Mini Review
Mini Review
Non-pharmacological aspects of the treatment of allergic diseases in pregnancy
Jusufović Edin1,2*, Lazic Zorica3,4, Cupurdija Vojislav3,4, Osmic Munevera1,2, Jusufovic Azra5 and Arandjelovic Snezana6,7
11Center for Specific and Non-Specific Lung Diseases of Public Health and Educational Center “Dr. Mustafa Sehovic”, Bosnia, and Herzegovina
2Faculty of Medicine of University of Tuzla, Bosnia, and Herzegovina
3Pulmonology Clinic of the Clinical Center Kragujevac, Kragujevac, Serbia
4Faculty of Medicine, University of Kragujevac, Kragujevac, Serbia
5Clinic for Pulmonary Diseases, University Clinical Centre, Tuzla, Bosnia, and Herzegovina
6Clinic for Allergy and Clinical Immunology, University Clinical Center of Serbia, Belgrade, Serbia
7Faculty of Medicine of University of Belgrade, Belgrade, Serbia
Edin Jusufovic, Center for Specific and Non-Specific Lung Diseases of Public Health and Educational Center “Dr. Mustafa Sehovic”, Faculty of Medicine of University of Tuzla, Bosnia, and Herzegovina.
Received Date: February 09, 2023; Published Date: March 23, 2023
Abstract
The approach to the non-pharmacological treatment of allergic diseases in pregnancy closely mirrors the non-pharmacological approach to the treatment of these conditions in the general population. In pregnant women, the importance of avoiding unnecessary medical therapy is paramount because of concerns about the effects of pharmacological therapy on fetal health. Maximizing non-pharmacological approaches as appropriate in an effort to minimize pharmacological interventions is strongly recommended. In some cases, adequate relief can be achieved with non-pharmacological interventions alone, and in many cases, the need for pharmacological therapy can be reduced by concurrent use of non-pharmacological approaches. At all times, it is critical to adequately ensure the well-being of both mother and baby. Due to the strong influence of the environment on allergic diseases, environmental control measures and non-pharmacological therapies can have a large impact on the severity of the disease and symptoms in patients in a safe and effective way.
Keywords: Allergic diseases; Pregnancy; Non-pharmacological treatment
Abbreviations: Ig-immunoglobulin; FEV1-Forced Expiratory Volume in 1 Second; FeNO-Fractional Exhaled Nitric Oxide; HEPA-High Efficiency Particulate Air; IPM-Integrated Pest Management; HVAC-Heating, Ventilation and Air Conditioning
Introduction
Pregnancy represents a unique physiological state that makes the management of chronic diseases more challenging, especially when considering the use of pharmacological therapies in the context of the risk of possible teratogenicity and poor maternal-fetal outcomes [1]. Allergic diseases are among the most common disorders affecting 18-30% of women in the United States during their reproductive years, with asthma and allergic rhinitis being the most common [2]. Allergic rhinitis, asthma and atopic dermatitis are the three main allergic diseases that can be expected during pregnancy. Non-pharmacological approaches to the treatment of atopic disorders in pregnancy must be a key part of any management plan for the disease state. This need is greatest during the first trimester. This chapter focuses on effective avoidance strategies and other non-pharmacological approaches to the treatment of common allergic disease in pregnant women, enabling better outcomes while limiting exposure to unnecessary medical therapy [3].
Nasal symptoms of allergic rhinitis are common in the pregnant population and occur in about 30% of pregnant women. In addition to pre-existing conditions, pregnancy-related hormones can affect nasal blood flow and local mucus glands, leading to previously absent symptoms or worsening of pre-existing nasal conditions. Among the etiologies responsible for nasal symptoms during pregnancy, allergic rhinitis, vasomotor (non-allergic) rhinitis, sinusitis, and medicinal rhinitis are the most common requiring treatment. The course of pre-existing allergic rhinitis during pregnancy is somewhat unpredictable and unique for each individual patient. Allergic rhinitis that existed before pregnancy is known to improve, worsen or remain stable during pregnancy [2]. Allergic rhinitis usually occurs in patients with severe nasal and ocular symptoms, such as rhinorrhea, nasal itching, sneezing, eye itching, and eye irritation. Allergic rhinitis can usually be caused by environmental factors such as pollen, dust mites, mold, and animal dander. As such, allergen avoidance is a key treatment modality for patients with allergic rhinitis. Although allergy skin tests can be useful for identifying causative allergens, due to the very small risk of a systemic reaction, skin testing should be avoided during pregnancy. Serum IgE testing for environmental allergens is now widely available and represents a safer alternative for assessing causative allergens in pregnant women [4,5].
