 Mini Review
Mini Review
Additively Manufactured Implant Applications in Orthopedic Surgery
Efe Savran1, Semir M Negash1, Nazmi Bülent Alp2 and Fatih Karpat1*
1Department of Mechanical Engineering, Faculty of Engineering, Bursa Uludag University, Türkiye
2Medical Park Hospital, Bursa, Turkey
Faith Karpat, Department of Mechanical Engineering, Faculty of Engineering, Bursa Uludag University, Türkiye
Received Date:May 16, 2024; Published Date:May 22, 2024
Abstract
Additive Manufacturing (AM) has revolutionized surgery with its ability to enhance precision and customize treatment of patients. By utilizing this technology, surgeons can create optimized implants and easily predefine surgical interventions to highly enhance the surgical outcomes and minimize risks. With the material variation enriching the applications of AM, ongoing clinical trials largely aim to validate advancements involving custom-designed implants to pave the way for their widespread adoption in medical practice. In this mini-review, orthopedic surgical implant studies with AM methodology conducted between 2020 and 2024 were examined. The importance of AM technology in the rapidly growing orthopedic surgical treatments was emphasized. The role of materials and the associated challenges along with the trending remedies were explained. Concept of patient-specific design method and finite element analysis approach that enables the virtual analysis and prediction of implant properties were also presented. Finally, clinical studies were examined to reveal the reactions of implant designs under real-time conditions.
Keywords:Additive Manufacturing; Bio-materials; Orthopedic Implants; Finite Element Analysis; Patient Specific Treatments
Introduction
The human body is capable of self-renewal and self-healing as a routine replacement of malfunctioning and old cells or as a recovery from an injury causing damage. Nevertheless, under certain situations these natural strategies fail to achieve satisfactory results that enable the return of organs to their normal duty. In such situations several medical intervention strategies are thought to support the natural process. Considering the skeletal system, in cases where replacement is required due to aging or complete failure or after the occurrence of situations such as trauma, cancer removal, infection or other forms of excessive damages orthopedic surgeries are usually undertaken as a part of the treatment process. Such treatments in most cases involve fixation or even the replacement of section of the skeleton with artificial implants. Ideally the implants need to be bio-compatible, strong enough but with minimal stress shielding effect and with appropriate surface morphology.
Moreover, depending on the purpose the implants can be designed as a permanent or temporary inserts for which suitable biodegradability, osteoconduction and osteoinduction properties are expected [1]. It is also important that the production and surgical fixation of these implants to be feasible and cost effective. To achieve these requirements, it is critical to identify an appropriate production method and material combination for enhanced implant designs and efficient clinical implementation. In this regard, this mini-review provides an overview of the applications of additively manufactured implants for orthopedic surgical treatments. Orthopedic surgical implant studies with AM methodology, conducted between 2020 and 2024, were examined in terms of materials, optimal design, virtual simulation and clinical applications.
Additive Manufacturing Technology
Aiming to enhance the efficiency of orthopedic surgical treatments, recently there has been huge research shift from traditional graft-based bone treatment studies to additively manufactured implants. Like in many other sectors, AM has shown very promising results in orthopedic applications also by reducing the known lengthy processing steps and lead time needed to provide treatment for orthopedic patients. Among all, AM highly enables patient specific treatments through a pre-production analysis of implants that are designed based on unique patients’ specific conditions [2]. Besides to the accurate and reproducible fabrication of implants, AM also eases the incorporation of additives including drugs, cells or any other forms of cues that are needed to facilitate the treatment.
