 Research Article
Research Article
Management of Recurrent Uncomplicated Diverticulitis in the Recent Era-Is Surgery Warranted? A Single Irish Centre Experience and Literature Review
Mahmoud M Salama1*, Ahmed Salama2, Caroline Drumm1, Wael Shabo3 and Mohamed Salama3
1St James Hospital, Dublin, Ireland
2Beaumont Hospital, Dublin, Ireland
3Our Lady of Lourdes Hospital, Drogheda, Ireland
Mahmoud M Salama, St James Hospital, Dublin, Ireland
Received Date:September 25, 2024; Published Date: December 12, 2024
Abstract
Introduction: Colonic Diverticulitis presents a growing healthcare challenge. The management of recurrent acute uncomplicated diverticulitis (RAUD) is controversial and debatable. The indication for surgery after recovery of RAUD is still unclear given the variability of real-life clinical practice.
Aims: To analyze and evaluate the management strategies and their outcomes of both complicated and uncomplicated diverticulitis.
Methods: We conducted a retrospective analysis of 882 cases between 2018 and 2022 and reviewed patient demographics, treatment
modalities, and recurrence rates. Management approaches included conservative, surgical, and interventional radiology-based interventions.
Results: Of the 882 cases, 19.6% were complicated, predominantly managed conservatively. Recurrence rates were 6.6%, with most cases
uncomplicated. Further interventions were required in 5.9% of recurrent cases. Elective surgery for uncomplicated diverticulitis was notably absent.
Complication rates post-surgical interventions were high.
Conclusion: Our study underscores the importance of evidence-based, patient-centered approaches in diverticulitis management. By
challenging traditional dogma and embracing contemporary insights, we advocate for tailored strategies that prioritize patient outcomes and quality
of life. Collaborative research endeavors are essential for informed decision-making and continuous improvement in diverticulitis care.
Keywords:Acute diverticulitis; Management; Recurrence; Surgery; Hartmann’s; Complications; Conservative Treatments; Non-Operative management
Introduction
Colonic Diverticulitis, a prevalent gastrointestinal condition characterized by inflammation of diverticula within the colon, poses a significant healthcare burden worldwide [1,2]. With an aging population and lifestyle factors such as diet and physical inactivity contributing to its increasing prevalence, diverticulitis has emerged as a prominent concern in modern healthcare systems [3-5].
The management of diverticulitis, particularly in cases of recurrence, has undergone substantial evolution over the past few decades. Historically, surgical intervention was often the cornerstone of management, with guidelines recommending elective resection after one or two episodes of acute uncomplicated diverticulitis (AUD) [6]. This approach, rooted in outdated perceptions of disease progression and surgical outcomes, reflected a belief in the inevitability of recurrent attacks and the potential for severe complications with each subsequent episode.
However, advancements in diagnostic modalities, such as computed tomography (CT) imaging, coupled with a deeper understanding of disease pathogenesis, have challenged traditional paradigms in diverticulitis management. Contemporary evidence suggests that recurrent episodes of diverticulitis may not necessarily herald a worsening disease course or mandate prophylactic surgery. Rather, there is growing recognition of the heterogeneity of diverticulitis presentations and the need for personalized, patient- centred approaches to management. The indications for surgery are unclear and post-operative complications remain high. The real-life clinical practice patterns are unknown.
Aims
To analyse and evaluate the management strategies and their outcomes of both complicated and uncomplicated diverticulitis. We aim that our study contributes to the evolving discourse on diverticulitis management by conducting a comprehensive retrospective analysis of clinical practices and outcomes. By examining a large cohort of diverticulitis cases, encompassing both complicated and uncomplicated presentations, we seek to elucidate current management trends and their implications for recurrent disease.
Methods
This study was a retrospective review conducted at our hospital, examining cases of diverticulitis diagnosed via computed tomography (CT) between January 2018 and December 2022.