Asthma can usually manifest itself with symptoms such as shortness of breath, wheezing, coughing and chest tightness. Confirmation of the diagnosis is ideally made by demonstrating evidence of reversible airway obstruction, which can be quantified by spirometry or pulmonary function testing showing an increase in FEV1 greater than or equal to 12% after inhalation of a shortacting bronchodilator such as albuterol. An elevated FeNO fraction may also indicate a diagnosis in the right clinical context. Although in non-pregnant patients, the methacholine challenge test can be used to diagnose asthma, this is not recommended in pregnant women [4]. Similarly, patients with asthma experience improvement, worsening, or unchanged disease severity during pregnancy, with each occurring in approximately one-third of patients. As for asthma, it is vital to maintain optimal management during pregnancy, as poor asthma control can be associated with preterm delivery, preeclampsia, low birth weight, and neonatal and maternal hypoxia [2,4].
Allergens
In general, the initial approach to non-pharmacological treatment of allergic rhinitis, asthma and atopic dermatitis in pregnancy does not differ from that in non-pregnant patients. Avoidance of known irritants and allergens is the cornerstone of the therapeutic strategy of allergic rhinitis and allergic asthma and should be recommended first for all patients [2]. Summary of allergen avoidance measures is shown in Table 1.
Table 1: Summary of allergen avoidance measures.
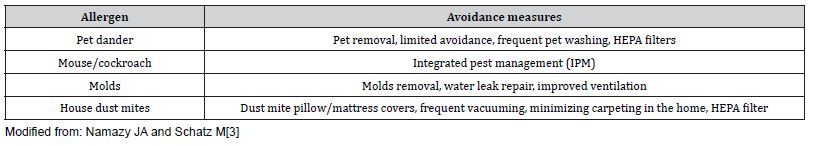
The following sections will describe many of the major allergens and the appropriate avoidance measures.
Pet dander allergens
Pregnant women with known sensitivity to pet dander should be advised that removing the pet from the environment is the most effective environmental control measure. Dogs and cats in particular are significant sources of indoor allergens common to many allergic patients. Fel d1 (Felis domesticus allergen 1) is an important cat allergen and is transmitted through the air in particles larger than 2.5 μm. Fel d1 is known to remain in the air for a significantly longer period of time. The main allergenic proteins for dogs, can f1 and can f2 (Canis familiaris allergens 1 and 2), are similar, although not as persistent in the air as those from cats. Cat and dog allergens are found in their secretions and secretions and on dander [6]. In a study of 20 patients with allergic asthma and pet sensitivities, of the patients who removed their pet and were followed up after one year, none of these patients required inhaled corticosteroids, in contrast to 9/10 of the patients who kept their pets in the control group [7]. In many cases, complete removal of the pet is either impractical or undesirable. Clinicians often recommend frequent washing of cats and dogs in an effort to reduce the level of pet dander allergens in the home and thus the symptoms of allergic rhinitis. It has been shown that the level of Can f1 in the home, as well as on the dogs themselves and their dander, can be significantly reduced by shampooing and blow-drying the dog at least twice a week. Can f1 levels have been shown to return to prewashed levels within 3-4 days [8]. In cats, weekly cat washing has been shown to result in a limited reduction in Fel d1 both in the patient’s home and in the cat, especially after 1 week [9]. Given the difficult nature of frequent animal washing, this strategy has not found widespread acceptance [10]. More likely to be successful in some cases would be a strategy of limited avoidance, such as ensuring that the patient’s pet is confined to the outside of the house or at least prohibited from entering the patient’s bedroom. The following discusses the use of air purifiers with HEPA filters in the treatment of animal dander allergy [1].
