Research Article
Research Article
Healthcare-associated Clostridioides difficile infections among pulmonology patients
Jelena Djekic Malbasa 1,2* , Tomi Kovacevic1,2 , Branislav Tušek2 , Anika Trudić1,2 Vladimir Stojšić1,2, Aleksandra Patić1,3
1Faculty of Medicine, University of Novi Sad, Novi Sad, Serbia
2Institute for Pulmonary Diseases of Vojvodina, Sremska Kamenica, Serbia
3Institute for Public Health of Vojvodina, Novi Sad, Serbia
Jelena Djekic Malbasa, Faculty of Medicine, University of Novi Sad, Novi Sad, Institute for Pulmonary Diseases of Vojvodina, Sremska Kamenica, Serbia..
Received Date:August 30, 2024; Published Date:October 02, 2024
Introduction
Clostridioides difficile (C. difficile) is a Gram-positive, anaerobic, toxin-producing bacteria widespread in the environment in spore forms. This bacteria produces two main types of toxins, A and B, responsible for Clostridioides difficile infection (CDI) [1-6].
The significant risk factors for CDI are changes in gastrointestinal microbiota following antibiotic use among older people with multiple commodities, a weakened immune system, and recent hospital or long-term care facility stays [7-17].
Due to wide distribution in the environment in spore forms, around 30% of CDI in European countries in 2020 were communityassociated (CA) or with unknown association (UA), while at least 60% of CDI cases were healthcare-associated (HA) CDI [18-20].
In the USA, the CDC reports that the incidence rate of HA CDI is 57.9 per 100,000 persons, representing a sizeable decline in recent years. The total burden of HA CDI also declined by 36% from 2011 to 2017 [21].
According to the European Centre for Disease Prevention and Control (ECDC), the crude incidence density of HA-CDI in 2016– 2017 was 3.48 cases per 10,000 patient-days, with the highest rates in Lithuania (7.51 cases/10,000 patient-days), Poland (7.50 cases/10,000 patient-days), and Estonia (5.92 cases/10,000 patient-days)[5].
The crude incidence density of HA-CDI in Europa in 2020 was 2.58 cases per 10,000 patient days, compared to 2.02 cases in 2019 and 2.79 cases in 2018. According to the same ECDC report, the highest incidence density was observed in Hungary (3.58 cases per 10,000 patient days), while Lithuania reported the lowest incidence density (1.03 cases per 10,000 patient days). The highest incidence density of HA CDI was reported in tertiary hospitals (3.49/10 000 patients), while specialized and primary types of hospitals reported the lowest (1.44 and 1.75/10 000 patients, respectively) [18].
The HA CDI burden is a significant public health issue in developed countries [20, 21, 22, 23] and considerable challenges in developing countries [5, 24, 22, 23].
Community-acquired pneumonia (CAP) is a hospital admission diagnosis following the highest antimicrobial consumption, one of the most critical risk factors for developing CDI [6].
The burden of HA CDI among patients admitted due to CAP and the profile of pulmonology HA CDI patients in developing countries, such as Serbia, with high antimicrobial consumption (utilization rate) and a very high percentage of multi-drug-resistant strains is not well known [25-27].
The Institute for Pulmonary Diseases of Vojvodina (IPBV) is the tertiary teaching hospital specialized for the diagnosis and treatment of respiratory diseases in Vojvodina Province, Serbia, covering a population of around 1.9 million inhabitants [28].
This study aimed to determine the HA CDI incidence among IPBV patients according to admission diagnosis and analyze patients’ demographic and clinical characteristics from 2015 to 2023.
Material and methods
A retrospective analysis of HA CDI in the IPBV from 1 January 2015 to 31 December 2023 was performed. HA CDI was defined according to the ECDC definition [29].
Reporting forms of HA CDI used in the analysis include the following data: age, gender, date of hospitalization, date of CDI symptoms onset, total length of hospital stay, type of Clinic where CDI were reported, antibiotic consumption prior CDI symptoms, types of CDI toxin positive findings, and outcome of hospitalization (alive, death),
IPBV consist of five Clinics: Clinic for Obstructive Pulmonary Diseases and Acute Pneumopathies (I), Clinic for Granulomatous and Interstitial Lung Diseases (II), Urgent Pulmonology Clinic (III), Pulmonary Oncology Clinic (IV), and Thoracic Surgery Clinic (V), respectively. The stool of patients with diarrhoea was tested for C. difficile toxins and glutamate dehydrogenase (GDH) antigen using a mini-VIDAS system.
