Mini Review
Mini Review
Changes in the Epidemiology and Surveillance of Viral Respiratory Diseases in the Madrid Region: Beyond Covid-19
Arce Arnáez Araceli and Íñigo Martínez Jesús*
Directorate General of Public Health, Regional Ministry of Health of Madrid, Madrid, Spain
Íñigo Martínez Jesús, Directorate General of Public Health, Regional Ministry of Health of Madrid, Madrid, Spain
Received Date:November 27, 2023; Published Date:December 14, 2023
Abstract
Respiratory infections are the second cause of morbidity and mortality in the world and the first cause of infectious disease in Spain and Europe. After the arrival of COVID-2019, with great impact on all health and social indicators, the non-pharmacological measures taken limited the incidence of other respiratory viruses by making their transmission difficult. Derived from this pandemic situation, the population has had a greater susceptibility to other respiratory viruses, since it could not acquire natural immunity as the circulation of these viruses was hampered. The pandemic situation and the control measures implemented initially had a favorable impact on the control of other respiratory diseases, but these increased in 2022. Co-circulation of respiratory viruses may occur and produce almost simultaneous epidemic peaks in the winter season. This simultaneous transmission poses important challenges in the clinical management of patients and in the planning of a possible care overload, both at the outpatient and hospital levels. Aging and chronicity associated with increased life expectancy suggest that acute respiratory infections will continue to be highly prevalent in the coming years. Added to this are respiratory syncytial virus (RSV) infections or other viruses that mainly affect the younger paediatric population population (0 to 4 years old) and are currently the leading cause of lower respiratory tract infection and hospitalization in infants. After the pandemic, it has been necessary to readapt the epidemiological surveillance systems against viral infections of the respiratory system, maintaining an adequate balance between sentinel and classic systems.
Keywords:COVID-19; virus diseases; respiratory syncytial virus; human; influenza; public health surveillance; sentinel surveillance; epidemiology
Abbreviations:ARI: Acute Respiratory Infections; RSV: Respiratory Syncytial Virus; NPIs: Non-Pharmacological Interventions; SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2
Introduction
In recent decades, respiratory infections have been the second cause of morbidity and mortality in the world and the first cause of infectious disease in Spain and Europe [1]. In an era of new risks of emerging diseases, the transmission of viruses that cause acute respiratory diseases continues to constitute a challenge because they generate non-specific pathology, diagnostic tests are not always performed to understand their aetiology and only supportive treatments are available, non-curative [2]. In an attempt to mitigate the spread of the COVID-19 pandemic, most countries adopted a heterogeneous series of non-pharmacological interventions (NPIs) that included confinements and restrictions on population mobility, limitation of activity in social centres and use of masks [3]. These interventions, which were in force even after vaccines and antivirals became available, together had a positive effect in terms of morbidity and mortality and managed to prevent the overload of health systems from being of greater magnitude [4- 7]. The measures used to try to control the pandemic produced a great social impact and, specifically considering the health field, very relevant effects were observed, overall negative, on the use of health services [8,9]. These measures also contributed to the modification of the epidemiology of other infectious diseases, effects that continue to take place in 2023. In general. NPIs limited the incidence of other pathogens, especially respiratory viruses, by making their transmission difficult [10-22] but at the cost of reducing natural protection against many communicable diseases.