Data Collection
Patient records were reviewed and data collected on demographics, clinical presentation, diagnostic findings, treatment modalities, and outcomes. Specific data points included age, gender, classification of diverticulitis (complicated vs uncomplicated), treatment approach (conservative management, Hartmann’s procedure, resection with anastomosis, laparoscopic washout, and interventional radiology drainage), recurrence rates, and any subsequent interventions.
Inclusion and Exclusion Criteria
Patients included in the study were those with a confirmed diagnosis of diverticulitis based on CT imaging. Both complicated and uncomplicated cases were included. Patients with incomplete medical records or those who were treated for other gastrointestinal conditions were excluded from the study.
Statistical Analysis
Descriptive statistics were used to summarize the data. Continuous variables were presented as means with standard deviations, and categorical variables were presented as frequencies and percentages.
Management Protocols
Patients with uncomplicated diverticulitis were typically managed
with conservative measures, including antibiotics and dietary
modifications. In cases of complicated diverticulitis, the initial approach
depended on the severity and specific complications: - All
patients were treated as inpatients. For this study, complicated
cases defined as diverticulitis with complication such as abscess,
perforation, stricture or obstruction.
Conservative Management: Included antibiotics, bowel rest,
and close monitoring.
• Hartmann’s Procedure (HP): Performed in patients with severe
complications such as bowel obstruction or free perforation
with peritonitis.
• Resection and Anastomosis (R&A): Considered for select
patients based on the extent of disease, patient stability and
surgeon’s preference.
• Laparoscopic Washout: Used in select cases with perforations
or abscesses not amenable to interventional radiology
drainage.
• Interventional Radiology (IR) Drainage: Preferred for
drainable abscesses to avoid surgery.
Follow-Up
Patients were followed up through outpatient records to monitor for recurrence of diverticulitis, subsequent interventions, and overall outcomes. Recurrent episodes were categorized as either uncomplicated or complicated, and the treatment approach for each recurrence was documented.
Results
During the study period, a total of 882 (F:M, 480:402) cases of diverticulitis were reviewed, comprising both complicated and uncomplicated cases. Among these cases, 173 (19.6%) were classified as complicated diverticulitis, while the majority, 709 (80.4%), were categorized as uncomplicated.
Management of uncomplicated cases:
All uncomplicated cases were treated conservatively.
Management of Complicated Cases:
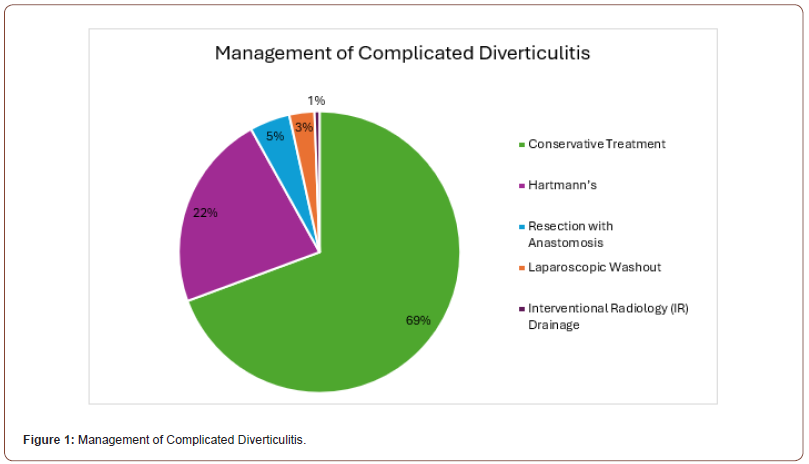
120 cases underwent conservative management in our cohort of complicated cases. 39 cases underwent HP, 8 cases R&A, 5 cases laparoscopic washout and 1 case required IR drainage (Figure 1).