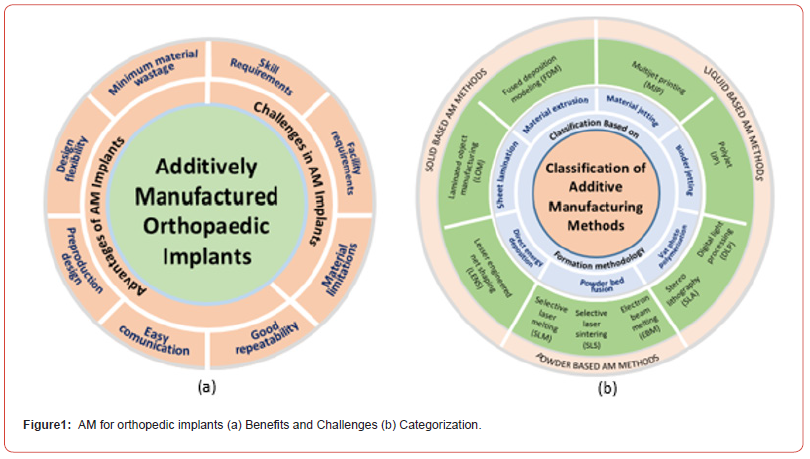
Depending on the treatment requirements, several AM methods [3] have been investigated in recent studies (Figure 1b). The purpose of the implant, its corresponding design and type of material to be used are the most crucial factors when it comes to selecting the appropriate AM method. Once the AM method is set, the printing conditions also need to be properly planned to get the best results with minimum deviations as compared to designed implants. For instance, the strength requirement of an implant whose purpose is to permanently support the body and a temporary one that is less prone to high pressure is not on the same level. This indicates that surgical sites also play a big role in defining not only the geometry but also the strength requirements. Understanding such constraints is important as it indicates the performance limits of the various AM methods that provide different level of strength for the same amount of implant volume.
Powder and liquid based AM methods are more integrated and compact as compared to Extrusion Based (EB) methods which are more sensitive and prone to inter-layer failures [4]. Similarly, with regards to geometric features such as pore size, shape and porosity EB methods provide the least control and perfection. However, when it comes to printing that involves cells or drugs EB methods take the upper hand.
Despite the mechanism of printing and post processing differences, orthopedic surgical procedures involving additively manufactured implants mostly begin by understanding and modeling the patient’s condition. Primarily, an implant that can satisfy the geometric requirement is designed according to scanned images retrieved by radiographers. In light to the condition of the patient, further studies are performed to refine the implant design followed by prototype production. Once the medical personnel approve modifications, a final implant is produced and surgical operations are performed after making the necessary post processing steps on the implants [5].
Materials
Decades long researches on artificial substitutes for defective bone sections have shown recently very promising results, especially with the enhancement of multi material processing methods. Conventionally a single material of either metal, polymer or ceramics have been used to produce implants putting certain limitations directly associated with the material properties. For a considerably longtime metals have been the most widely used bio-materials due to their excellent load bearing ability. However, they generally lack biological activeness and exhibit slow or no degradation, which makes using them for applications that require temporary insertion cumbersome as multiple surgery become inevitable. Their higher strength also comes with stress shielding effects that might cause implant or fixation failure [6].
In order to overcome the stiffness issue of metal implants and to reduce weight, polymeric implants have also been investigated. They are easier to produce and their properties can also be controlled over a wider range. Nevertheless, polymers generally suffer from low strength and exhibit rapid or irregular degradation. Furthermore, despite their good biological signaling and cell adhesion properties they are also susceptible to microbial contamination, particularly in cases where natural polymers are used which has increased the use of antimicrobial strategies as a remedy [7].
Likewise, implants of ceramic origin have been confirmed in several studies to exhibit bone like behaviors. In fact, ceramic materials constitute large portion of native bone and obviously an integration with a likely material is expected to ease biological activities. However, when it comes to implant integrity, they are more of fragile with poor resistance to shearing or tensile stresses [8].
To overcome the drawbacks of these materials, combined use in the form of powder mixing, fiber reinforcing, coating or painting have become the most common trends recently. For instance, in polymeric or ceramic based implants metals are usually added in the form of dispersed filler powders to improve strength [9]. Meanwhile, metals in addition to alloying preferably take coatings of other material classes to improve their surface properties [10]. One of the biggest advantages of using multi material designs for implants is the possibility of tailoring the material property to meet the requirements of a specific case. Theoretically, there can be hundreds of such combinations except literature indicates the superiority of certain materials. Titanium (Ti) in the form of Ti6Al4V alloy is for example widely used because of its corrosion resistance, non-toxicity and high bio-compatibility properties as compared to other metals [11]. On the other hand, Hydroxyapatite (HAp) has been repeatedly reported as one of the best performing ceramic materials especially when used in the form of nanoparticle additive to enhance properties of other base material classes [12]. On the contrary, mostly polymers take the matrix form for another nanoparticle or fibrous material to bind and improve the strength issues they suffer [13]. Additionally, polymers in the form of hydrogels offer the best medium for evenly mixing of additives like drugs, cues or even cells for cases like bio-ink based printing [14].