The effects of the withdrawal of NPIs against COVID-19 on the epidemiology of other diseases
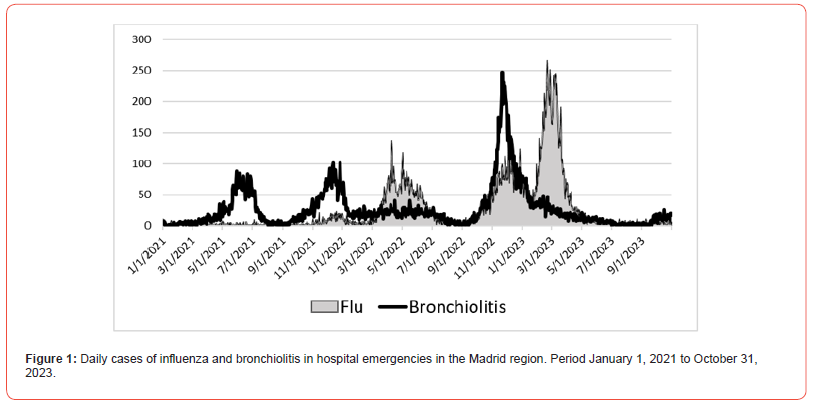
The withdrawal of the NPIs by the different countries occurred when it was considered that the immune status of the population against COVID-19 was adequate, due to the sum of the natural protection acquired after the disease and that resulting from vaccination. This moment has been described as the calm before the storm, since there had been unusually low incidence rates of certain communicable diseases that were a consequence of a decrease in the opportunity to achieve natural immunity against these pathogens and therefore represented the emergence of a larger group of susceptible individuals [23]. In the Madrid region, after the lifting of these measures, the incidence of flu, legionellosis and tuberculosis increased significantly during 2022, with an increase of 32% in sporadic cases of legionellosis and an 8% increase in the incidence of tuberculosis. [24]. The incidence of flu in that year was 14 times higher than in 2021, but without reaching the figures of pre-pandemic years, a trend that continues during the first half of 2023. Respiratory syncytial virus (RSV) cases in children under 2 years of age have also increased in the 2022-2023 season, recovering the magnitude and seasonality that it maintained in the pre-pandemic stage [25]. The modification of the temporal presentation and the proximity of the epidemic peaks is observed in Figure 1, which includes the series of cases of influenza (n=27,225) and bronchiolitis (n=27,506) treated in hospital emergencies in the Madrid region from the beginning of 2021 to November 2023.
The high effort of health systems to adapt to the COVID-19 pandemic was also associated with the strengthening of epidemiological surveillance of this disease. In the current, post-pandemic stage, it has been necessary to readjust the epidemiological surveillance systems to the new situation, since cocirculation of respiratory viruses can occur, and this simultaneous transmission poses important challenges for surveillance, in addition to the management of the patients and for planning a possible care overload, both at the outpatient and hospital levels. Aging and chronicity associated with increased life expectancy suggest that acute respiratory infections will continue to present high levels of incidence in the coming years. Furthermore, some infections, such as those caused by VRS, mainly affect the younger paediatric population (0 to 4 years) and are currently the leading cause of lower respiratory tract infection in infants in the Madrid region.
Lower and upper respiratory tract infections can be caused by various types of viruses, including parainfluenza, adenovirus, rhinovirus, bocavirus and human metapneumovirus. In addition to the clinical impact on patients and their quality of life, acute viral respiratory infections (ARIs), when they occur at epidemic peaks, can compromise healthcare capacity and consequently lead to a significant overload in the consumption of health resources. Thus, for example, the confluence of the three viruses, influenza, RSV and COVID-19, meant in the winter of 2022 an increase of 40% in cases treated in emergencies in Spain [26]. In the Madrid region, episodes treated in the emergency room due to influenza increased by 346% between November and April 2022-2023 compared to the same period in 2021-2022 and bronchiolitis episodes increased by 84% (Figure 1).
Adaptation of surveillance of acute viral respiratory infections incorporating sentinel systems
These types of infections are a priority for surveillance systems. After three years of pandemic, with different variants of SARS-CoV-2 that have emerged and predominated in the different epidemic waves, it is still necessary to continue characterizing the virus and assess whether its new mutations affect vaccine effectiveness, including new vaccines of multivalent composition that incorporate new variants. The influenza virus causes annual seasonal epidemics, usually in the winter months, and has significant pandemic potential, as occurred in 2009. Antigenic changes in the surface proteins of the virus are the origin of the annual epidemics and the reason for the update annual vaccinations. The RSV causes lower respiratory tract infections, mainly bronchiolitis, in infants under 1 year of age, without forgetting the impact that RSV infection has on adults and especially on the elderly. It also generates seasonal epidemic peaks, generally prior to the circulation of the influenza virus. RSV infections represent a significant healthcare burden every year, both in primary care services and in hospitals, including visits to the emergency room, occupancy of hospitalization floors and paediatric intensive care units [27-29].
