Case Report
Case Report
Spontaneous subcutaneous emphysema and pneumomediastinum : A complication of high-flow nasal oxygen therapy
Masad Ilyass1*, Touab Rida1, Mounir Reda2, Serghini Issam3, Alaoui Hassan3 and Qamouss Youssef3
1Department of Anesthesiology and Intensive Care, Military Hospital Mohammed V, Faculty of Medicine and Pharmacy of Rabat, Mohammed V University, Morocco
2Department of cardiovascular surgery, Avicenne Military Hospital Marrakech, Faculty of Medicine and Pharmacy of Marrakech FMPM Cadi AyyadUniversity Marrakech, Morocco
3Department of Anesthesiology and Intensive Care, Avicenne Military Hospital Marrakech, Faculty of Medicine and Pharmacy of Marrakech FMPM Cadi AyyadUniversity Marrakech, Morocco
Masad Ilyass, Department of Anesthesiology and Intensive Care, Military Hospital Mohammed V, Faculty of Medicine and Pharmacy of Rabat, Mohammed V University, Morocco.
Received Date: August 22, 2022; Published Date: January 10,2023
Abstract
Spontaneous subcutaneous emphysema and pneumomediastinum, unrelated to mechanical air flow, were newly defined as a problem of sufferers with coronavirus disorder (COVID-19) pneumonia without the related hazard factors. The predominant goal of supplying this example is to spotlight an extraordinary however vital problem amongst sufferers with COVID-19 pneumonia handled with a high-go with the drift nasal cannula (HFNC). Spontaneous pneumothorax has been discovered in sufferers tormented by SARS-CoV-2 pneumonia. Although the viral contamination itself contributes to its development, better PEEP generated via way of means of each HFNC and mechanical air flow is any other hazard component for multiplied alveoli harm and air leak. Herein, we gift a case of an affected person without a preceding records of lung sicknesses who changed into identified with COVID-19 viral pneumonia complex via way of means of Spontaneous subcutaneous emphysema and pneumomediastinum that befell throughout HFNC oxygen therapy.
Keywords: Covid-19; Oxygen therapy; Pneumomediastinum; Subcutaneous emphysema
Introduction
The coronavirus disorder 2019 (COVID-19) is worldwide, hastily spreading disorder, difficult worldwide health care and economics There are numerous traditional techniques of oxygen supplementation for dyspneic sufferers – easy nasal cannulas, easy oxygen mask, oxygen mask with a reservoir, and high-go with the drift nasal cannulas (HFNC). Each of them generates an exceptional expected fraction of stimulated oxygen (FiO2), relying on oxygen go with the drift and the affected person’s breathing rate.
Spontaneous subcutaneous emphysema and pneumomediastinum, unrelated to mechanical ventilation, have been newly described as a complication of patients with coronavirus disease (COVID-19) pneumonia without the associated risk factors. The main objective of presenting this case is to highlight a rare but important complication among patients with COVID-19 pneumonia treated with a high-flow nasal cannula (HFNC).
Case Report
A 40-year-old patient with no history was admitted to intensive care for treatment of covid 19 pneumonia. The beginning of the symptoms dates back to 4 days before his admission by cough, fever numbered at 38.5 with asthenia. PCR covid 19 positive, chest CT: bilateral ground glasses, right basal condensation, the damage is estimated at 50%.
SpO2 at ambient air 70% TA 13/7 FC 93 bpm, Electrocardiogram was without abnormality.
In the biological assessment: white blood cells at 16,000 with neutrophil polynuclear predominance, lymphopenia at 400, CRP 161, HB 15.3, and platelets at 393,000. the patient was put on antibiotic therapy based on ceftriaxone, ciprofloxacin and azithromycin, vitamin therapy, a
On the respiratory level, the patient was put under the mask at a high concentration of 15l/min without clinical improvement, hence his putting on HFNC, flow at 60l/min, and FiO2 100% for 48 hours.SpO2 was 94 to 96%. Then start progressive weaning in flow and FiO2.
