Case Report
Case Report
Management of Severe Maternal Hyponatremia Secondary to Pre-Eclampsia
Michelle Joy Wang1,2*, Allyson Larosa1,2, Nisha Kumar3, Wissam Mustafa3 and Christina Yarrington1,2
1Boston University School of Medicine, Boston, MA
2Department of Obstetrics and Gynecology, Boston Medical Center, Boston, MA
3Department of Anesthesia, Boston Medical Center, Boston, MA.
Michelle Joy Wang, Boston University School of Medicine, Department of Obstetrics and Gynecology, Boston Medical Center, Boston, MA, USA.
Received Date: May 22, 2025; Published Date: June 02, 2025
Annotation
Objective: Severe maternal hyponatremia is a rare complication of preeclampsia in pregnant patients with a range of proposed etiologies including syndrome of inappropriate antidiuretic hormone and low effective circulating blood volume causing an increase in antidiuretic hormone
Case Report: A 32-year-old G1P0 presented at 35 weeks’ gestation to her primary obstetric provider with mild range blood pressures and an incidental sodium level of 123mEq/L. The patient was diagnosed with preeclampsia with an atypical severe feature of hyponatremia. When her sodium nadired to 118mEq/L, anesthesia, neonatology, and renal specialists huddled to discuss the risks of delivery. She ultimately developed a non-reassuring category 2 fetal heart pattern and was delivered by cesarean section. Postoperatively, her sodium rapidly normalized with minimal intervention.
Conclusion: Maternal hyponatremia is a rare though serious complication of preeclampsia that warrants close inpatient management and a balance of maternal, neonatal, and obstetric considerations.
Keywords: Hyponatremia; Pre-eclampsia; Perioperative Obstetric Care
Introduction
A reduction of serum sodium by as much as 5mEq/L is expected as normal physiologic response to pregnancy [1]. However, when serum sodium decreases beyond this, underlying pathologic causes should be considered, including preeclampsia. Hyponatremia has been documented to affect as many as 9.7% of patients with preeclampsia [2-4]. Researchers postulate that vasopressinase secretion or production may be impaired in the setting of preeclampsia or that decreased circulating volume seen in preeclampsia in the setting of nephrotic level protein loss ultimately leads to increased ADH secretion [4-7]. Hyponatremia in pregnancy generates significant perinatal risks including maternal seizure or coma, and central pontine myelinolysis upon sodium correction and neonatal seizure or coma and hypotonia [8-9]. We present the following case to remind the obstetric anesthesia community about the potential severity of maternal hyponatremia and the interdisciplinary approach required for intrapartum management.
Case Presentation
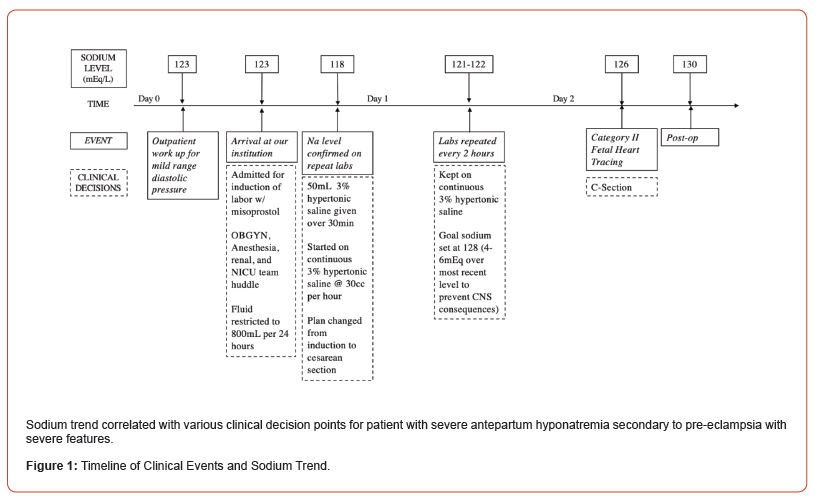
32-year-old G1P0 presented at 35 weeks gestation to her primary obstetric provider with mild range diastolic blood pressures and an incidental sodium level of 123mEq/L (see Figure 1). Further work-up inpatient demonstrated a urine protein to creatinine ratio of 7.7, and sodium of 122mEq/L and pitting edema. The patient was diagnosed with preeclampsia with an atypical severe feature of hyponatremia and recommended to for delivery via induction of labor. When her sodium nadired to 118mEq/L during her induction, anesthesia, neonatology, and renal specialists huddled to discuss the risks of delivery. A formal huddle between maternal fetal medicine, anesthesia, nephrology, and nursing highlighted the key challenges in patient management. First, her serum sodium was worsening. Second, as preeclampsia was the leading diagnosis, only delivery would restore normal physiology. Cesarean section would expedite delivery but potentially create a large postoperative fluid redistribution and perioperative hyponatremia is a known risk factor for mortality and morbidity [10]. Induction with oxytocin could mimic the effects of antidiuretic hormone and worsen the patient’s condition. Furthermore, if this patient were to seize, discernment in etiology between eclampsia and hyponatremia would be impossible; thus, seizure treatment would need to target both underlying causes.