Due to the high incidence, the associated morbidity and mortality of these viruses and the capacity to evolve, the WHO and the ECDC recommend that countries monitor the co-circulation of RSV, influenza viruses and SARS-CoV-2, and their genetic and phenotypic characteristics, through surveillance, sentinel and non-sentinel systems [30]. Traditional surveillance systems include notifiable diseases and surveillance based on monitoring the number of health care episodes in primary care and hospital emergencies, aimed at specific pathologies. During the pandemic, a great effort was made in surveillance to carry out an epidemiological survey of each patient and study epidemic outbreaks. Given the very high number of cases -2,005,382 confirmed cases for a population of 6,744,456 during the period of Public Health Emergency of International Importance-, after the most acute phase of the pandemic, the need to implement a sentinel system was promoted for syndromic surveillance of ARIs. The purpose is to monitor the incidence and epidemiological and microbiological characteristics of respiratory infections caused by the best-known circulating pathogens in the community (flu, COVID-19 and RSV).
Since the end of 2020, the Madrid region adapted the influenza sentinel surveillance system that it had been carrying out for the last 25 years and began syndromic surveillance of ARI, following international recommendations and providing its information at the state level [31]. In July 2023, the Strategy for the integration of COVID-19 in the surveillance and control of acute respiratory infections in the Madrid region was published, which eliminates the individualized declaration of all exhaustively identified COVID-19 cases and establishes surveillance of COVID-19, influenza and RSV through the sentinel system [32]. Surveillance is carried out in both primary care and hospital care and is maintained during all months of the year. To monitor the incidence, the number of episodes detected in primary care consultations and the number of urgent hospital admissions due to ARI are collected daily. On the other hand, to know the characteristics of the cases, the clinical and evolution data, the risk history and the vaccination status of the cases detected are collected one day a week and a respiratory sample is taken for testing for detection of respiratory viruses. In addition, the system provides the data required by the national sentinel surveillance system [33].
In the 2023-2024 season, 10% of the population of the region of Madrid is monitored in primary care and 22.6% in the hospital setting through a network of sentinel centres made up of 30 health centres and 3 hospitals. The participation of these centres is key to having high-quality information that allows us to know the epidemiological situation, identify changes that may require the early adoption of public health measures and evaluate the effectiveness and impact of preventive measures. Updated status reports are published every week of the year.
Prevention measures for viral respiratory diseases: infection control and immunization
The general population is susceptible throughout life to becoming infected by different respiratory viruses and to suffering repeated infections from the same agent. Respiratory viruses are transmitted between people by direct or indirect interaction, through aerosols or droplets through the air. The prevention of this transmission or spread of viruses can be done with nonpharmacological infection control measures (use of a mask, personal protective equipment, physical distancing between people), but fundamentally through vaccination or immunization (of groups of risk and health professionals), which are the most effective tools [34]. Vaccination, both for flu and COVID-19, is aimed mainly at those people who are at greater risk of presenting complications, or those who can transmit to vulnerable others, in addition to personnel who perform essential services for the community.
Recently, in 2023, the marketing of a monoclonal antibody, nirsevimab, has been authorized for the prevention of lower respiratory tract disease caused by RSV in neonates and infants during their first season of exposure to the virus. In the Madrid region, RSV infection mainly affects children under one year of age and the majority of children admitted are under 3 months. The use of nirsevimab at the population level pursues the objective of primary prevention in pediatric age. Between October 1, 2023 and March 31, 2024, a population immunization campaign is being implemented by administering the monoclonal antibody nirsevimab to all infants under 6 months of age at the beginning of the RSV season and to born during the season [35], with preliminary results that point to high effectiveness in preventing severe forms that require hospitalization.
Acknowledgement
We would like to thank Madrid Surveillance Network Centre of Madrid Region without whose continuous work of epidemiological surveillance the preparation of this manuscript would not have been possible.
Conflicts of interest
No conflict of interes
References
- Ferkol T, Schraufnagel D (2014) The global burden of respiratory disease. Ann Am Thorac Soc 11(3): 404-406.