Applications of Additive Manufacturing
In the application section of surgical implants created by AM method, the benefits provided by patient-specific designs, clinical applications and studies conducted with the finite element method used for prediction purposes were examined.
Patient-Specific Implant Design
Obtaining surgical implants using traditional methods may be insufficient in terms of patient satisfaction. Structural differences in patients and case differences make it difficult to use the same implant design. Implant designs made specifically for the patient make the application and usage processes much easier and enable more successful results to be achieved. In recent years, as the AM method has become widespread and its design limitations have been reduced, the design, production and post-processing of implants have become much easier. Among the studies on patient-specific implant design, Arshad et al. [15] state that the success of end osseous implants depends on bone loss in the implant area. A titanium subperiosteal implant, specially designed and obtained by AM, was installed in a patient who had a history of previous implant failures. The implant, designed specifically for the patient, eliminates the need for bone filling and provides functional recovery in a single surgical intervention. Balamurugan and Selvakumar [16] emphasize that traditional methods in dental implant production are inadequate in terms of patient mouth condition, prosthesis reliability, and comfort. For this reason, they focused on the necessity of patient-specific prostheses and the difficulties experienced in the production of these prostheses. It is emphasized that patient-specific implant applications should be checked for a certain period of time with the help of computeraided design and analysis methods. Patient-specific designs that can withstand difficult conditions with the methods specified in the dental implant formation process can yield positive results. Matute et al. [17] proposed a special implant solution with the help of AM for a patient in need of cranial protection. The models created with polymethylmethacrylate (PMMA) and polyethyleneether- ketone (PEEK) materials were evaluated mechanically by finite element analysis. The results of the study showed that both materials offered similar responses. Considering that PMMA is a cheaper material than PEEK, it would be preferred with sufficient bio-mechanical safety. Danielli et al. [18] focused on patient-specific acetabular and hemipelvis implants. They aimed to determine the mechanical behavior of the titanium implant obtained by the AM method both experimentally and in a virtual environment using the finite element analysis method. The results of the study suggest that the modulus of elasticity in implants with thin thickness should be changed depending on model scaling. Rana et al. [19] emphasize in their study that stress shielding is a serious challenge in total hip arthroplasty. It is stated that patient-specific, porous implant structures suitable for additive manufacturing are a solution to this problem. Computed tomography and finite element analysis were used for implant design and optimization with heterogeneous porosity. As a result of the optimization study, stress shielding was significantly reduced and an implant design with high structural reliability was obtained.
Finite Element Analysis
It is a fact that surgical implants are of high importance for health. For the application to be successful, the design process can be supported with virtual methods to gain insight into real usage conditions. Thanks to the virtual results obtained, the most appropriate design is created and patient satisfaction is maximized. Finite element analysis is an analysis method frequently used in implant designs, among other fields. With a finite element model created with sufficient accuracy, time and cost savings can be achieved, and surgical interventions can be performed successfully. Among the studies conducted on finite element analysis of implants, Ciklacandir et al. [20] have described an implant design process that includes obtaining radiological images with different imaging methods, printing of bone morphology, and finite element analysis. While Stereolithography (STL) and Selective Laser Sintering (SLS) were used as AM methods, 3Matic software was used for editing the virtual model obtained from tomography. The resulting virtual model was analyzed with the finite element method and the stress distribution was examined. Virtual analysis results were highly accurate with real values. Ouldyerou et al. [21] emphasize that stress shielding occurs in solid titanium implant models and will cause structure loss. For this reason, implant models with two different porosity ratios were examined under different loading conditions, on a healthy and osteoporotic bone. According to the results of finite element analysis, the implant structure with high porosity has reached a higher stress value and the strain values in osteoporotic bone tissue are higher than in healthy bone tissue. Haque et al. [22] studied the determination of the optimal number of fixation points and the distance between points for cranial implants. By integrating the finite element analysis method, the optimal specific properties of the implant were determined. The results of the study stated that symmetrical fixation points reduced subsidence. Vautrin et al. [23] examined the determination of the fatigue life of porous titanium implants fabricated by AM method with the help of the finite element method. Mechanical tests were performed on additively manufactured titanium samples to establish a connection between the endurance limit and failure under cyclic loading, and a finite element model was subsequently developed to predict this result. The developed model was compared with experimental results and made available for fatigue life prediction. Ma et al. [24] emphasize that patient-specific implant designs can easily be made real through AM. In the study, implant models with different porosity ratios were created and stress, strain and deformation were examined using the finite element method. In this way, the elasticity modulus of the humerus bone was approximately determined. The study showed that designing models with a porous structure can reduce hardness, reduce stress shielding, increase stability, and extend life. Savran et al. [25] used the finite element method to determine the structural reliability of the lattice-structured implant design they created to prevent and alleviate stress shielding in the humerus bone.