Categorical variables were analyzed using χ² or Fisher exact test, while for continuous t-test or ANOVA were performed. All statistical analyses were performed using SPSS version 24, and a p-value <0.005 was considered statistically significant. The study was approved by the Ethics Committee of The Institute for Pulmonary Diseases of Vojvodina, Sremska Kamenica, Serbia, IRB No (27-III/3).
Results
From 2015 to 2023, a total of 444 IPBV patients with confirmed CDI were hospitalized, among 364 (81.9%) had HA CDI during actual hospitalization.
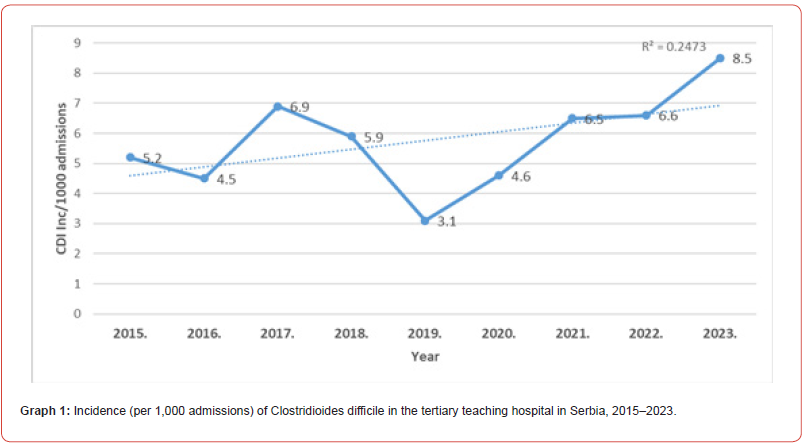
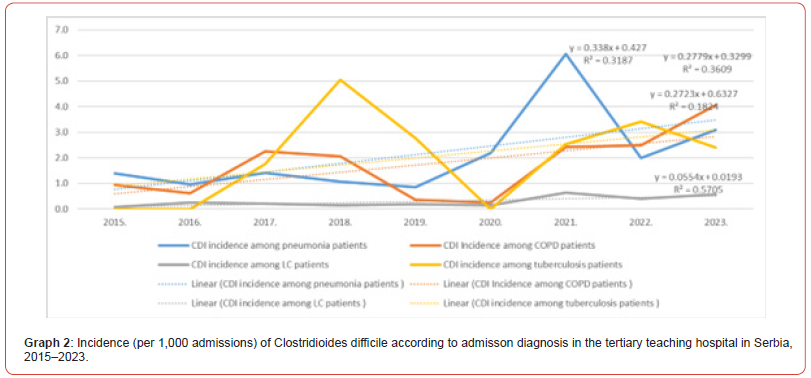
The CDI incidence increased during the observed period, from 3.1/1000 hospital admissions in 2019 to 8.5/1000 in 2023 (Graph1). The highest HA CDI incidence was observed in 2021 for pneumonia as an admission diagnosis, in 2018 for tuberculosis patients, and in 2023 for HA COPD patients. The lowest HA CDI incidence with a stable trend during the observed period was reported among lung cancer patients (Graph 2).
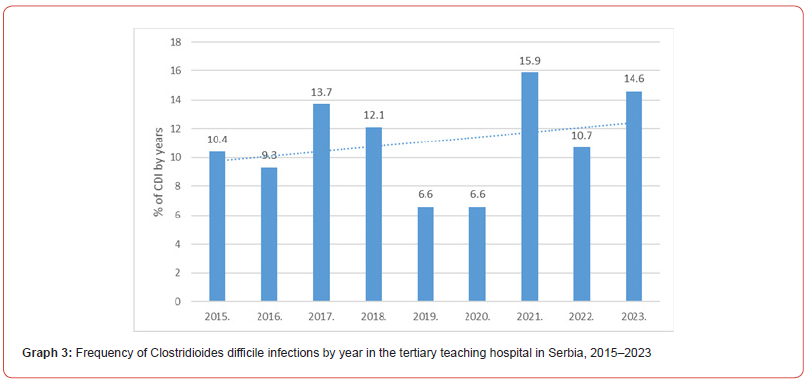
During the observed nine-year period, the frequency of HA CDI patients by the year showed a significant difference (χ²=28.687, df=8, p<0.001), with the lowest number of cases in 2019 and 2020 (24 cases, or 6.6% (24/364)), and the highest number in 2021 (58 cases, 15.9% (58/364)) (Graph 3).
HA CDI showed significant differences by Clinics (p<0.001). Distribution of HA CDI patients according to I, II, III, IV, V, and combined Clinic were 75 (20.7%), 80 (22.0%), 132 (36.4%), 21 (5.8%), 21 (5.8%), 29 (8.0%), and 26 (7.2%), respectively.