Complications in resection and anastomotic group:
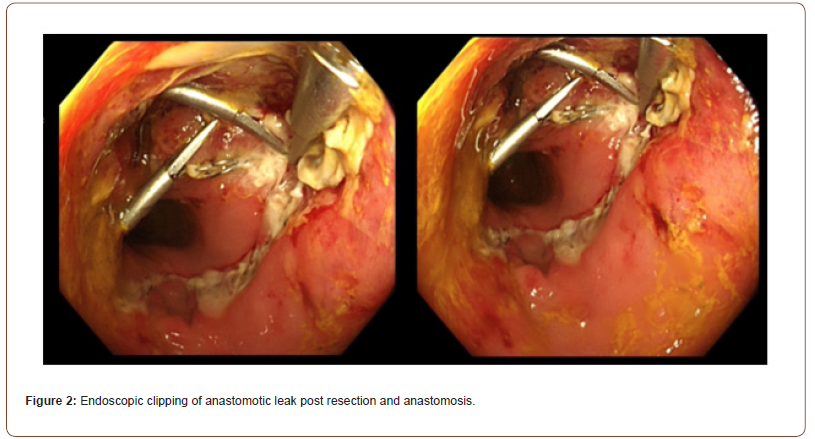
Anastomotic leak was noted in 3 cases, two of which were treated with endoscopic clips (Figure 2) and the third one underwent re-laparotomy, anastomotic resection and end colostomy formation.
Complications of Hartmann’s group:
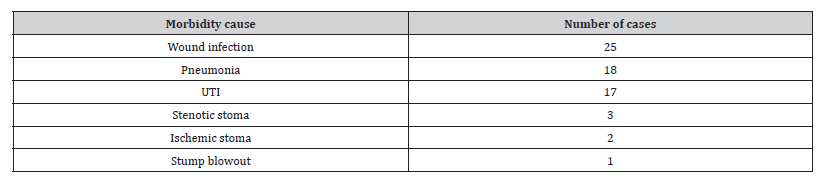
A total of 39 patients with complicated diverticulitis underwent HP during our study period. Of these, there was 2 cases of mortality within 30 days post-operatively (Table 1). A variety of non-fatal complications were noted post operatively including wound infection in 25 cases, pneumonia in 18, urinary tract infection (UTI) in 17, stoma stenosis in 3 cases, ischaemic of the stoma in 2 and stump blowout in 1 case (Figure 2).
Table 1:Morbidity following Hartman’s Procedure.
Recurrence of Attacks:
Total Recurrent Cases: 58 (6.6% of total cases), 10 of them
recurred more than twice.
Uncomplicated Recurrence: 42 cases (72.4% of recurrent
cases)
Complicated Recurrence: 16 cases (27.6% of recurrent
cases)
Complicated since first episode: 12 cases (75% of complicated
recurrence cases)
Initially uncomplicated, then complicated: 4 cases (25%
of complicated recurrence cases).
Further Interventions for Recurrent Cases:
• IR Drainage: 2 cases (2.9% of recurrent cases)
• Laparoscopic Washout: 2 cases (2.9% of recurrent cases)
Elective Surgery:
• No elective surgery was performed for uncomplicated diverticulitis during the study period.
Laparoscopic washout group:
For Perforated Diverticulitis:
Patient 1: A 37-year-old female with Hinchey stage 3 diverticulitis
underwent laparoscopic washout.
Patient 2: A 62-year-old female with abscess and perforation,
underwent laparoscopic washout followed by IR drainage
twice.
Patient 3: A 57-year-old male laparoscopic washout for
right-sided perforated diverticulitis
Patient 4: A 56-year-old male with Hinchey stage 3 diverticulitis,
had diagnostic laparoscopy, washout, and drain placement.
For Abscess Management: not amenable to IR
• Patient 5: A 49-year-old female with perisigmoid abscess, not
amenable for IR drainage, underwent laparoscopic washout.
• Patient 6: A 63-year-old female with a large abscess and perforation,
initially treated with laparoscopic washout but eventually
underwent Hartmann’s procedure.
• Patient 7: A 52-year-old male with a large abscess not amenable
for IR drainage, underwent laparoscopic washout and
drain placement.
All patients were treated with antibiotics and as inpatients during the acute attack.