Clinical Trials
The fact that the numerical results of structural support elements prepared for patient satisfaction in surgery coincide with reality has the effect of increasing operating safety. For this reason, an implant design prepared specifically for the patient is kept under surveillance for a certain period of time after installation and improvements are recorded. During the observation process, patient satisfaction and value changes in implant-specific parameters are the criteria that show the success of the study. Studies on clinical trials on implants obtained by AM method in surgery are given below. Lee and colleagues [26] used the glassceramic composition called BGS-7 in the facial bone implant using the additive manufacturing method. As a result of the application performed on 8 different people, a high implant-bone fusion rate and high satisfaction were obtained. In the study, the low amount of implant collapse was stated as the success evaluation criterion, and the amount of collapse in the application was quite low. Angeloni et al. [27] compared PMMA and AM in a dental implant study. The success criteria in the study were determined as color change, early signs of deterioration, procedure time, and patient satisfaction. In 33 patients, 21 implants created by the traditional method and 21 implants created by the AM method were installed, and it was observed that the AM method was relatively riskier. On the other hand, the assembly time of the model created by the AM method is shorter. In other criteria, the two methods achieved equal scores. Anunmana and colleagues [28] emphasized the importance of the effect of the guide on the accuracy of clinical applications in dental implant studies and compared additive manufacturing methods by evaluating the dimensional accuracy of the models obtained by AM method. Three different methods are included in the application: Stereolithography (SLA), Digital light processing (DLP), and PolyJet. To evaluate the clinical situation, 10 surgical guides were produced on 30 polyurethane models and the implants were placed with the help of these guides. The study success evaluation criteria include processing time, entry, and angular deviation at the peak. In the study, Polete gave more positive results than other methods in terms of deflection angles. The DLP method offered the shortest processing time. Mendonça et al. [29] on increasing bone augmentation in dental implant studies, compared a sample taken from the patient (autograft) with a piece obtained by AM. Measuring the amount and quality of bone formation was preferred as the success criterion of the study. According to the results of the study, the AM method offers advantages in geometry and anatomical precision compared to traditional methods. Additionally, β-tricalcium phosphate enhances bone growth, making it an alternative solution to autograft. Liu et al. [30] state that porous titanium implants with AM method are safe in bone deformations centered in the metaphyseal region. In the study, finite element analysis was used to examine bio-regeneration after implant installation. The results of the study reflect that mechanical conductivities vary according to implant fixation methods. Among the fixation methods, with wings and screws, the stress is transferred mostly to the lateral bone and prosthesis body. Intramedullary (IM) nail ensures that stress is transferred evenly throughout the bone and prosthesis structure. Fixation with nails is relatively more suitable for bone regeneration along with its compliance with Wolff’s law.
Challenges and Future Perspectives
The need for efficient orthopedic surgical treatments is in its highest demand due to the increasing aging population, diseases and expanding modes of injuries. The success of such treatments highly relays on the ability to design, produce and implement appropriate implants. Since the advent of AM a more dynamic, intricate and precise implants production have become achievable. Due to this, orthopedic implants of any size and shape are thinkable nowadays with even a more patient specific orthopedic approaches emerging rapidly.
To secure a successful orthopedic surgical treatment through AM based implants, identifying the suitable material and design combination is important. Despite extensive efforts satisfying the opposing implant property requirements still poses some challenges and this is one of the research areas which needs further investigation. Usually, materials with properties very similar to native bone tend to be weaker and less compact, meanwhile those with good strength lack the biological characteristics. From this perspective, structural optimizations along with multi material production strategies hold huge potential in achieving excellent property balance for orthopedic implants.
In the years to come, it is expected that research directions to be more towards digitally analyzing multi material and porous implants through more realistic mechanical as well as biological models. This would allow to create robust orthopedic treatment systems with optimized implants, predictable properties and efficient clinical trials.