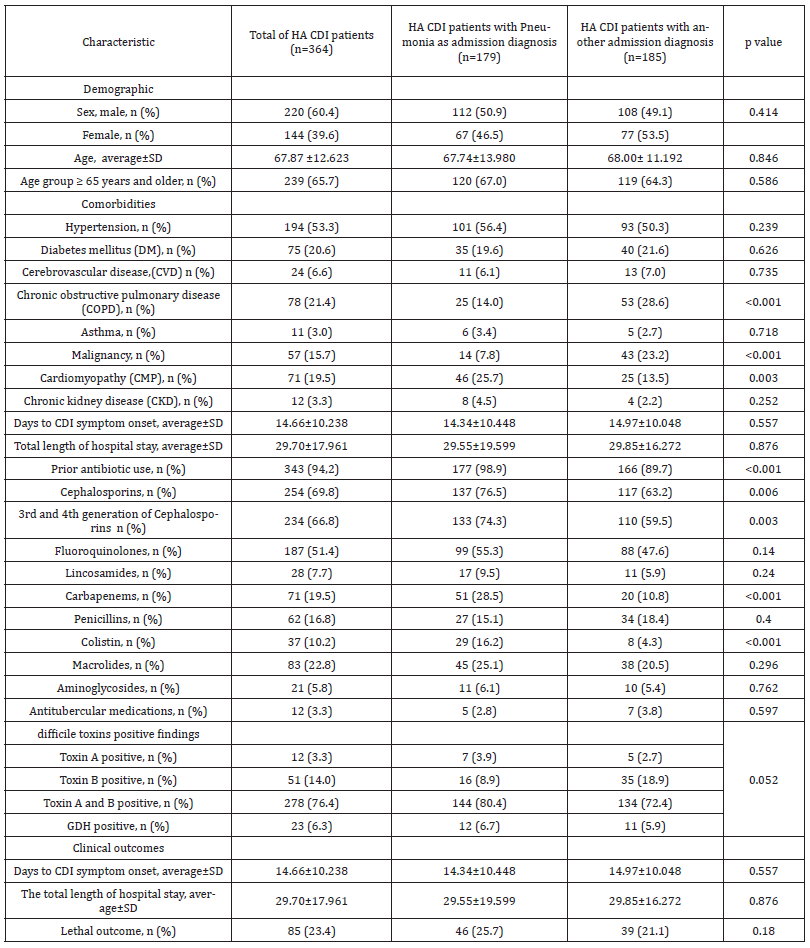
Baseline demographic and clinical characteristics of HA CDI patients are presented in Table 1.
Males represent 60.4% (220/364) of HA CDI patients, without significant differences between CAP and other admission diagnosis.
The average age of HA CDI patients was 68 (67.87±12.623), and 65.7% (239/364) were 65 years or older. Significant differences by average age or age group according to admission diagnosis were not observed.
Among all HA CDI patients, the highest frequency was reported for hypertension (53.3%), diabetes mellitus (DM) (20.6%), chronic obstructive pulmonary disease (COPD) (21.4%), cardiomyopathy (CMP) (19.5%), and malignancy (15.7%). Compared to patients with other admission diagnoses, patients with CAP had a significantly higher frequency of CMP (25.7% vs 13.5%, respectively; p=0.003) (Table 1).
Prior antibiotic use was reported in 94.2% (343/364) of all HA CDI patients. Patients with CAP had a significantly higher percentage of prior antimicrobial consumption than patients with another admission diagnosis (98.9% vs 89.7%, p<0.001).
Frequencies of most common classes of antibiotics used the prior onset of CDI symptoms among all HA CDI patients were: cephalosporins (69.8%), 3rd and 4th generation of cephalosporins (66.8%), fluoroquinolones (51.4%), macrolides (22.8%), carbapenems (19.5%), and 16.8% for penicillins. According to antimicrobial classes, prior use was significantly higher for 3rd and 4th generation of cephalosporins (74.3% vs 59.5%, p=0.003), carbapenems (28.5% vs 10.8%, p<0.001), and colistin (16.2% vs 4.3%, p<0.001) among CAP HA CDI patients compared to other admission diagnosis (Table 1).
Among all HA CDI cases, 278 (76.4%) were both toxin A and toxin B positive, 51 (14.0%) were only toxin B positive, and 12 (3.3%) were only toxin A positive. Significant differences between toxin types and admission diagnosis were not observed.
The average duration of hospitalization prior to the development of CDI symptoms was 15 days (14.66±10.238), while the total length of hospital stay for all HA CDI patients was 30 days (29.70±17.961). Significant differences in the average duration of hospitalization prior to the onset of CDI symptoms and in the total duration of hospitalization between groups were not observed (Table 1).
