Case Report
Case Report
Case Report – Endometrial TB
Selina Schmidtke, Johannes Nicolakis, Allessandra Aisha Tramontana and Beda Hartmann*
Danube Hospital, A 1220 Vienna, Austria
Beda Hartmann, Danube Hospital, A-1220 Vienna, Austria
Received Date:February 08, 2024; Published Date: March 11, 2024
Introduction
Tuberculosis remains one of the main causes of infectionrelated deaths worldwide, especially in developing countries. For the first time in two decades, the global incidence rate rose again between 2020 and 2022 by 3.9%, causing 1.3 million deaths in 2022 [1]. Miliary tuberculosis is a potentially fatal form caused by disseminated lymphohaematogenous spread of Mycobacterium tuberculosis bacilli. This form is more common in people with a compromised immune system, such as HIV-positive people. Pregnant and postpartum women also have an increased risk of developing miliary tuberculosis [2,3]. This risk is particularly high for women who have undergone in vitro fertilization (IVF) due to genital tuberculosis and infertility [4,5]. So far, there have only been a few reports of this disease following IVF treatment, with most cases coming from China, where tuberculosis is more common [6]. Here we present the case of a 30-year-old Kosovar woman who underwent a medically induced abortion after IVF. Subsequently, she developed miliary tuberculosis, which is rare in Austria.
Case
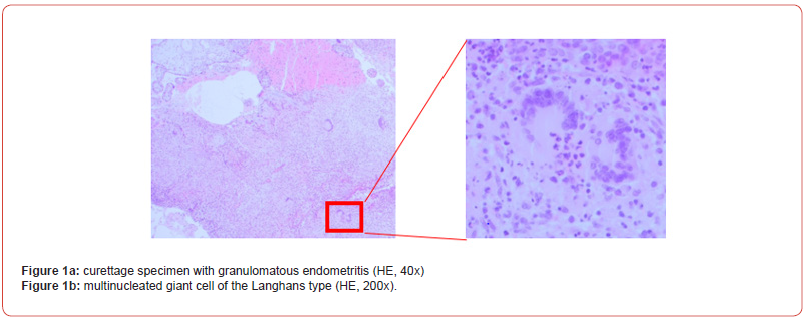
A 30-year-old woman presented to our clinic in October 2023 with vaginal bleeding at 18 weeks’ gestation in her second pregnancy after IVF procedure in which one embryo was transferred. The first pregnancy was a miscarriage in the sixth week of pregnancy. The patient had already undergone first trimester screening in the 13th week of gestation, which showed a pre-eclampsia risk of 1:39 before the 37th week. She was advised to take acetylsalicylic acid 150 mg until the 36th week of pregnancy. In the 18th week of gestation, the patient presented with light vaginal bleeding. Ultrasound was performed and showed an hydramnios and suspected polycystic kidney disease. A test to detect premature rupture of membranes was negative. Laboratory results showed high infection parameters, so the patient was treated with amoxicillin for a suspected infection. Due to the high risk of intrauterine and extrauterine death due to pulmonary hypoplasia, after careful consideration the patient and her partner decided to terminate the pregnancy. The patient underwent a medical abortion procedure using mifepristone and misoprostol, followed by a curettage. She was discharged the next day without any complications. Histologic examination of the curettage specimen showed exaggerated placental site and granulomatous endometritis with multinucleated giant cells of the Langhans type and extensive necrosis. Ziehl-Nelsen stain was negative for acid-fast bacilli; however, a mycobacterium-specific polymerase chain reaction was positive for Mycobacterium tuberculosis complex (IS6110-sequence). Histologic examination of the placenta revealed charangoists, subordinates and necrotizing amnionitis. Fetal autopsy and histology examination revealed a eutrophic male fetus with oligo-/an hydramnios sequence (contractures, lung hypoplasia) and neutrophile-rich stomach contents as sign of amnion infection syndrome. Granulomatous inflammation was not found in the placenta or the fetus. Ziehl- Neelsen stain and PCR for Mycobacterium was not performed on fetal or placental tissue. After consultation with the pathologist, the following progression was suspected: The urogenital tuberculosis caused endometrial necrosis, leading to premature rupture of the membranes with subsequent anhydramnios, leading to pulmonary hypoplasia and amnion infection syndrome.