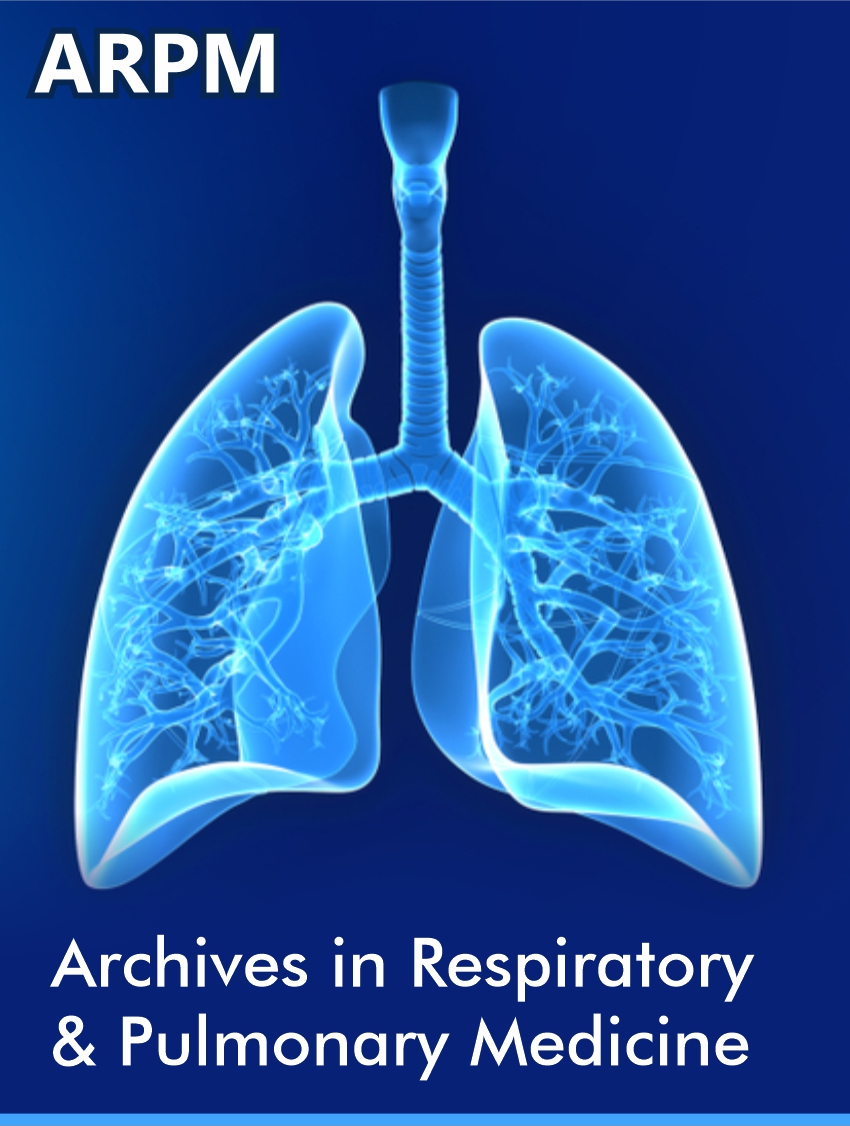
the evolution was marked by the clinical worsening and the appearance of subcutaneous emphysema during the 3rd day of his hospitalization (Figure 1). the realization of a thoracic computed tomography of control was impossible.
Chest X-ray (anteroposterior incidence in half seated position) notes the Presence of clarity at the level of the subcutaneous soft parts of the thoracic wall more marked on the left, in relation to the subcutaneous emphysema (Figure 2).
