 Review Article
Review Article
An Uncommon Association of Cerebral Venous Thrombosis and Meningitis in a Postpartum Patient with Chronic Otitis: A Case Report
Chikhi Brahim*, Aarjouni Youssef, Hmadat Iyass, Mohamed Rabi Andaloussi and Jaafari Abdelhamid
Department of Anesthesia and Intensive Care, Military Hospital Mohammed V, Faculty of Medicine and Pharmacy of Rabat, Mohammed V University, Rabat, Morocco
Chikhi Brahim, Department of Anesthesia and Intensive Care, Military Hospital Mohammed V, Faculty of Medicine and Pharmacy of Rabat, Mohammed V University,12040, Rabat, Morocco
Received Date: February 20, 2025; Published Date: February 25, 2025
Abstract
Cerebral venous thrombosis (CVT) is a rare but potentially serious condition, often associated with pregnancy and postpartum, and frequently overlooked due to its variable clinical presentation. This case report describes an unusual association of CVT with meningitis in a 23-year-old postpartum woman with chronic otitis. The patient presented with fever, meningeal signs, and purulent otorrhea, alongside an inflammatory syndrome and negative cerebrospinal fluid cultures, which led to an initial diagnosis of acute mastoiditis complicated by meningitis. Despite initial antibiotic therapy, the patient developed altered consciousness and a generalized seizure, prompting further imaging that revealed a septic venous thrombosis. Contrast-enhanced brain CT and venous-phase imaging confirmed the diagnosis of septic CVT. The patient was managed with combined antibiotic therapy and anticoagulation, resulting in clinical improvement. Surgical treatment, including mastoidectomy, was performed with no complications. This case highlights the importance of considering CVT in the differential diagnosis of complicated otogenic infections, underscoring the need for early imaging and combined medical and surgical management.
Keywords: Cerebral Venous Thrombosis; Mastoiditis Meningitis; Chronic Otitis; Thrombosis Treatment; Antibiotic Therapy
Introduction
Cerebral thrombophlebitis is a rare but potentially severe condition if not treated appropriately or in a timely manner. Cerebral venous thromboses (CVT) account for less than 1% of strokes. Although the diagnosis should often be considered, it is sometimes delayed due to its highly variable and sometimes insidious presentation [1]. The incidence is difficult to determine but is estimated at five cases per 1,000,000 per year. CVT can occur at any age, with a significant peak in young women, related to the predisposing role of estrogen-progestin contraceptives, pregnancy, and the postpartum period. This case report describes an unusual association of cerebral venous thrombosis with meningitis in a patient with chronic otitis one month postpartum.
Patient and Observation
A 23-year-old female patient, one-month post-partum with a history of chronic left otitis evolving for six weeks, treated with third-generation cephalosporin after the failure of initial antibiotic therapy with amoxicillin/clavulanic acid, presented to the emergency department with fever, meningeal syndrome (headaches, vomiting, photophobia), and purulent otorrhea.
Clinical examination revealed a febrile patient (39.1°C), conscious, well-oriented in time and space, with equal and reactive pupils, meningeal stiffness without focal neurological signs or signs of intracranial hypertension. The examination also found hypoacusis with tympanic perforation on otoscopy of the left ear and no oculomotor paralysis. The patient was hemodynamically and respiratorily stable, with blood pressure at 121/69 mmHg, a heart rate of 95 bpm, oxygen saturation at 98%, and a respiratory rate of 20 cycles/min.
Biological tests revealed an inflammatory syndrome (C-reactive protein at 330 mg/L, procalcitonin at 10.22 ng/mL, leukocytosis at 18.5 G/L, including 14.4 G/L neutrophils, fibrinogen at 7 g/L). Hemostasis tests, renal, and hepatic functions were normal (activated partial thromboplastin time: 39 sec, Quick time: 92%, creatinine clearance > 90 mL/min, ASAT: 24 IU/L, ALAT: 12 IU/L, total bilirubin: 4 mg/L)..
Lumbar puncture suggested a partially treated bacterial meningitis since the patient was already under antibiotic therapy (clear cerebrospinal fluid, mixed cellular formula with 200 leukocytes/mm³ including 45% lymphocytes and 55% neutrophils, elevated protein level at 0.92 g/L, and normal glucose levels).