- (2007) World Health Organization. Infection prevention and control of epidemic-and pandemic-prone acute respiratory diseases in health care: WHO interim guidelines.
- Shen Y, Powell G, Ganser I, Zheng Q, Grundy C, et al. (2021) Monitoring non-pharmaceutical public health interventions during the COVID-19 pandemic. Sci Data 8(1): 225-230.
- Askitas N, Tatsiramos K, Verheyden B (2021) Estimating worldwide effects of non-pharmaceutical interventions on COVID-19 incidence and population mobility patterns using a multiple-event study. Sci Rep 11(1): 1972-1980.
- Mendez Brito A, El Bcheraoui C, Pozo Martin F (2021) Systematic review of empirical studies comparing the effectiveness of non-pharmaceutical interventions against COVID-19. J Infect 83(3): 281-293.
- Flaxman S, Mishra S, Gandy A, Unwin HJT, Mellan TA, et al. (2020) Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 584(7820): 257-261.
- Walker PGT, Whittaker C, Watson O, Baguelin M, Ainslie KEC, et al. (2020) Report 12: the global impact of COVID-19 and strategies for mitigation and suppression. Imperial College London, UK.
- World Health Organization (2021) COVID-19 continues to disrupt essential health services in 90% of countries. Geneva: WHO.
- Moynihan R, Sanders S, Michaleff ZA, Scott AM, Clark J, et al. (2021) Impact of COVID-19 pandemic on utilisation of healthcare services: a systematic review. BMJ Open 11(3): e045343-e045350.
- van de Berg S, Charles T, Dörre A, Katz K, Böhm S (2023) Epidemiology of common infectious diseases before and during the COVID-19 pandemic in Bavaria, Germany, 2016 to 2021: an analysis of routine surveillance data. Euro Surveill 28(41): 2300030-2300035.
- Hirae K, Hoshina T, Koga H (2023) Impact of the COVID-19 pandemic on the epidemiology of other communicable diseases in Japan. Int J Infect Dis 128(1): 265-271.
- Bright A, Glynn Robinson AJ, Kane S, Wright R, Saul N (2020) The effect of COVID-19 public health measures on nationally notifiable diseases in Australia: preliminary analysis. Commun Dis Intell (2018) 44(1): 1-16.
- Lai CC, Chen SY, Yen MY, Lee PI, Ko WC, et al. (2021) The impact of the coronavirus disease 2019 epidemic on notifiable infectious diseases in Taiwan: a database analysis. Travel Med Infect Dis 40(1): 101997-101999.
- Rybak A, Levy C, Angoulvant F, Auvrignon A, Gembara P, et al. (2022) Association of nonpharmaceutical interventions during the COVID-19 pandemic with invasive pneumococcal disease, pneumococcal carriage, and respiratory viral infections among children in France. JAMA Netw Open 5(6): e2218959-e2218963.
- Redlberger Fritz M, Kundi M, Aberle SW, Puchhammer Stöckl E (2021) Significant impact of nationwide SARS-CoV-2 lockdown measures on the circulation of other respiratory virus infections in Austria. J Clin Virol 137(1): 104795-104798.
- Hatoun J, Correa ET, Donahue SMA, Vernacchio L (2020) Social distancing for COVID-19 and diagnoses of other infectious diseases in children. Pediatrics 146(4): e2020006460-e2020006464.
- Chen B, Wang M, Huang X, Xie M, Pan L, et al. (2021) Changes in incidence of notifiable infectious diseases in China under the prevention and control measures of COVID-19. Front Public Health 9(1): 728768-728770.
- Huh K, Jung J, Hong J, Kim M, Ahn JG, et al. (2021) Impact of nonpharmaceutical interventions on the incidence of respiratory infections during the coronavirus disease 2019 (COVID-19) outbreak in Korea: a nationwide surveillance study. Clin Infect Dis 72(1): e184-e191.
- Launay T, Souty C, Vilcu AM, Turbelin C, Blanchon T, et al. (2021) Common communicable diseases in the general population in France during the COVID-19 pandemic. PLoS One 16(10): e0258391-e0258394.