Table 1:Baseline demographic and clinical characteristics of healthcare-associated Clostridioides difficile infections in the tertiary university hospital in Serbia, 2015–2023
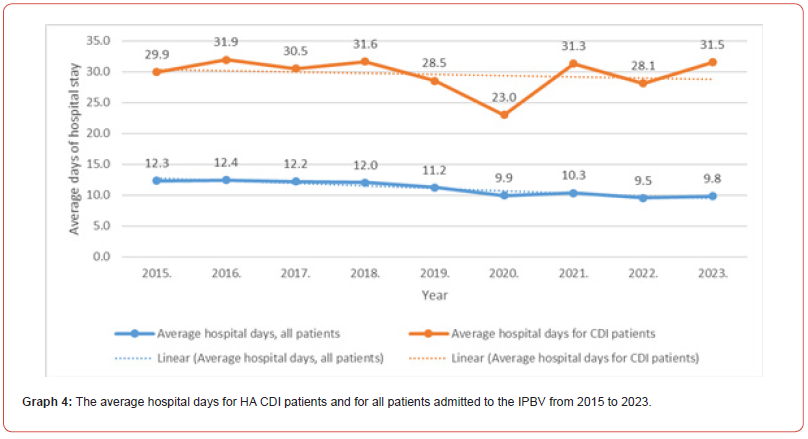
The average duration of hospitalization for all IPBV patients from 2015 to 2023 was 11 days (11.066±1.129), with an observed decreasing trend during the period (R2=0.8786). The total length of hospital stay for all HA CDI patients was 30 days (29.70±17.96) without significant changes during the period (R2=0.0377). (Graph 4).
In-hospital mortality (all causes) among HA CDI patients was reported in 85 (23.4%) of cases. No significant differences were observed in death outcomes among HA CDI patients between admission diagnosis groups.
Discussion
HA CDI could become a more important public health concern in developing countries such as Serbia due to the high prevalence of multi-drug resistant strains in our region [25-27].
There is an increasing trend in antimicrobial consumption [25] and an ageing population, where, according to the 2021 census data, 22% of the population was 65 years or older [28].
The highest HA CDI incidence is reported in tertiary hospitals [18]. Observed rates in our study were higher than the average in European hospitals [18] because we analyzed data from tertiary hospitals. We also reported an increase in HA CDI incidence in our tertiary hospital over nine years. The frequency of HA CDI cases was significantly higher in 2021 (15.9%), while were the lowest in 2019 (6.6%) and 2020 (6.6%). The observed increase among pulmonology patients is probably a consequence of the COVID-19 pandemic during the 2019/2020 season, followed by the rise in antibiotic consumption [30-33].
In our study population, HA CDI was significantly common among males (60.4% vs. 39.4%), while most other studies reported higher CDI incidence among females [8, 34, 35].
In our sample, HA CDI was more common among males due to the higher frequency of males among patients with pneumonia or other chronic respiratory diseases such as COPD or lung cancer [36].
It is well known that the use of antibiotics among elderly persons with multiple comorbidities was significantly associated with HA-CDI [7-17, 24, 36].
Among our HA CDI patients, 65.7% were aged ≥65 years, and 94.2% received antibiotics before developing CDI. The risk of developing CDI is the highest (8 to 10-fold higher) during the period of antimicrobial therapy and stay increased (3-fold higher) in the next two months after antimicrobial treatment [37].
Recently published results highlight the influence of piperacillin/tazobactam, meropenem, vancomycin, ciprofloxacin, ceftriaxone, and levofloxacin as antibiotics with increased risk [13].
In our study, almost 76.5% of pneumonia patients with HA CDI had prior use of cephalosporins, 55.3% fluoroquinolones, 25.1% macrolides, 28.5% carbapenems, and 15.1% penicillins. Patients with CAP significantly commonly use 3rd and 4th generation of cephalosporins, carbapenems, and colistin, compared to nonpneumonia admission diagnosis due to CAP complicated with HA infections with MDR Acinetobacter baumannii, Klebsiella pneumoniae or P. aeruginosa.
According to the results from a worldwide point prevalence survey of hospitals in the EU, ceftriaxone was the most commonly used antibiotic, with observed significant differences between Northern and Eastern Europe (from 2.5% to 24.8%, respectively) [24, 38].
Similar to previous reports from our country, cephalosporins were the most commonly used antibiotics in our hospitals, while penicillin use was low [24, 26].