Acknowledgement
This work was supported by the Scientific and Technological Research Council of Turkey under 2244 industrial doctorate program (project codes are 119C154 and 118C136).
Conflict of interest
The authors declare no conflict of interest.
References
- Tsakiris, Violeta, Christu Tardei, Florentina Marilena Clicinschi (2021) Biodegradable Mg Alloys for Orthopedic Implants – A Review. Journal of Magnesium and Alloys 9(6): 1884-1905.
- Kotrych, Daniel, Andrea Angelini, Andrzej Bohatyrewicz, Pietro Ruggieri (2023) 3D Printing for Patient-Specific Implants in Musculoskeletal Oncology. EFORT Open Reviews 8(5): 331-339.
- Pérez, Mercedes, Diego Carou, Eva María Rubio, Roberto Teti (2020) Current Advances in Additive Manufacturing. Procedia CIRP 88: 439-444.
- Rendas, Pedro, Lígia Figueiredo, Ricardo Cláudio, Catarina Vidal, Bruno Soares, et al. (2023) Investigating the Effects of Printing Temperatures and Deposition on the Compressive Properties and Density of 3D Printed Polyether ketone. Progress in Additive Manufacturing.
- Meng, Meng, Jinzuo Wang, Huagui Huang, Xin Liu, Jing Zhang, et al. (2023) 3D Printing Metal Implants in Orthopedic Surgery: Methods, Applications and Future Prospects. Journal of Orthopaedic Translation 42: 94-112.
- Liverani, Erica, Giulia Rogati, Stefania Pagani, Silvia Brogini, et al. (2021) Mechanical Interaction between Additive-Manufactured Metal Lattice Structures and Bone in Compression: Implications for Stress Shielding of Orthopaedic Implants. Journal of the Mechanical Behavior of Biomedical Materials 121: 104608.
- Serrano-Aroca Ángel, Alba Cano-Vicent, Roser Sabater I Serra, Mohamed El-Tanani, Alaa AA Aljabali, et al. (2022) Scaffolds in the Microbial Resistant Era: Fabrication, Materials, Properties and Tissue Engineering Applications. Materials Today Bio 16:100412.
- Zhou, Keran, Farah Alwani Azaman, Zhi Cao, Margaret Brennan Fournet, and Declan M. Devine. 2023. Bone Tissue Engineering Scaffold Optimisation through Modification of Chitosan/Ceramic Composition. Macromol 3(2): 326-342.
- Jiang, Dayue, Fuda Ning, and Ying Wang (2021) Additive Manufacturing of Biodegradable Iron-Based Particle Reinforced Polylactic Acid Composite Scaffolds for Tissue Engineering. Journal of Materials Processing Technology 289: 116952.
- Shao Hanyu, Qiyue Zhang, Mingman Sun, Ming Wu, Xu Sun, et al. (2023) Effects of Hydroxyapatite-Coated Porous Titanium Scaffolds Functionalized by Exosomes on the Regeneration and Repair of Irregular Bone. Frontiers in Bioengineering and Biotechnology 11:1283811.
- Marin, Elia, and Alex Lanzutti (2024) Biomedical Applications of Titanium Alloys: A Comprehensive Review. Materials 17(1): 114.
- Kadi, Fatima, Ghasem Dini, S. Ali Poursamar, and Fatemeh Ejeian. (2024) Fabrication and Characterization of 3D-Printed Composite Scaffolds of Coral-Derived Hydroxyapatite Nanoparticles/Polycaprolactone/Gelatin Carrying Doxorubicin for Bone Tissue Engineering. Journal of Materials Science. Materials in Medicine 35(1): 7.
- Filippi, Miriam, Gordian Born, Mansoor Chaaban, Arnaud Scherberich (2020) Natural Polymeric Scaffolds in Bone Regeneration. Frontiers in Bioengineering and Biotechnology 8.
- Wu Yi-Fan, Ya-Ting Wen, Eisner Salamanca, Lwin Moe Aung, Yan-Qiao Chao, et al. (2024) 3D-Bioprinted Alginate-Based Bioink Scaffolds with β-Tricalcium Phosphate for Bone Regeneration Applications. Journal of Dental Sciences 19(2): 1116-1125.