Allergens of mice and cockroaches
For pest allergens such as mouse and cockroach that are particularly problematic in low-income and urban settings, environmental non-pharmacological control measures are also of considerable importance [10]. For mouse allergen exposure, studies have typically used integrated pest management to reduce mouse allergen concentrations. IPM involves a multi-intervention approach, which includes sealing cracks and holes in the house, placing mousetraps, careful food disposal, intensive cleaning procedures and, when necessary, the use of rodenticides. Studies examining IPM have used a variety of approaches ranging from providing education on IPM strategies to actual professional implementation of these interventions [11,12]. A reduction of at least 50-75% of mouse allergens at home has been shown to be directly associated with significant improvement in asthma clinical outcomes [13-15]. Some of these studies also showed that professionally performed IPM led to a 70-75% reduction in allergen concentrations in house mice, while one study showed that a comparable reduction was achieved by providing IPM education to patients alone. However, it should be noted that another study showed only minimal change in mouse allergen concentrations when looking at IPM education interventions alone compared to controls [12-14]. As such, professionally performed IPM interventions appear to be effective in achieving clinically relevant reductions in mouse allergen concentration levels in the home; however, the efficacy of patient education-only IPM interventions has yet to be definitively proven reliable [10]. For pregnant women with known mouse sensitivity and concurrent allergic rhinitis and/or asthma, IPM education or referral to obtain professionally performed IPM interventions, when appropriate, is highly recommended.
Similar to environmental control measures for mouse allergens, integrated pest management (IPM) strategies are often used for patients sensitized and exposed in the home to cockroach allergen. Although there are over 4500 species of cockroaches, only four are indoor pests, Periplaneta americana, Blatta orientalis, Blattella germanica and Supella longipalpa, and the main allergens are Bla g1, Bla g2 and per a1 [6]. As with mouse allergen strategies, cockroach IPM consists of a multi-intervention approach that may include sealing holes and cracks in the home, using pesticides, intensive cleaning aimed at reducing cockroach allergen reservoirs, and meticulous disposal of food. These interventions have been shown to provide significant reductions in house cockroach allergen levels compared to controls in the homes of children with asthma in low-income urban areas. In fact, it has been shown that cockroach allergen levels can be significantly reduced by 80-90% using IPM strategies [15-19]. Furthermore, clinical benefit associated with reduced exposure to cockroach allergens in the home has been demonstrated, with data showing clinical benefit when at least a 50-90% reduction in cockroach allergen concentrations or the median number of cockroaches captured is achieved [18,20]. There is also a suggested clinical benefit observed in children with asthma, but without cockroach sensitivity, who are exposed to cockroach allergen in their home environment. However, the benefit is not as pronounced as shown in children sensitized to cockroach allergens [20]. Therefore, as with mouse allergen exposure, it can be extrapolated that IPM should be part of a comprehensive management strategy advised to cockroachsensitized pregnant women affected by allergic rhinitis and/or asthma. Insecticidal sprays should not be used, either by the patient themselves or by IPM professional services, in an effort to avoid the irritating effects of these chemical aerosolized compounds that can exacerbate respiratory diseases [10].
Other animal allergens
Other animals, such as horses, birds, and rabbits, are also common allergens that can worsen patients’ symptoms. The major equine allergen, Equ c1, has been found in equine salivary glands, urine, and dander [19]. Although there is very little research on bird sensitization, a recent study found that bird sensitization is lower than that found in dogs or cats, possibly due to fewer pet birds [20]. Other smaller pets that are furry, such as hamsters, rabbits, and guinea pigs, have become increasingly common in recent decades, with more than 5% of households in the United States and Europe having small furry pets. However, quantitative measurements of these allergens in house dust are suboptimal [19]. As with other animal allergens, avoidance measures are advised for sensitive and symptomatic patients [3].