Clinically, one month after the abortion, the patient had a daily fever, nocturnal cough without sputum and pain in her back. For further diagnosis, a CT scan of the chest and abdomen was performed and showed multiple disseminated nodular lesions <3 mm in both lungs as well as calcifications of the pleura and spleen, indicating miliary tuberculosis. The patient’s menstrual blood tested positive for tuberculosis by PCR. Mycobacterium tuberculosis was also detected in the urine and menstrual blood culture. Anti-TB medication with isoniazid, rifampicin, pyrazinamide and ethambutol was started for treatment. One week later, the patient presented again due to severe headaches and photophobia. A CT scan of the head showed no abnormalities. The patient was admitted to the emergency ward and a lumbar puncture was performed, which revealed a high cell count, high protein and glucose, suggesting tuberculosis meningitis. However, the liquor´s PCR test was negative. The anti-TB therapy was supplemented with adjuvant corticosteroid therapy. On the same day, the patient was admitted to a specialized tuberculosis centre for further treatment. An MRI of the brain revealed signs of tuberculosis meningitis. After one month of hospitalisation, the patient was discharged with anti- TB medication (Figures 1a & 1b).
Discussion
Active tuberculosis in pregnancy is highly related with increased maternal and fetal morbidity and mortality. Due to delayed diagnosis and treatment in pregnancy, tuberculosis is associated with miscarriages, induced abortions, premature births and increased maternal morbidity, including respiratory disease [7]. Reactivation of latent tuberculosis is probably one of the main causes of miliary tuberculosis in pregnancy. During pregnancy hormonal changes such as increased levels of estrogen, progesterone, and glucocorticoids modulate the immune system, which leads to a decrease in the activity of macrophages, NK cells, and T helper cells [8]. Studies have shown, that there is a higher incidence of military tuberculosis in pregnant women who have undergone in vitro fertilization and embryo transfer (IVF-ET) [9]. The use of glucocorticoids, progesterone and estrogen during IVF is associated with suppression of the immune system, thus leading to reactivation of TB and progression to disseminated infection [10,11]. This case report demonstrates the fulminant progression of miliary tuberculosis after an IVF-ET pregnancy and following medically induced termination due to endometrial tuberculosis and subsequent anhydramnios. Retrospective anamnesis revealed that the patient is originally from the Republic of Kosovo but has been living in Austria for the past three years. There is no known history of tuberculosis in her family or contacts. In retrospect, it is likely that chronic endometrial tuberculosis caused the first miscarriage in her medical history and subsequent infertility due to genital tuberculosis led to IVF treatment. Our case supports the recommendation that patients originating from countries with a high incidence of tuberculosis should be screened before undergoing IVF treatment due to infertility.
References
- (2023) World Health Organization. Global tuberculosis report Geneva.
- Sharma SK, Mohan A, Sharma A, Mitra DK. (2005) Miliary tuberculosis: new insights into an old disease. Lancet Infect Dis. Jul 1 5(7): 415-430.
- Sharma SK, Mohan A, Sharma A (2016) Miliary tuberculosis: A new look at an old foe. J Clin Tuberc Mycobact Dis May 1 18(3): 13-27.
- Hu Z, Zeng D, Yang Y, Liu H, Wang A, et al. (2023) Pathomorphological characteristics of tuberculous placenta and its clinical implication. Diagn Pathol 18(1): 128.
- Wang K, Ren D, Qiu Z, Li W (2022) Clinical analysis of pregnancy complicated with miliary tuberculosis. Ann Med 54(1): 71-79.
- Dong S, Zhou R, Peng E, He R (2022) Analysis of Clinical Features and Risk Factors in Pregnant Women with Miliary Pulmonary Tuberculosis After In Vitro Fertilization Embryo Transfer. Front Cell Infect Microbial 12: 885 -895.
- Sobhy S, Babiker Z, Zamora J, Khan K, Kunst H (2017) Maternal and perinatal mortality and morbidity associated with tuberculosis during pregnancy and the postpartum period: a systematic review and meta‐analysis. BJOG Int J Obstet Gynaecol 124(5): 727-733.
- Robinson DP, Klein SL (2012) Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Horm Behav 62(3): 263-271.
- Ye R, Wang C, Zhao L, Wu X, Gao Y, et al. (2019) Characteristics of miliary tuberculosis in pregnant women after in vitro fertilisation and embryo transfer. Int J Tuberc Lung Dis 23(2): 136-139.
- Liu S, Shi L, Wang T, Shi J (2018) Effect of low‐dose dexamethasone on patients with elevated early follicular phase progesterone level and pregnancy outcomes in IVF-ET treatment: A randomized controlled clinical trial. Clin Endocrinol (Oxf) 89(6): 771-778.
- Labarta E, Rodríguez C (2020) Progesterone use in assisted reproductive technology. Best Pract Res Clin Obstet Gynaecol 69: 74-84.
-
Selina Schmidtke, Johannes Nicolakis, Allessandra Aisha Tramontana and Beda Hartmann*. Case Report – Endometrial TB. Arch of Repr Med. Med. 1(4): 2024. ARM.MS.ID.000517.
-
Tuberculosis, In Vitro Fertilization (IVF), IVF Treatment, In Vitro Fertilization and Embryo Transfer (IVF-ET), Anti-TB Medication with Isoniazid, Rifampicin, Pyrazinamide, Ethambutol
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.