According to the results of prior studies, patients with solid organ malignancy, neutropenia, diabetes mellitus (DM), chronic kidney disease (CKD), and chronic respiratory patients with tuberculosis and chronic obstructive pulmonary disease (COPD) have a higher risk for CDI [8, 12,39, 40].
In our sample, the highest frequency of comorbidities was reported for hypertension, COPD, DM, and CMP. Patients with pneumonia at admission significantly commonly had CMP, while other patients without pneumonia had more often COPD or malignant diseases. The observed results are in line with those of prior studies from developed countries [6-8, 14, 41].
The average duration of hospital stay prior to the development of CDI symptoms was 15 days, with no significant differences by Clinic type (internal medicine, surgery). Among comorbidities, only patients with COPD had a significantly lower average duration of hospitalization prior to CDI onset, around 12 days, compared to others (12.10±6.911 vs 15.36±10.863). Our results were similar to those of studies performed in developed countries [41].
HA CDI increase the duration of hospitalization and readmission rates and negatively impacts patient care and healthcare costs. According to Hirsch et al. [42], CDI is associated with an increased median length of stay of 5 days and an additional $27,891 in hospital charges per admission. In the nationwide analysis in Japan [43], the median excess in length of hospital stay attributable to CDI and recurrent CDI was three days and 6.5 days, respectively.
Similar results were confirmed in other studies, where CDI was associated with €9000 of extra costs, €7800 of higher reimbursements, and 6.4 days extra length of stay [44].
Zhang et al. reported that patients with CDI had $24,205 higher costs than patients without CDI over a 6-month follow-up period [45].
In our study, the average total hospital stay for our HA CDI patients was significantly longer than the average length of stay for all hospitalized patients during the observed period (30 days vs. 11 days).
Although we reported increasing HA CDI incidence, all-cause mortality among HA CDI patients showed no changes during nine years. CDI mortality rates showed differences by region of the world, from 5 to 20%, and can be significantly higher in developing countries [19,22, 43, 46,47].
A population-based cohort study showed that CDI was associated with a 3-to 7-fold higher mortality rate than the matched controls [48].
Differences in mortality rates between countries can be explained by healthcare quality, availability of novel antimicrobial therapy, and strict implementation of infection control policies [17, 20]. In our study, the percentage of lethal outcomes among patients with HA CDI (all-cause mortality) was 23.4%. Antibiotics available for treating CDI in our country are metronidazole and vancomycin.
However, in developed countries, the use of fidaxomicin over vancomycin and metronidazole for initial treatment due to its lower recurrence rate is recommended according to the Infectious Disease Society of America/Society for Healthcare Epidemiology of America (IDSA/SHEA), American College of Gastroenterology (ACG) and the European Society of Clinical Microbiology and Infectious Disease (ESCMID)guidelines.
Fidaxomicin belongs to the macrocyclic lactones (macrolide) class of antimicrobial agents. It has a narrow spectrum of antibacterial activity and effectively targets C. difficile without much disruption of the remaining colonic flora [21, 49, 50].
Active surveillance and further epidemiological studies of the HA CDI burden among pulmonology patients are needed to improve preventive strategies. Antibiotic stewardship, decreasing the length of hospital stay, early detection of CDI, and strict implementation of prevention and control policies in our hospital are crucial until new drugs and innovative vaccines against C. difficile become available [17, 21, 49-52].
Limitation of Study
This retrospective observational study was performed according to the Active Surveillance C. difficile questionnaire, and data about the severity of clinical manifestation and lethal outcomes directly influenced by CDI were not reported.
Further prospective epidemiological studies among this population are necessary to improve infection and control policies and plan for novel preventive and therapy options.
Conclusion
The incidence of HA CDI among pulmonology tertiary hospital patients increased from 2015 to 2023, particularly after the COVID-19 2019/2020 season. Most of our HA CDI patients were elderly males who had previously consumed broad-spectrum antibiotics. Hospitalization longer than 15 days was a significant risk factor for our CDI patients.
Active surveillance, antibiotic stewardship, decreasing the length of hospital stay, early detection of CDI, and strict implementation of prevention and control policies in our hospital are crucial until new therapy options against C. difficile become available.
Conflict of Interest
Authors declare no conflict of interest.
Acknowledgment
None..
-
Jelena Djekic Malbasa , Tomi Kovacevic, Branislav Tušek, Anika Trudić, Vladimir Stojšić, et al. Healthcare-associated Clostridioides difficile infections among pulmonology patients. Archives in Respiratory & Pulmonary Medicine. 1(3): 2024. ARPM.MS.ID.000515.
-
Tuberculosis, Poor adherence, Associated factors, Medication, TB clinic, Public health, Mettu Karl Referral Hospital, Ethiopia
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.