Allergenic molds
Asthma morbidity has been associated with mold and/or damp home environments in multiple studies [21,22]. Mold is known to become problematic in home environments affected by excess moisture. Excess moisture can be secondary to a number of factors, including ventilation problems, water intrusion, plumbing problems, and other structural problems. Carbon dioxide levels have been shown to correlate with the concentration of fungal allergens, supporting the concept that lack of ventilation promotes mold growth. Concentrations of mold allergens are most elevated at ambient temperatures ranging from 20 to 22.5°C [23]. The most studied allergenic fungi are Aspergillus, Alternaria, Penicillium, Fusarium, Cladosporium and Epicoccum [6]. Asthma outcomes have been shown to improve following mold and damp remediation interventions. These interventions include different approaches: stopping rainwater ingress, removing mold from surfaces, repairing plumbing leaks, and installing proper ventilation. These interventions have been shown in studies to improve asthma outcomes, including reduced medication use, fewer symptom days, and reduced use of health care resources [24-26]. The risk of respiratory symptoms and mold exposure are related, regardless of whether the patient is sensitized to mold allergens or not. Sensitization to fungal allergens is thought to increase the risk of morbidity [27,28]. It is recommended that patients with mold sensitization and allergic asthma use a central heating, ventilation, and air conditioning (HVAC) system with changed filters to reduce the movement of fungal spores from the outside into the home. When using mold remediation, the National Institute for Occupational Safety and Health recommends using at least an N-95 mask when removing visible mold due to the risk of aerosolized particles [10]. Therefore, for patients with allergic rhinitis and known mold sensitization, or for patients with allergic asthma regardless of mold sensitization, it is advisable to implement mold remediation measures for home environments known to be susceptible to significant mold colonization [3].
House dust mites
House dust mites are ubiquitous in many environments around the world. The main allergen comes from dust mite droppings, which are typically 20-30μ in diameter, and the main dust mite species are Euroglyphus and Dermatophagoides. Dust mites are especially prevalent in warm (above 20°C), moist, and dark environments, such as pillows, mattresses, stuffed animals, and carpets [7,29]. In patients with known house dust mite sensitivity and associated symptoms, environmental control measures are common and highly recommended. Interventions targeting the bedroom, due to the large percentage of time spent in it, are typically emphasized [30]. Covering mattresses and pillows in a finely woven fabric that can prevent the passage of mite feces is the primary intervention. Regular washing of bedding in warm or hot water is also recommended, and it is known that if a clothes dryer is used, almost all mites are killed [31,32]. It is well known that the growth of mites is facilitated by a moist environment. Although it is understood that relative humidity thresholds of 45-50% are usually required to achieve control, trials investigating dehumidification have shown mixed results, possibly due to the fact that even a short period of higher humidity can be sufficient to allow reproduction and survival of the mites. house dust [33,34]. Regarding carpets and upholstery, it is recommended that for patients allergic to dust, the amount of carpets in the home be reduced to a minimum and that the carpet be regularly vacuumed, cleaned, and dried in the sun if possible. Furthermore, if high humidity is difficult to control, it is suggested to avoid upholstery as much as possible [30]. Activities such as vacuuming and handling bedding, furniture, or other materials known to contain dust mites can disrupt the allergen and cause it to spread into the air [35]. It is recommended that vacuuming be performed by a person who is not allergic to dust mites if possible [3].
High efficiency filters for air particles
Another strategy that many patients consider is the use of air filters. There are many different types of air filters, and the most recommended are high efficiency particulate air filters (HEPA filters). Other types of air filters, such as electrostatic filters and ionizers, work by electrically charging air particles to remove them. However, these devices are known to emit ozone and as such should be avoided [3]. When looking at cases of known pet allergic patients, HEPA filters were shown to produce about a 30- 40% reduction in airborne cat allergen compared to placebo filters. However, HEPA filters do not appear to significantly affect the level of pet dust allergens, and most importantly, the use of these filters does not appear to significantly improve either allergic rhinitis or asthma symptoms [36] In fact, cat allergen in particular is known to be found in homes long after the cat has been removed, due to the inherent nature of the allergen. Despite these findings, one study showed that the combined practice of frequent vacuuming combined with the use of free-standing HEPA filters placed in multiple rooms in the home was associated with improved asthma outcomes, although there was only minimal change in actual dust allergen levels [37]. As such, it is possible that the combination of high-efficiency particulate air filters in combination with other environmental measures, such as vacuuming to reduce dust allergen deposition, may have clinical benefit in both allergic rhinitis and pregnant women with asthma with known pet dander. allergic sensitivity; however, to date there appears to be no highcertainty evidence to support this assumption [3].