The efficacy of magnesium for seizure prevention in this patient with severe electrolyte abnormalities were another unknown. Finally, if maternal sodium levels were not corrected, the risks of neonatal seizure and hypotonia risks at delivery were high. The multidisciplinary team recommended stopping her induction and correcting the hyponatremia with hypertonic saline and fluid restriction with plan for cesarean delivery once the patient’s sodium had increased to 128mEq/L. The following day, her sodium level improved to 126mEq/L. However, the fetal heart rhythm demonstrated diminished variability and late decelerations; thus, the decision was made to proceed with an urgent cesarean. The surgery was complicated by a hemorrhage with quantitative blood loss of 1161 mL, which was managed with additional intramuscular oxytocin and 1 unit of pRBC. Crystalloid resuscitation was minimal. Neonatal Apgar scores were 8 and 9 at 1 and 5 minutes, respectively. The neonate was transferred to the NICU for close observation. The neonatal initial labs were significant for umbilical cord serum sodium of 127mEq/L and arterial blood pH of 7.18. Following delivery, the 3% hypertonic saline was discontinued, and the patient’s sodium level improved to 130mEq/L and remained stable upon repeat testing on postoperative day one. The patient otherwise had an uneventful postoperative course and was ultimately discharged on postoperative day 4.
Discussion
Sodium levels should be optimized as much as possible in the interest of reducing maternal morbidity; however, the perinatal team must remember that sodium correction relies on volume restriction with implicit consequences to placental perfusion. To this end, it is important to remember that a prolonged induction course or prolonged course of gradual electrolyte correction will almost inevitably lead to placental hypoperfusion and subsequent decompensation of fetal status prompting cesarean delivery. The antepartum multidisciplinary team caring for a patient with hyponatremia must thus be prepared for either maternal or neonatal resuscitation at the time of delivery.
Conclusion
Hyponatremia is a rare but highly morbid potential complication of preeclampsia that generates a complex intersection of perinatal and perioperative risks that obstetric anesthesiologists should be cognizant of and prepared for.
Acknowledgements
None.
Conflicts of Interest
The authors have no conflicts of interest relevant to this article.
References
- Davison JM, Gilmore EA, Durr J, Robertson GL, Lindheimer MD (1984) Altered osmotic thresholds for vasopressin secretion and thirst in human pregnancy. Am J Physiol 246(1, pt 2): F105-109.
- Abalos E, Cuesta C, Grosso AL, Chou D, Say L (2013) Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol 170(1):1-7.
- Razavi AS, Chasen ST, Gyawali R, Kalish RB (2017) Hyponatremia associated with preeclampsia. J Perinat Med 45(4).
- Sandhu G, Ramaiyah S, Chan G, Meisels I (2010) Pathophysiology and management of preeclampsia-associated severe hyponatremia.Am J Kidney Dis 55(3): 599-603.
- Wilson HJ, Shutt LE (2008) Syndrome of inappropriate ADH secretion in a woman with preeclampsia.Obstet Anesth Dig 28(2):121-122.
- Camara-Lemarroy CR, de Leon-Cruz A, Rodriguez-Gutierrez R, Galarza-Delgado DA (2013) Severe hyponatremia associated with pre-eclampsia. Gynecol Endocrinol 29(8): 801-803.
- Magriples U, Laifer S, Hayslett JP (2001) Dilutional hyponatremia in preeclampsia with and without nephrotic syndrome.Am J Obstet Gynecol 184(2): 231-232.
- Janga KC, Khan T, Khorolsky C, Greenberg S, Persaud P (2015) A rare case of central pontine myelinolysis in overcorrection of hyponatremia with total parenteral nutrition in pregnancy. Case Rep Nephrol 2015: 940807.
- Kahramanoglu I (2014) Preeclampsia as a Rare Cause of Hyponatremia.Gynecol Obstet (Sunnyvale) 04(05).
- Leung AA, McAlister FA, Rogers SO Jr, Pazo V, Wright A, Bates DW, et al. (2012) Preoperative hyponatremia and perioperative complications. Arch Intern Med 172(19): 1474-1481.
-
Michelle Joy Wang*, Allyson Larosa, Nisha Kumar, Wissam Mustafa and Christina Yarrington. Management of Severe Maternal Hyponatremia Secondary to Pre-Eclampsia. Arch of Repr Med. 1(5): 2025. ARM.MS.ID.000522.
-
Hyponatremia, Preeclampsia, Maternal hyponatremia, Primary obstetric, Neonatology, Maternal fetal medicine, Hypertonic saline, Cesarean delivery, Crystalloid resuscitation, Prolonged induction
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.