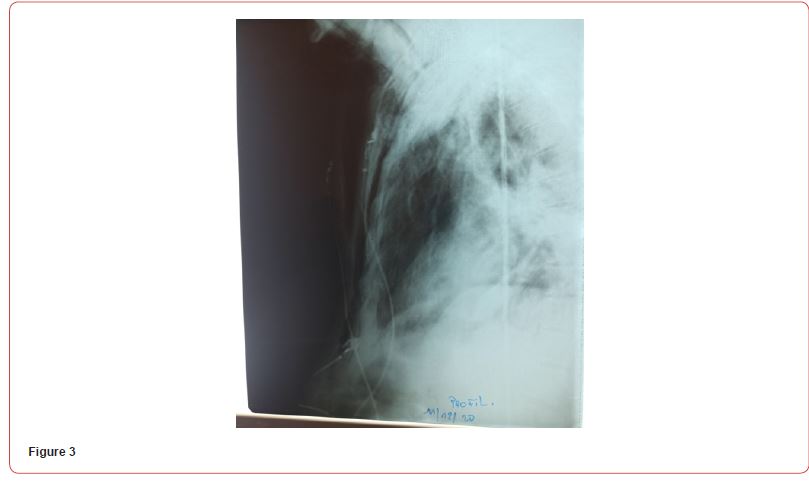
Chest X-ray (profile view): showing the dissecting nature of the subcutaneous emphysema, associated with pneumomediastinum (Figure 3).

The action to be taken was respect for emphysema with twicedaily radiological control and non-invasive ventilation sessions with the following parameters: Inspiratory Support at 14, pep at 3, and FiO2 according to saturation with a target of 94%; thus, the introduction of corticosteroid therapy based on prednisone 1mg/kg. The evolution was the disappearance of the emphysema coinciding with the respiratory weaning and the putting of the patient under a high-concentration mask and then a nasal cannula of oxygen with a flow of 4l/min.
Discussion
A novel coronavirus, named excessive acute respiration syndrome coronavirus 2 (SARS-CoV-2) changed into diagnosed as an etiological factor, first discovered in a cluster of sufferers with pneumonia of unknown foundation in a metropolis of Wuhan, China, on the cease of 2019 [1]. The excessive-glide nasal cannula (HFNC) is a non-invasive respiration assist machine, designed to supply 20–eighty L/min of air and oxygen combination this is accurately heated and humidified after which allotted via extensive nasal cannulas. It changed into formerly established to have an excessive medical efficacy in enhancing the ventilation/perfusion ratio, decreasing respiration effort, and elevating oxygenation [2,3]. During the COVID-19 pandemic, HFNC won lots of extra interest as a probable manner to keep away from intubation in a few sufferers [3,4].
Air leak is a well-known complication of positive pressure ventilation, and HFNC provides increased pressure within airways Oriol Roca, et al. [5], which may potentially cause an air leak. Several mechanisms cause the improvement of Spontaneous subcutaneous emphysema and pneumomediastinum. First is the alveolar rupture secondary to irritation and diffuse alveolar pressures because of coughing. The escaping air from the ruptured alveoli tracks alongside the broncho vascular sheaths, dissecting into the pulmonary hila and escaping into the mediastinal space. This is visible on thoracic computed tomography scans demonstrating the Macklin impact, defined as linear collections of air non-stop to the broncho vascular sheaths dissecting into the pulmonary hilum [6]. Second is the direct viral invasion of the lung parenchyma, visceral and parietal pleura inflicting disruption of the parenchymal and pleural integrity or ruptured alveoli main to next air leak [7]. The 0.33 is the prothrombotic impact of COVID-19 contaminationinflicting pulmonary vascular thrombosis and next necrosis withinside the alveolar membranes. Fourth is cytokine stormprompted diffuse alveolar harm or direct viral contamination of kind 1 and kind 2 pneumocytes growing the chance of alveolar rupture [8]. Some authors additionally join chronic cough, a not unusual place symptom of COVID-19, with an accelerated chance of Spontaneous subcutaneous emphysema and pneumomediastinum because of excessive intrapulmonary strain [9,10]. Coughing reasons, a fast boom in intra-pulmonary strain—whilst the glottis is closed and intracoastal muscular tissues agreement collectively with the diaphragm, the intrathoracic strain can upward push to three hundred mmHg (circa four hundred cm water strain) [11]. We presume that producing PEEP might also additionally moreover make contributions to alveolar harm through rupturing their partitions withinside the presence of diffuse neutrophilic infiltrations withinside the alveoli. On the alternative hand, it without a doubt is more secure than mechanical ventilation, due to the fact the PEEP generated the use of excessive-glide nasal cannulas isn’t as excessive as in closed-machine devices. Every case of the fast deterioration of oxygenation in an affected person supported with HFNC ought to improve a suspicion of pneumothorax and cause right similarly decision-making. Through this case, we would really like to elevate fundamental issues approximately the use of HFNC in COVID-19 sufferers. First, clinicians ought to be conscious that pneumothorax is probably extra common withinside the organization of sufferers requiring excessive-glide oxygen. Therefore, fast deterioration in oxygenation would possibly suggest this problem and ought to constantly entail a differential diagnosis. Second, we declare that HFNC may not be as secure as presumed, especially in sufferers with COVID-prompted diffuse alveolar destruction. Hence, we’d subsequent time consider placing an affected person onto HFNC earlier than the alveolar destruction exceeds, and PaO2/FiO2 ratio drops under 100.