- M Arshad, N Khoramshahi, G Shirani (2023) Additively custom‐made 3D‐printed subperiosteal implants for the rehabilitation of the severely atrophic maxilla (a case report). Clin. Case Reports 11(11): 1-8.
- P Balamurugan, N Selvakumar (2021) Development of patient specific dental implant using 3D printing. In: J Ambient, Intell Humaniz (Eds.,) Comput 12(3): 3549-3558.
- F P Moncayo-Matute, E Vázquez-Silva, P G Peña-Tapia, P B Torres-Jara, D P Moya-Loaiza, et al. (2023) Finite Element Analysis of Patient-Specific 3D-Printed Cranial Implant Manufactured with PMMA and PEEK: A Mechanical Comparative Study. Polymers (Basel) 15(17): 3620.
- F Danielli, L Ciriello, L La Barbera, J F Rodriguez Matas, G Pennati (2023) On the need of a scale-dependent material characterization to describe the mechanical behavior of 3D printed Ti6Al4V custom prostheses using finite element models. J Mech Behav Biomed Mater 140: 105707.
- M Rana, S Karmakar, A Bandyopadhyay, A Roychowdhury (2023) Design and manufacturing of patient-specific Ti6Al4V implants with inhomogeneous porosity. J Mech Behav Biomed Mater 143: 105925.
- S Ciklacandir, S Mihcin, Y Isler (2022) Detailed Investigation of Three-Dimensional Modeling and Printing Technologies from Medical Images to Analyze Femoral Head Fractures Using Finite Element Analysis. Irbm 43(6): 604-613.
- A Ouldyerou, L Aminallah, A Merdji, A Mehboob, H Mehboob (2023) Finite element analyses of porous dental implant designs based on 3D printing concept to evaluate biomechanical behaviors of healthy and osteoporotic bones. Mech Adv Mater Struct 30(11): 2328-2340.
- F Haque, A F Luscher, K A S Mitchell, A Sutradhar (2023) Optimization of Fixations for Additively Manufactured Cranial Implants: Insights from Finite Element Analysis. Biomimetics 8(6).
- A Vautrin, J Aw, E Attenborough, P Varga (2023) Fatigue life of 3D-printed porous titanium dental implants predicted by validated finite element simulations. Front Bioeng Biotechnol 11: 1-11.
- H Ma, S Xu, X Ju, A Tang, X Hu (2023) Finite Element Analysis of Renewable Porous Bones and Optimization of Additive Manufacturing Processes. Coatings 13(5).
- E Savran, OC Kalay, NB Alp, F Karpat (2023) Design and analysis of lattice structure applied humerus semi-prosthesis. Materials Testing 7(65).
- U L Lee, J Y Lim, S N Park, B H Choi, H Kang, et al. (2020) A clinical trial to evaluate the efficacy and safety of 3d printed bioceramic implants for the reconstruction of zygomatic bone defects. Materials (Basel) 13(20): 4515.
- F A De Souza, M C Blois, K Collares, M B F Dos Santos (2024) 3D-printed and conventional provisional single crown fabrication on anterior implants: A randomized clinical trial. Dent Mater 40(2): 340-347.
- C Anunmana, C Ueawitthayasuporn, S Kiattavorncharoen, P Thanasrisuebwong (2020) In vitro comparison of surgical implant placement accuracy using guides fabricated by three different additive technologies. Appl Sci 10(21): 1-11.
- C M De Almeida Malzoni, V Gonçalves, J Possari, E M Junior (2022) The use of 3D ceramic block graft compared with autogenous block graft for rehabilitation of the atrophic maxilla: a randomized controlled clinical trial. Trials 23(1): 903.
- B Liu, et al. (2022) Mechanical Distribution and New Bone Regeneration After Implanting 3D Printed Prostheses for Repairing Metaphyseal Bone Defects: A Finite Element Analysis and Prospective Clinical Study. Front Bioeng Biotechnol 10(6): 1-10.
-
Efe Savran, Semir M Negash, Nazmi Bülent Alp and Fatih Karpat*. Additively Manufactured Implant Applications in Orthopedic Surgery. Anaest & Sur Open Access J. 5(1): 2024. ASOAJ.MS.ID.000602.
-
Orthopedic surgery, Cancer removal, Operations, Antimicrobial strategies, Hydroxyapatite, Drugs, Polymethylmethacrylate, Hip arthroplasty
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