A brain CT scan with and without contrast injection showed mastoid cell opacification with destruction of the left ossicular chain, erosion of the tympanic tegmen and antrum, and facial canal lysis at the tympanic portion. The venous-phase acquisition ruled out cerebral venous thrombosis. The diagnosis of acute mastoiditis complicated by meningitis was suspected.
The patient was treated with third-generation cephalosporin (100 mg/kg/24h) and was scheduled for mastoidectomy after antibiotic control of the meningitis. Cerebrospinal fluid culture and blood cultures were negative. Inflammatory parameters continued to rise (CRP at 370 mg/L, procalcitonin at 11.38 ng/ mL, leukocytosis at 19.9 G/L). A bacterial culture of the otorrhea identified Pseudomonas aeruginosa sensitive to Meropenem and Amikacin.
Antibiotic therapy was adjusted accordingly (Meropenem 6 g/ day in three doses, Amikacin 2 g/day). The patient became apyretic on the third day, and inflammatory markers declined by the fifth day (CRP at 72 mg/L, procalcitonin at 3.5 ng/mL, leukocytosis at 11.5 G/L). However, on the tenth day, the patient experienced altered consciousness (GCS at 13), agitation, and a generalized tonic-clonic seizure, which resolved after an intravenous dose of 2 mg midazolam.
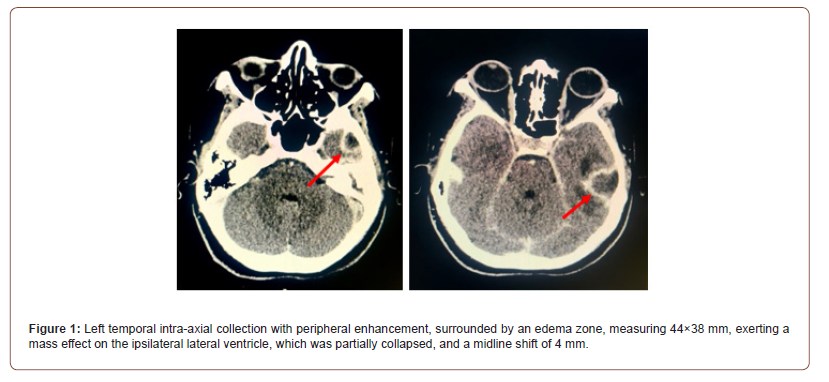
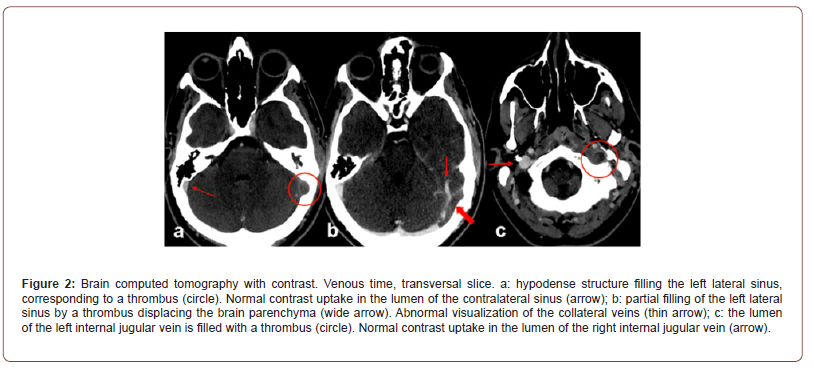
The patient was transferred to the ICU. A contrast-enhanced brain CT scan revealed a well-defined left temporal intra-axial collection with peripheral enhancement, surrounded by an edema zone, measuring 44×38 mm, exerting a mass effect on the ipsilateral lateral ventricle, which was partially collapsed, and a midline shift of 4 mm (Figure 1). There was also a lack of opacification of the left sigmoid and transverse sinuses, extending to the ipsilateral internal jugular vein, corresponding to septic venous thrombosis (Figure 2).
Anticoagulant therapy with therapeutic-dose low molecular weight heparin (LMWH) was initiated. The combination of antibiotic therapy and anticoagulation resulted in clinical and biological improvement: the patient remained apyretic, without otorrhea, or focal neurological signs, or seizures, and inflammatory markers normalized.
Surgical treatment was performed the following week, including mastoidectomy and aspiration of the abscess without complications. Oral anticoagulation replaced LMWH five days postoperatively. The patient was transferred to the ENT department for follow-up and imaging control.