Regarding the use of HEPA filters to reduce house dust mite allergens, a randomized, double-blind, placebo-controlled study looked at patients with a history of allergic rhino conjunctivitis and known allergic sensitivity to dogs, cats, or house dust mites. In the study, the combined use of a HEPA filter in the patient’s bedroom along with dust mite bed pillow covers showed significantly reduced levels of dust particles in the bedroom compared to a placebo. In addition, there was a significant improvement in ocular and nasal symptoms at night in the group of patients receiving combined environmental interventions; however, it should be noted that symptoms did not improve during the day in this group of patients [38]. Overall, this suggests that the benefit of highefficiency particulate air filters in allergic rhinitis and/or asthmatic patients is best realized in combination with other environmental control measures [3].
Immunotherapy against allergens
In addition to other non-pharmacological interventions, desensitization of allergic disease using allergen immunotherapy also has an appropriate role in the treatment of allergic rhinitis and allergic asthma during pregnancy. Subcutaneous immunotherapy has been used to treat allergic diseases for approximately 100 years and has been shown to be very effective for allergic rhinitis, allergic asthma, and insect venom allergies. Studies have shown the safety of subcutaneous immunotherapy during pregnancy, in the sense that no significant change in prematurity, hypertension, congenital malformations or proteinuria, or complications during childbirth was demonstrated, with the exception of a systemic reaction in three patients [39]. In many patients, subcutaneous immunotherapy results in permanent desensitization to allergens, even after discontinuation of immunotherapy. More recently, the use of sublingual immunotherapy (tablets of grass, ragweed, or mites that dissolve under the tongue daily) has entered mainstream practice as an alternative in some cases. The safety of sublingual immunotherapy has been previously examined, with a study of 155 patients during 185 pregnancies receiving sublingual immunotherapy with dust mites or a mixture of five allergens, with a 6-year follow-up showing no systemic reactions in patients receiving sublingual immunotherapy, with only local reactions observed compared to control arms. Twenty-four of these patients started sublingual immunotherapy for the first time during pregnancy. Therefore, the safety of sublingual immunotherapy has been suggested both for patients who have previously received sublingual immunotherapy before pregnancy and for those who start sublingual immunotherapy during pregnancy [40].
Therefore, pregnant women who were previously on stable subcutaneous immunotherapy without significant complications can safely continue with the maintenance dose of immunotherapy throughout pregnancy. For women of childbearing age, consideration of starting subcutaneous immunotherapy before pregnancy may be a wise proactive choice in some cases to avoid the need for medication during pregnancy, especially for allergic asthma. However, subcutaneous immunotherapy should not be initiated during pregnancy, and doses should not be increased during pregnancy due to the possibility of systemic reactions. In case the patient becomes pregnant during the step-up phase of low-dose subcutaneous immunotherapy, the injections should be stopped. An unusual exception may be for a patient with a history of anaphylaxis secondary to venom hypersensitivity and ongoing risk of exposure [2,3].
Exposure to Irritants
Tobacco smoking is a well-established risk factor for many diseases in the general population worldwide. In pregnancy, smoking also has a wide range of negative effects on the health of the mother and fetus, including pregnant women with asthma. Smoking is associated with worsening asthma medication requirements and reduced response to pharmacological asthma therapy. A recent study showed that the relative risk of asthma exacerbation during pregnancy was significantly higher in current and former smokers compared to never smokers and showed that even never smokers who had only passive exposure to tobacco had a significantly increased risk. from exacerbation of asthma during pregnancy [38]. The study reported that never-smokers with passive tobacco exposure had a significantly lower predicted FEV1% compared with patients who never smoked and had no passive tobacco exposure. Because asthma exacerbations are known to be associated with an increased risk of poor pregnancy outcomes, it is absolutely critical that pregnant women be advised to stop smoking immediately and avoid exposure to secondhand smoke [41]. Furthermore, a correlation was established between exposure to smoke in the womb or in childhood and the development of rhinitis and asthma in childhood [42]. In addition to tobacco smoke, mothers with asthma should also avoid other potential irritants, such as pollutants and other harmful chemicals, as much as possible because of their potential to make the disease worse [2,3].