Conclusion
Subcutaneous emphysema, pneumothorax, and pneumomediastinum need to be notified as a severe hardship for the duration of HFNC therapy. Nevertheless, HFNC is a tremendously secure and really frequently an awesome technique of air flow for plenty sufferers with SARS-Cov-2 caused respiration failure.
Acknowledgement
None.
Conflict of interest
No conflict of interest.
References
- Zhu N, Zhang D, Wang W, Li X, Yang B, et al. (2019) A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med 382(8): 727-733.
- Mauri T, Turrini C, Eronia N, Grasselli G, Volta CA, et al. (2017) Physiologic effects of high-flow nasal cannula in acute hypoxemic respiratory failure. Am J Respir Crit Care Med 195(9): 1207-1215.
- Geng S, Mei Q, Zhu C, Yang T, Yang Y, et al. (2020) High flow nasal cannula is a good treatment option for COVID-19. Heart Lung 49(5): 444-445.
- Gürün Kaya A, Öz M, Erol S, Çiftçi F, Çiledag A, et al. (2020) High flow nasal cannula in COVID-19: A literature review. Tuberk Toraks 68(2): 168-174.
- Oriol Roca, Gonzalo Hernández, Salvador Díaz Lobato, José M Carratalá, Rosa M Gutiérrez, et al. (2016) Current evidence for the effectiveness of heated and humidified high flow nasal cannula supportive therapy in adult patients with respiratory failure. Crit Care 20(1): 109.
- Murayama S, Gibo S (2014) Spontaneous pneumomediastinum and Macklin effect: overview and appearance on computed tomography. World J Radiol 6(11): 850-854.
- Tucker L, Patel S, Vatsis C, Antonia Poma, Ali Ammar, et al. (2020) Pneumothorax and pneumomediastinum secondary to COVID-19 disease unrelated to mechanical ventilation. Case Rep Crit Care 2020: 6655428.
- Machiraju PK, Alex NM, Safinaaz, Baby NM (2021) Pneumomediastinum in COVID-19: A series of three cases and review of literature. SAGE Open Med Case Rep 9.
- Woodside KJ, van Sonnenberg E, Chon KS, Loran DB, Tocino IM, et al. (2003) Pneumothorax in patients with acute respiratory distress syndrome: Pathophysiology, detection, and treatment. J Intensive Care Med 18(1): 9-20.
- Akdogan RE, Mohammed T, Syeda A, Jiwa N, Ibrahim O, et al. (2021) Pneumothorax in Mechanically Ventilated Patients with COVID-19 Infection. Case Rep Crit Care 2021: 6657533.
- McCool FD (2006) Global physiology, and pathophysiology of cough: ACCP evidence-based clinical practice guidelines. Chest 129(1 Suppl): 48S-53S.
-
Masad Ilyass*, Touab Rida, Mounir Reda, Serghini Issam, Alaoui Hassan and Qamouss Youssef. Spontaneous subcutaneous emphysema and pneumomediastinum : A complication of high-flow nasal oxygen therapy. Archives in Respiratory & Pulmonary Medicine. 1(2): 2023. ARPM.MS.ID.000505.
-
Covid-19, Oxygen therapy, Pneumomediastinum, Subcutaneous emphysema, Pneumonia, Nasal cannula, Coronavirus disorder
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.