Discussion
Otogenic septic thrombosis of the lateral sinus is a complication of mastoiditis, primarily described in children [2–5]. Adult mastoiditis has a low incidence (about 1 case per 100,000 inhabitants per year), with complications occurring in 50% of cases, half of which are intracranial. Otogenic septic thrombosis of the lateral sinus accounts for 3% of all complications [4]. Other possible cerebro-meningeal complications include meningitis, meningoencephalitis, cerebral empyema, and intracranial abscess, while extracranial complications include labyrinthitis and peripheral facial paralysis [2,5].
Mastoid infection spreads to the adjacent lateral sinus either directly or via small veins [2,6]. Thrombosis may be promoted by coagulase-producing bacteria, such as Fusobacterium species [2]. In our case, Pseudomonas aeruginosa was identified. Septic emboli can cause bacteremia, potentially leading to generalized sepsis, similar to Lemierre’s syndrome (internal jugular vein thrombosis secondary to an oropharyngeal infection) [2].
There are no specific clinical signs of otogenic cerebral venous thrombosis; only brain imaging differentiates it from other cerebro-meningeal complications [3,5,6]. In pediatric cases, a frequent nonspecific sign is abducens nerve paralysis (VI), related to intracranial hypertension secondary to hydrocephalus from impaired venous drainage [2].
Early imaging, particularly CT venography or MRI, is essential for preoperative management [3,5,6]. Untreated, the natural course of lateral sinus thrombosis may lead to hydrocephalus if recanalization fails [2].
Management is both medical and surgical, combining infection eradication through antibiotic therapy, otologic surgery, and anticoagulation for thrombotic complications [3-7]. The minimum duration of antibiotic therapy is two weeks [5]. Anticoagulation remains debated, especially in children, due to concerns about septic embolism and intracranial hemorrhage [2,6]. However, a recent study in children showed that well-conducted LMWH therapy did not increase bleeding or infection risks [4]. The American Heart Association/American Stroke Association recommended in 2011 curative LMWH followed by oral anticoagulation for 3–6 months in CVT with transient risk factors [7].
Surgical options include conservative mastoidectomy, as chosen in our case, or more radical approaches involving sinus exposure, thrombectomy, and internal jugular vein ligation [2,4,6].
Conclusion
CVT diagnosis remains challenging due to its clinical variability. Imaging, particularly CT and MRI, plays a crucial role in diagnosis, enabling early etiological investigation, which determines prognosis and specific treatment.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- Stam J (2005) Thrombosis of the cerebral veins and sinuses. N Engl J Med 352(17): 1791-1798.
- Francois M (2005 Complications des otites moyennes aiguës et chroniquesComplications of acute and chronic otitis media. EMC Oto-rhino-laryngologie 2(1): 92-106.
- Sitton MS, Chun R (2012) Pediatric otogenic lateral sinus thrombosis: role of anticoagulation and surgery. Int J Pediatr Otorhinolaryngol 76(3): 428-432.
- Ropposch T, Nemetz U, Braun EM, Lackner A, Walch C (2012) Low mole- cular weight heparin therapy in pediatric otogenic sigmoid sinus thrombosis: a safe treatment option? Int J Pediatr Otorhinolaryngol 76(7): 1023-1026.
- Palma S, Bovo R, Benatti A, Aimoni C, Rosignoli M, et al. (2013) Mastoiditis in adults: a 19-year retrospective study. Eur Arch Otorhinolaryngol 271(5): 925-931.
- Seven H, Ozbal AE, Turgut S (2004) Management of otogenic lateral sinus thrombosis. Am J Otolaryngol 25(5): 329-333.
- Saposnik G, Barinagarrementeria F, Brown RD, Bushnell CD, Cucchiara B, et al. (2011) A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42: 1158-1192.
-
Chikhi Brahim*, Aarjouni Youssef, Hmadat Iyass, Mohamed Rabi Andaloussi and Jaafari Abdelhamid. An Uncommon Association of Cerebral Venous Thrombosis and Meningitis in a Postpartum Patient with Chronic Otitis: A Case Report. Anaest & Sur Open Access J. 6(1): 2025. ASOAJ.MS.ID.000630.
-
Cleft Lip, Cleft Palate, Intravenous Fluids, Repair surgery, Congenital syndrome, ear infections, Anaesthetists
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