Discussion
The incidence of diverticular disease has increased in the last decades and it represents a challenge to the health care system. The optimal management of uncomplicated diverticulitis generates a considerable debate. Its management has undergone substantial evolution, reflecting advancements in diagnostic modalities and a nuanced understanding of disease pathogenesis [1,7-9].
Historically, surgical intervention was considered a cornerstone, often recommended after one or two episodes of acute diverticulitis [10,11].
One century ago, Telling advocated surgery as a treatment of diverticulitis in the British Journal of Surgery [7,8]. The guideline from the American Society of Colon and Rectal Surgeons (ASCRS) in 2000 recommended elective resection after one or two episodes of acute uncomplicated diverticulitis (AUD). This approach is rooted in outdated perceptions of disease progression and surgical outcomes. In 1975 Parks et al assumed an increasing risk of complication and a reduction in the response rate to conservative therapy after the second attack of AUD. This has increasingly come under scrutiny in light of contemporary evidence.
Our study, encompassing 882 cases of diverticulitis, offers valuable insights into current management practices and their align ment with evolving evidence. Of our 173 complicated diverticulitis cases, 120 were managed conservatively (69.4%), 4 of which failed the conservative approach and required intervention. Even minor complications such as abscess or sealed perforation with extra-luminal air can be managed conservatively. This departure from the once-prevalent surgical approach underscores a paradigm shift towards a more nuanced, patient-centred approach.
Contrary to historical beliefs, our findings suggest that recurrent episodes of diverticulitis do not always signify a worsening disease course or necessitate prophylactic surgery [9]. In fact, our data revealed that 72.4% of recurrent cases were uncomplicated, while 27.6% were complicated. Within the complicated recurrence cases, we found that 75% were complicated since the first episode, while 25% were initially uncomplicated but later became complicated. This nuanced understanding challenges the traditional notion that recurrent episodes inevitably escalate in severity [10]. Moreover, the high success rates observed with non-operative management underscore the efficacy of conservative approaches in resolving acute uncomplicated episodes. The absence of elective surgery for AUD during the study period reflects a growing acknowledgment of the limitations of a one-size-fits-all approach. Instead, contemporary guidelines advocate for personalized decision-making, considering factors beyond age or number of attacks [11]. This individualized approach prioritizes patient outcomes and quality of life, steering away from the traditional surgical dogma that once prevailed.
2 decades ago, the ASCRS recommended an individualized management post recovery from AUD. Current guidelines from ASCRS and AGA recommended against routine surgery and advised elective surgery after recovery from AUD should be individualized and not based on age or number of attacks and careful risk vs benefits assessment is essential [12].
The most recent guidelines in the management of AUD from the ACP published in 2022 advocate less aggressive management of AUD. Currently there is a broad consensus that acute surgery is not indicated in patients with AUD [12,13]. All the patients admitted with AUD are managed conservatively in our hospital.
Beyond surgical considerations, our study sheds light on the nuanced role of interventions in the context of recurrent diverticulitis. While emergency surgeries such as Hartmann’s procedure remain indispensable for severe complications, elective colectomy does not confer a significant reduction in disease burden. This underscores the need for a nuanced risk-benefit assessment and a departure from blanket recommendations for prophylactic surgery.
Furthermore, our findings underscore the importance of ongoing research to refine and optimize therapeutic strategies in diverticulitis management. The debate surrounding surgical techniques, particularly R&A vs HP, open vs laparoscopic vs robotic highlights the need for comparative effectiveness studies to delineate optimal approaches.