Other Non-Pharmacological Approaches in Asthma and Allergic Rhinitis
A recent review of other non-pharmacological approaches to the treatment of asthma in pregnancy evaluated the effectiveness of certain approaches, such as education, part of the FeNObased treatment algorithm, and progressive muscle relaxation (deliberately applying tension to specific muscle groups followed by release of that tension), which showed some beneficial effects for treatment of asthma in pregnancy. However, the review ultimately emphasized that no firm conclusions could be drawn regarding the true benefit of these approaches due to various limitations in previous studies [43]. Other non-pharmacological approaches to improving asthma symptoms may also include stress reduction management and breathing exercises, as asthma symptoms may be exacerbated by psychological stressors. The breathing exercises previously suggested including the use of breathing patterns that reduce hyperventilation as well as hyperinflation, leading to normalization of carbon dioxide levels and then, theoretically, a reduction in breathlessness and bronchospasm. However, when it was previously tested in children with asthma, no clear evidence of its effectiveness was found [44]. Regarding psychological stress factors and asthma, an appropriate psychiatric evaluation should be performed for pregnant women with asthma who have a concurrent psychiatric illness, and appropriate stress reduction measures should be considered for patients with stress-related symptoms [3].
In allergic rhinitis, the use of saline rinses may facilitate mucus passage and reduce nasal congestion in some patients. Also, the use of external nasal strips can help relieve nasal passage obstruction in some cases. For the treatment of allergic diseases and asthma, although some patients may consider the use of probiotics as an adjunct to standard medical care, there are no studies in pregnant women that demonstrate the therapeutic benefit of probiotics for allergic sensitization, asthma, or atopy. dermatitis. Furthermore, there are currently no societal recommendations supporting the use of probiotics for the treatment of allergic manifestations or asthma [45,46]. As for other non-traditional interventions such as acupuncture, no studies have yet been conducted to evaluate the effects of acupuncture on allergic disease or asthma in pregnant women [3].
Acknowledgment
We would like to thank all colleagues who supported us in writing this paper.
Conflicts of Interest
No conflict of interest.
References
- Bolz M, Körber S, Reimer T, Buchmann J, Schober HC, et al. (2017) The Treatment of Illnesses Arising in Pregnancy. Dtsch Arztebl Int 114(37): 616-626.
- Pali Schöll I, Namazy J, Jensen Jarolim E (2017) Allergic diseases and asthma in pregnancy, a secondary publication. World Allergy Organ J 10(1): 10.
- Namazy JA, Schatz M (2019) Asthma Allergic and Immunologic Diseases During Pregnancy. A Guide to Management. Springer International Publishing.
- Namazy J, Schatz M (2016) The Treatment of Allergic Respiratory Disease During Pregnancy. J Investig Allergol Clin Immunol 26(1): 1-7.
- Namazy JA, Schatz M (2015) Pharmacotherapy options to treat asthma during pregnancy. Expert Opin Pharmacother 16(12): 1783-1791.
- Baldacci S, Maio S, Cerrai S, Sarno G, Baïz N, et al. (2015) Allergy and asthma: Effects of the exposure to particulate matter and biological allergens. Respir Med 109(9): 1089-1104.
- Shirai T, Matsui T, Suzuki K, Chida K (2005) Effect of pet removal on pet allergic asthma. Chest 127(5): 1565-1571.
- Hodson T, Custovic A, Simpson A, Chapman M, Woodcock A, et al. (1999) Washing the dog reduces dog allergen levels, but the dog needs to be washed twice a week. J Allergy Clin Immunol 103(4): 581-585.
- Portnoy J, Kennedy K, Sublett J, Phipatanakul W, Matsui E, et al. (2012) Environmental assessment and exposure control: a practice parameter-furry animals. Ann Allergy Asthma Immunol 108(4): 223.e1-223.e15.
- Ahluwalia SK, Matsui EC (2018) Indoor Environmental Interventions for Furry Pet Allergens, Pest Allergens, and Mold: Looking to the Future. J Allergy Clin Immunol Pract 6(1): 9-19.
- Phipatanakul W, Matsui E, Portnoy J, Williams PB, Barnes C, et al. (2012) Environmental assessment and exposure reduction of rodents: a practice parameter. Ann Allergy Asthma Immunol 109(6): 375-387.
