJ, Brady FA, Morris VB (1996) Donor Site Morbidity of the Anterior Iliac Crest Following Cancellous Bone Harvest. Int J Oral Maxillofac. Surg 25(4): 268-271.
- Bloomquist DS, Feldman GR (1980) The Posterior Ilium as a Donor Site for Maxillo-Facial Bone Grafting. J Maxillofac Surg 8(1): 60-64.
- Garcia-Júnior IR, Souza FÁ, Figueiredo AAS, Poli PP, Benetti F, et al. (2018) Maxillary Alveolar Ridge Atrophy Reconstructed with Autogenous Bone Graft Harvested from the Proximal Ulna. J Craniofac Surg 29(8): 2304-2306.
- Hjørting-Hansen E (2002) Bone Grafting to the Jaws with Special Reference to Reconstructive Preprosthetic Surgery. Mund Kiefer Gesichtschirurgie 6(1): 6-14.
- Cawood JI, Howell RA (1988) A Classification of the Edentulous Jaws. Int J Oral Maxillofac Surg 17(4): 232-236.
- Issrani R, Ammanagi R, Keluskar V (2012) Geriatric Dentistry–Meet the Need. Gerodontology 29(2): e1-e5.
- Schimmel M, Müller F, Suter V, Buser D (2017) Implants for Elderly Patients. Periodontol 73(1): 228-240.
- Zhao R, Yang R, Cooper PR, Khurshid Z, Shavandi A, et al. (2021) Bone Grafts and Substitutes in Dentistry: A Review of Current Trends and Developments. Molecules 26(10): 3007.
- Rossi AC, Freire AR, Perussi MR, Caria PHF, Prado FB (2012) Use of Homologous Bone Grafts in Maxillary Sinus Elevation. Int J Odontostomatol 6(1): 19-26.
- Stern A, Barzani G (2015) Autogenous Bone Harvest for Implant Reconstruction. Dent Clin North Am 59(2): 409-420.
- Goyal Mittal N, Gupta GK, Singhal M (2015) Ridge Augmentation in Implant Dentistry. J Int Clin Dent Res Organ 7: 94.
- Titsinides S, Agrogiannis G, Karatzas T (2019) Bone Grafting Materials in Dentoalveolar Reconstruction: A Comprehensive Review. Jpn Dent Sci Rev 55(1): 26-32.
- Meloto CB, Rizzatti-Barbosa CM, Gomes SGF, Custodio W (2008) Dental Practice Implications of Systemic Diseases Affecting the Elderly: A Literature Review. Braz J Oral Sci 7(27).
- Devorah Schwartz-Arad, Liran Levin (2005) Intraoral Autogenous Block Onlay Bone Grafting for Extensive Reconstruction of Atrophic Maxillary Alveolar Ridges. J Periodontol 76(4): 636-641.
- Madsen MJ, Mauffrey C, Bowles N, Seligson D (2011) Using the Proximal Ulna as a Novel Site for Autogenous Bone Graft Harvesting. J Oral Maxillofac Surg 69(7): 1930-1933.
- Bracker K, Trout N (2000) Use of a Free Cortical Ulnar Autograft Following En Bloc Resection of a Mandibular Tumor. J Am Anim Hosp Assoc 36(1): 76-79.
- Garcia-Júnior IR, Souza FÁ, Figueiredo AAS, Poli PP, Benetti F, et al. (2018) Maxillary Alveolar Ridge Atrophy Reconstructed with Autogenous Bone Graft Harvested from the Proximal Ulna. J Craniofac Surg 29(8): 2304-2306.
-
Lilian Cornejo Valdez, Louis Hardan, Nicolas Nassar, Jose Manuel Rios Alcantara, Horacio Islas Granillo. Maxillary Reconstruction using Autologous Bone Graft: A Case Report. Anaest & Sur Open Access J. 6(2): 2025. ASOAJ.MS.ID.000634.
-
Autograft; ulna; atrophic bone crest; elderly; implant-supported prosthesis; systemically compromised; iris publishers; iris publisher’s group
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