Patients with AUD can be managed conservatively for several reasons. Firstly, the risk for complicated recurrence requiring emergency surgery after successful recovery from AUD managed medically is low [13,14]. Studies have demonstrated that the longterm recurrence rates for uncomplicated diverticulitis range from 13% to 20%, with a subsequent need for emergency surgery ranging from 6% to 7% [13,15]. Interestingly, complicated diverticulitis requiring surgery is more common during the first episode than during recurrent episodes [16]. Additionally, surgical intervention may not always resolve all abdominal symptoms and may even result in life-threatening complications. Recurrence rates after sigmoid colectomy for uncomplicated diverticulitis range approximately from 3% to 13%, suggesting that performing elective colectomy may not significantly decrease the burden of diverticulitis in the population [17-19]. Non-operative management of AUD has proven to be successful in more than 95% of patients, emphasizing its efficacy as a treatment option [20,21]. Recent evidence has also revealed that younger patients have similar rates of recurrence and subsequent need for colectomy as older patients [22]. Overall, the majority of patients with AUD will not experience further episodes.
Regarding the operative approaches, emergency surgery is mainly reserved to severe complications as bowel obstruction or free perforation with peritonitis. (NICE, 2019, Sartelli et al 2020).
Primary R&A with or without proximal diversion is reserved for haemodynamically stable patients (weak recommendation based on low quality evidence, 2B), [8,23]. Despite emerging data supporting primary anastomosis with diversion, this approach is not widely used (NSQIP study analysed patient undergoing emergent colectomy for diverticulitis from 2012 to 2016 found that only 7.6% underwent primary anastomosis with proximal diversion) [24].
HP is preferred option for unstable patients with shock, acidosis, acute or chronic organ failure or old patient with poor sphincteric function (Strong recommendation based on low quality evidence, 2B), [8,23]
Despite HP is the procedure of choice, it remains associated with high morbidity and mortality due to the preoperative instability of the patient selected for the procedure (age, frail, co-morbid population-Sartelli et al, 2020, NELA 2021)
Laparoscopic peritoneal lavage is performed in selected patients with general peritonitis and it is not considered as a first line treatment (Weak recommendation based on high quality evidence, 2A), [8]. It is associated with higher risks of reoperation and approximately 3 times greater risk of persistent peritonitis, intra-abdominal abscess and the need for emergency surgery.
The Scandinavian diverticulitis (SCANDIV) and LOLA trials – (Laparoscopic lavage of the ladies’ trial) both published in 2015 failed to demonstrate superiority of laparoscopic lavage to sigmoid colectomy for acute diverticulitis [25,26].
Laparoscopic lavage nowadays is not the option of choice with most surgeons and its adoption remains low. The 2020 ASCRS guidelines recommend against the use of laparoscopic lavage in feculent peritonitis and preferred colectomy over lavage in purulent peritonitis [24].
Evaluating the patient related factors and not number of previous episodes of diverticulitis in planning sigmoid resection was suggested (Weak recommendations based on very low quality of Evidence, 2D), [8].
In high-risk patients such as immunocompromised patients, elective sigmoid colectomy after successful conservative treatment is recommended (Weak recommendation based on low quality of evidence, 2D), [8].
All the patients in our study, including AUD cases were treated as in patient with a full course of antibiotics. However, there are a few recent studies showed that antibiotics neither prevent complications and recurrences nor do they reduce symptoms or length of stay. (RCT, The AVOD study, DIABOLO Trial) [24,27,28].
Limitations
While our study provides valuable insights into diverticulitis management, several limitations should be noted. Conducted at a single centre, the findings may not be generalizable to other settings. The retrospective design introduces biases from relying on existing medical records. The relatively limited number of cases, despite including 882, affects statistical power and precision. The heterogeneity of cases adds complexity to analysis and interpretation. Additionally, variations in treatment approaches among clinicians may introduce variability and confounding factors. Despite these limitations, our study contributes to the literature on diverticulitis management and underscores the need for further research to provide more robust evidence.