- Pongracic JA, Visness CM, Gruchalla RS, Evans R, Mitchell HE (2008) Effect of mouse allergen and rodent environmental intervention on asthma in inner-city children. Ann Allergy Asthma Immunol 101(1): 35-41.
- Di Mango E, Serebrisky D, Narula S, Shim C, Keating C, et al. (2016) Individualized Household Allergen Intervention Lowers Allergen Level but Not Asthma Medication Use: A Randomized Controlled Trial. J Allergy Clin Immunol Pract 4(4): 671.e4-679.e4.
- Matsui EC, Perzanowski M, Peng RD, Wise RA, Balcer-Whaley S, et al. (2017) Effect of an Integrated Pest Management Intervention on Asthma Symptoms Among Mouse-Sensitized Children and Adolescents with Asthma: A Randomized Clinical Trial. JAMA 317(10): 1027-1036.
- Eggleston PA, Butz A, Rand C, Curtin Brosnan J, Kanchanaraksa S, et al. (2005) Home environmental intervention in inner-city asthma: a randomized controlled clinical trial. Ann Allergy Asthma Immunol 95(6): 518-524.
- Morgan WJ, Crain EF, Gruchalla RS, O'Connor GT, Kattan M, et al. (2004) Results of a home-based environmental intervention among urban children with asthma. N Engl J Med 351(11): 1068-1080.
- Portnoy J, Chew GL, Phipatanakul W, Williams PB, Grimes C, et al. (2013) Environmental assessment and exposure reduction of cockroaches: a practice parameter. J Allergy Clin Immunol 132(4): 802-8.e1-25.
- Arbes SJ, Sever M, Mehta J, Gore JC, Schal C, et al. (2004) Abatement of cockroach allergens (Bla g 1 and Bla g 2) in low-income, urban housing: month 12 continuation results. J Allergy Clin Immunol 113(1): 109-114.
- Rabito FA, Carlson JC, He H, Werthmann D, Schal C (2017) A single intervention for cockroach control reduces cockroach exposure and asthma morbidity in children. J Allergy Clin Immunol 140(2): 565-570.
- Konradsen JR, Fujisawa T, van Hage M, Hedlin G, Hilger C, et al. (2015) Allergy to furry animals: new insights, diagnostic approaches, and challenges. J Allergy Clin Immunol 135(3): 616-625.
- Fisk WJ, Lei Gomez Q, Mendell MJ (2007) Meta-analyses of the associations of respiratory health effects with dampness and mold in homes. Indoor Air 17(4): 284-296.
- Chao HJ, Milton DK, Schwartz J, Burge HA (2002) Dustborne fungi in large office buildings. Mycopathologia 154(2): 93-106.
- Kercsmar CM, Dearborn DG, Schluchter M, Xue L, Kirchner HL, et al. (2006) Reduction in asthma morbidity in children as a result of home remediation aimed at moisture sources. Environ Health Perspect 114(10): 1574-1580.
- Burr ML, Matthews IP, Arthur RA, Watson HL, Gregory CJ, et al. (2007) Effects on patients with asthma of eradicating visible indoor mould: a randomized controlled trial. Thorax 62(9): 767-772.
- Mitchell H, Cohn RD, Wildfire J, Thornton E, Kennedy S, et al. (2012) Implementation of evidence-based asthma interventions in post-Katrina New Orleans: The Head-off Environmental Asthma in Louisiana (HEAL) study. Environ Health Perspect 120(11): 1607-1612.
- Pongracic JA, O'Connor GT, Muilenberg ML, Vaughn B, Gold DR, et al. (2010) Differential effects of outdoor versus indoor fungal spores on asthma morbidity in inner-city children. J Allergy Clin Immunol 125(3): 593-599.
- Gent JF, Kezik JM, Hill ME, Tsai E, Li DW, et al. (2012) Household mold and dust allergens: exposure, sensitization and childhood asthma morbidity. Environ Res 118: 86-93.
- Wilson JM, Platts-Mills TAE (2018) Home Environmental Interventions for House Dust Mite. J Allergy Clin Immunol Pract 6(1): 1-7.
- Singh M, Jaiswal N (2013) Dehumidifiers for chronic asthma. Cochrane Database Syst Rev (6): CD003563.