- Steffen R, Lautenschlager S, Fehr J (2020) Travel restrictions and lockdown during the COVID-19 pandemic-impact on notified infectious diseases in Switzerland. J Travel Med 27(8): taaa180-185.
- Olsen SJ, Winn AK, Budd AP, Prill MM, Steel J, et al. (2021) Changes in influenza and other respiratory virus activity during the COVID-19 pandemic - United States, 2020–2021. MMWR Morb Mortal Wkly Rep 70(29): 1013–1019.
- Müller O, Razum O, Jahn A (2021) Effects of non-pharmaceutical interventions against COVID-19 on the incidence of other diseases. Lancet Reg Health Eur 6(1): 100139-100141.
- Oh KB, Doherty TM, Vetter V, Bonanni P (2022) Lifting non-pharmaceutical interventions following the COVID-19 pandemic - the quiet before the storm?. Expert Rev Vaccines 21(11):1541-1553.
- (2023) General Directorate of Public Health. Community of Madrid. Morbidity due to notifiable diseases in the Community of Madrid, year 2022 (in Spanish). Boletín Epidemiológico de la Comunidad de Madrid; Nº Volumen 28. Septiembre 2023.
- (2023) General Directorate of Public Health. Community of Madrid. Epidemiological situation of the Respiratory Syncytial Virus (RSV). Madrid's community. Seasons 2016/17 to 2022/23 (in Spanish). Boletín Epidemiológico de la Comunidad de Madrid; Nº Volumen 28. Agosto 2023.
- (2022) Spanish Society of Pediatric Emergencies. Statement from the SEUP regarding the increase in care volume in emergency areas (in Spanish). Madrid.
- Vila J, Lera E, Peremiquel Trillas P, Martínez L, Barceló I, et al. (2022) Management of hospitalized respiratory syncytial virus bronchiolitis in the pediatric ward in Spain: assessing the impact of a new clinical practice protocol. Pediatr Drugs 24(1): 63-71.
- Li Y, Johnson EK, Shi T, Campbell H, Chaves SS, et al. (2021) National burden estimates of hospitalisations for acute lower respiratory infections due to respiratory syncytial virus in young children in 2019 among 58 countries: a modelling study. Lancet Respir Med 9(2): 175-185.
- (2022) European Centre for Disease Prevention and Control. Intensified circulation of respiratory syncytial virus (RSV) and associated hospital burden in the EU/EEA. 12 December 2022. Stockholm (Sweden).
- (2023) European Centre for Disease Prevention and Control. Reporting Protocol for integrated respiratory virus surveillance.
- (2023) General Directorate of Public Health. Community of Madrid. Sentinel surveillance of acute respiratory infections (ARI) (in Spanish).
- (2023) General Directorate of Public Health. Community of Madrid. Strategy for the integration of COVID-19 in the surveillance and control of acute respiratory infections in the Community of Madrid (in Spanish).
- (2023) Carlos III Health Institute. Protocol for sentinel surveillance of Acute Respiratory Infection (ARI) in Primary Care in Spain 2023-24 Season (in Spanish). Protocolo Vigilancia centinela de IRAs_2023-24_v.27092023.pdf (isciii.es).
- Mazur NI, Terstappen J, Baral R, Bardají A, Beutels P, et al. (2023) Respiratory syncytial virus prevention within reach: the vaccine and monoclonal antibody landscape. Lancet Infect Dis 23(1): e2-e21.
- (2023) General Directorate of Public Health. Community of Madrid. Technical document on Immunization against Respiratory Syncytial Virus (RSV) in infants in the Community of Madrid in the 2023-2024 season (in Spanish).
-
Arce Arnáez Araceli and Íñigo Martínez Jesús*. Changes in the Epidemiology and Surveillance of Viral Respiratory Diseases in the Madrid Region: Beyond Covid-19. Archives in Respiratory & Pulmonary Medicine. 1(3): 2023. ARPM.MS.ID.000512.
-
COVID-19; virus diseases; respiratory syncytial virus; human; influenza; public health surveillance; sentinel surveillance; epidemiology
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.