Conclusion
In summary, the management of diverticulitis has evolved significantly, moving away from the historical emphasis on surgical intervention towards a more conservative, patient-centred approach. Our study, which reviewed 882 cases of diverticulitis, highlights this shift, demonstrating that a substantial proportion of complicated cases can be effectively managed conservatively. This approach challenges traditional beliefs about the necessity of prophylactic surgery after recurrent episodes and underscores the importance of individualized risk assessment. The high success rates of non-operative management and the absence of elective surgeries for uncomplicated diverticulitis during our study period emphasize the efficacy of conservative treatments. Furthermore, our findings advocate for personalized decision-making that considers factors beyond just age or the number of attacks, aiming to optimize patient outcomes and quality of life. Despite the limitations of it being a single-centre and retrospective study, these insights contribute to the ongoing discourse on diverticulitis management, emphasizing the need for further research to refine and optimize therapeutic strategies. As we continue to navigate the complexities of diverticulitis, it is crucial to embrace evidence-based practices that prioritize patient-centred care and adapt to the evolving understanding of the disease.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Strate LL, Morris AM (2019) Epidemiology, Pathophysiology, and Treatment of Diverticulitis. Gastroenterology 156(5): 1282-1298.e1.
- Weizman AV, Nguyen GC (2011) Diverticular disease: epidemiology and management. Can J Gastroenterol 25(7): 385-389.
- Kruis W, Germer CT, Böhm S, Dumoulin FL, Frieling T, et al. (2022) German guideline diverticular disease/diverticulitis: Part II: Conservative, interventional and surgical management. United European Gastroenterol J 10(9): 940-957.
- Dahl C, Crichton M, Jenkins J, Nucera R, Mahoney S, et al. (2018) Evidence for Dietary Fibre Modification in the Recovery and Prevention of Reoccurrence of Acute, Uncomplicated Diverticulitis: A Systematic Literature Review. Nutrients 10(2): 137.
- Ma W, Jovani M, Nguyen LH, Tabung FK, Song M, et al. (2020) Association Between Inflammatory Diets, Circulating Markers of Inflammation, and Risk of Diverticulitis. Clin Gastroenterol Hepatol 18(10): 2279-2286.e3.
- Rafferty J, Shellito P, Hyman NH, Buie WD (2006) Practice parameters for sigmoid diverticulitis. Dis Colon Rectum 49(7): 939-944.
- Chabok A, Thorisson A, Nikberg M, Schultz JK, Sallinen V (2021) Changing Paradigms in the Management of Acute Uncomplicated Diverticulitis. Scand J Surg 110(2): 180-186.
- Telling WHM, Gruner OC (1916) Acquired diverticula, diverticulitis, and peridiverticulities of the large intestine. British Journal of Surgery 4(15): 468-530.
- Parks T (1969) Natural history of diverticular disease of the colon. A review of 521 cases. Br Med J 4(5684): 639-642.
- Stollman NH, Raskin JB (1999) Diagnosis and management of diverticular disease of the colon in adults. Official journal of the American College of Gastroenterology| ACG 94(11): 3110-3121.
- Hall J, Hardiman K, Lee S, Lightner A, Stocchi L, et al. (2020) The American Society of Colon and Rectal Surgeons Clinical Practice Guidelines for the Treatment of Left-Sided Colonic Diverticulitis. Dis Colon Rectum 63(6): 728-747.
- Nally DM, Kavanagh DO (2019) Current Controversies in the Management of Diverticulitis: A Review. Dig Surg 36(3): 195-205.
- Campana JP, Mentz RE, González Salazar E, González M, Moya Rocabado G, et al. (2023) Long-term outcomes and risk factors for diverticulitis recurrence after a successful laparoscopic peritoneal lavage in Hinchey III peritonitis. International Journal of Colorectal Disease 38(1): 18.
- Chapman JR, Dozois EJ, Wolff BG, Gullerud RE, Larson DR (2006) Diverticulitis: a progressive disease? Do multiple recurrences predict less favorable outcomes? Ann Surg 243(6): 876-830; discussion 880-3.
- Bolkenstein HE, Van Dijk ST, Consten ECJ, Heggelman BGF, Hoeks CMA, et al. (2019) Conservative Treatment in Diverticulitis Patients with Pericolic Extraluminal Air and the Role of Antibiotic Treatment. J Gastrointest Surg 23(11): 2269-2276.