- Choi SY, Lee IY, Sohn JH, Lee YW, Shin YS, et al. (2008) Optimal conditions for the removal of house dust mite, dog dander, and pollen allergens using mechanical laundry. Ann Allergy Asthma Immunol 100(6): 583-588.
- Miller JD (2017) Difference in mite survival in blankets washed in top-loading vs. front-loading washing machines. J Allergy Clin Immunol 139(2): AB119.
- Arlian LG, Neal JS, Morgan MS, Vyszenski-Moher DL, Rapp CM, et al. (2001) Reducing relative humidity is a practical way to control dust mites and their allergens in homes in temperate climates. J Allergy Clin Immunol 107(1): 99-104.
- Gore RB, Durrell B, Bishop S, Curbishley L, Woodcock A, et al. (2006) High-efficiency vacuum cleaners increase personal mite allergen exposure, but only slightly. Allergy 61(1): 119-123.
- Sulser C, Schulz G, Wagner P, Sommerfeld C, Keil T, et al. (2009) Can the use of HEPA cleaners in homes of asthmatic children and adolescents sensitized to cat and dog allergens decrease bronchial hyperresponsiveness and allergen contents in solid dust? Int Arch Allergy Immunol 148(1): 23-30.
- Francis H, Fletcher G, Anthony C, Pickering C, Oldham L, et al. (2003) Clinical effects of air filters in homes of asthmatic adults sensitized and exposed to pet allergens. Clin Exp Allergy 33(1): 101-105.
- Stillerman A, Nachtsheim C, Li W, Albrecht M, Waldman J (2010) Efficacy of a novel air filtration pillow for avoidance of perennial allergens in symptomatic adults. Ann Allergy Asthma Immunol 104(5): 440-449.
- Oykhman P, Kim HL, Ellis AK (2015) Allergen immunotherapy in pregnancy. Allergy Asthma Clin Immunol 11: 31.
- Shaikh WA, Shaikh SW (2012) A prospective study on the safety of sublingual immunotherapy in pregnancy. Allergy 67(6): 741-743.
- Grarup PA, Janner JH, Ulrik CS (2014) Passive smoking is associated with poor asthma control during pregnancy: a prospective study of 500 pregnancies. PLoS One 9(11): e112435.
- Thacher JD, Gruzieva O, Pershagen G, Neuman Å, Wickman M, et al. (2014) Pre-and postnatal exposure to parental smoking and allergic disease through adolescence. Pediatrics 134(3): 428-434.
- Zairina E, Stewart K, Abramson MJ, George J (2014) The effectiveness of non-pharmacological healthcare interventions for asthma management during pregnancy: a systematic review. BMC Pulm Med 14: 46.
- Macêdo TM, Freitas DA, Chaves GS, Holloway EA, Mendonça KM (2016) Breathing exercises for children with asthma. Cochrane Database Syst Rev 4(4): CD011017.
- Ly NP, Litonjua A, Gold DR, Celedón JC (2011) Gut microbiota, probiotics, and vitamin D: interrelated exposures influencing allergy, asthma, and obesity? J Allergy Clin Immunol 127(5): 1087-1094.
- Mennini M, Dahdah L, Artesani MC, Fiocchi A, Martelli A (2017) Probiotics in Asthma and Allergy Prevention. Front Pediatr 5: 165.
- Sánchez J, Díez S, Cardona R (2015) Pet avoidance in allergy cases: Is it possible to implement it? Biomedica 35(3): 357-362.
- Mendell MJ, Mirer AG, Cheung K, Tong M, Douwes J (2011) Respiratory and allergic health effects of dampness, mold, and dampness-related agents: a review of the epidemiologic evidence. Environ Health Perspect 119(6): 748-756.
-
Jusufović Edin*, Lazic Zorica, Cupurdija Vojislav, Osmic Munevera, Jusufovic Azra and Arandjelovic Snezana. Non-pharmacological aspects of the treatment of allergic diseases in pregnancy. Archives in Respiratory & Pulmonary Medicine. 1(2): 2023. ARPM.MS.ID.000506.
-
Allergic diseases, Pregnancy, Non-pharmacological treatment, Fetal health, Environmental control measures, rhinitis, sinusitis, Pregnancy hormones
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.