- Pittet O, Kotzampassakis N, Schmidt S, Denys A, Demartines N, et al. (2009) Recurrent Left Colonic Diverticulitis Episodes: More Severe Than the Initial Diverticulitis? World Journal of Surgery 33(3): 547-552.
- Waser A, Balaphas A, Uhe I, Toso C, Buchs NC, et al. (2023) Incidence of diverticulitis recurrence after sigmoid colectomy: a retrospective cohort study from a tertiary center and systematic review. Int J Colorectal Dis 38(1): 157.
- Waser A, Balaphas A, Uhe I, Toso C, Buchs NC, et al. (2023) Incidence of diverticulitis recurrence after sigmoid colectomy: a retrospective cohort study from a tertiary center and systematic review. International Journal of Colorectal Disease 38(1):157.
- Longchamp G, Abbassi Z, Meyer J, Toso C, Buchs NC, et al. (2021) Surgical resection does not avoid the risk of diverticulitis recurrence-a systematic review of risk factors. Int J Colorectal Dis 36(2): 227-237.
- Bolkenstein HE, Van Dijk ST, Consten ECJ, Heggelman BGF, Hoeks CMA, et al. (2019) Conservative Treatment in Diverticulitis Patients with Pericolic Extraluminal Air and the Role of Antibiotic Treatment. Journal of Gastrointestinal Surgery 23(11): 2269-2276.
- Agnes AL, Agnes A, Di Grezia M, Giambusso M, Savia E, et al. (2024) Management of acute diverticulitis in Stage 0-IIb: indications and risk factors for failure of conservative treatment in a series of 187 patients. Scientific Reports 14(1): 1501.
- Santacroce G, Lenti MV, Abruzzese GM, Alunno G, Di Terlizzi F, et al. (2024) Clinical outcomes of diverticular disease in young adults: results from a tertiary referral center. Front Med (Lausanne) 11: 1363548.
- Rook JM, Dworsky JQ, Curran T, Banerjee S, Kwaan MR (2021) Elective surgical management of diverticulitis. Curr Probl Surg 58(5): 100876.
- Khan A, Hawkins AT (2021) Challenging Surgical Dogma: Controversies in Diverticulitis. Surg Clin North Am 101(6): 967-980.
- Azhar N, Johanssen A, Sundström T, Folkesson J, Wallon C, et al. (2021) Laparoscopic Lavage vs Primary Resection for Acute Perforated Diverticulitis: Long-term Outcomes from the Scandinavian Diverticulitis (SCANDIV) Randomized Clinical Trial. JAMA Surg 156(2): 121-127.
- Vennix S, Musters GD, Mulder IM, Swank HA, Consten EC, et al. (2015) Laparoscopic peritoneal lavage or sigmoidectomy for perforated diverticulitis with purulent peritonitis: a multicentre, parallel-group, randomised, open-label trial. The Lancet 386(10000): 1269-1277.
- Elisei W, Tursi A (2016) Recent advances in the treatment of colonic diverticular disease and prevention of acute diverticulitis. Ann Gastroenterol 29(1): 24-32.
- Buchs NC, Konrad-Mugnier B, Jannot AS, Poletti PA, Ambrosetti P, et al. (2013) Assessment of recurrence and complications following uncomplicated diverticulitis. Br J Surg 100(7): 976-979; discussion 9.
-
Mahmoud M Salama*, Ahmed Salama, Caroline Drumm, Wael Shabo and Mohamed Salama. Management of Recurrent Uncomplicated Diverticulitis in the Recent Era-Is Surgery Warranted? A Single Irish Centre Experience and Literature Review. Anaest & Sur Open Access J. 6(1): 2024. ASOAJ.MS.ID.000627.
-
Mater Dei Hospital, Hypertension, Diabetes Mellitus, Gastro-Oesophageal Reflux Disease, Ischaemic Heart Disease, Chronic Obstructive Pulmonary Disease, Body Mass Index, Standard Deviation
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






