Research Article
Research Article
Time To Conversion of Hemi/Total Shoulder Arthroplasty To Reverse Total Shoulder Arthroplasty: A Systematic Review of Longevity and Factors Influencing Conversion
David S Constantinescu1*, Kevin J Lacy2, James R Satalich3, Alexander R Vap4
1Department of Orthopedic Surgery, University of Miami, USA
2,3,4Department of Orthopedic Surgery, VCU Medical Center, USA
David S Constantinescu, Department of Orthopedic Surgery, University of Miami, USA.
Received Date: January 22, 2021; Published Date: August 19, 2021
Abstract
Background: The purposes of this study were to determine the average time from hemiarthroplasty (HA) or total shoulder arthroplasty (TSA) to conversion to reverse total shoulder arthroplasty (RTSA) and to determine the factors leading to conversion to RTSA.
Methods: A review of the literature regarding the existing evidence for conversion of HA/TSA to RTSA was performed. Inclusion criteria were as follows: reporting of conversion of a HA or TSA to RTSA with a follow up of greater than 24 months, English language, and human studies. Excluded were articles that did not mention a time to conversion surgery.
Results: One hundred studies were initially retrieved with 3 meeting the inclusion criteria. The weighted mean time to conversion of HA/TSA to RTSA was 36.8 months. Rotator cuff failure was the indication for conversion in 66% of cases (65/99), while component loosening (glenoid or humeral stem) was the indication in 14% (14/99) of cases.
Conclusions: Among patients that undergo conversion of HA/TSA to RTSA the reported time to conversion was 36.8 months on average. The most common indication for conversion to RTSA was rotator cuff failure, highlighting the importance of rotator cuff integrity when performing a primary HA or TSA.
Keywords: Shoulder, arthroplasty, total shoulder arthroplasty, reverse shoulder arthroplasty, rotator cuff tear, revision shoulder arthroplasty, conversion shoulder arthroplasty.
Abbreviations:
1.Hemiarthroplasty (HA).
2.Total shoulder arthroplasty (TSA).
3.Reverse total shoulder arthroplasty (RTSA).
Introduction
The number of primary total shoulder arthroplasty (TSA) procedures performed is increasing [1-3]. The need for conversion to reverse total shoulder arthroplasty (RTSA) can also expected to follow given the number of primary TSAs performed among an increasingly active population. In instances of TSA or hemiarthroplasty (HA) where anatomic revision is not possible, a RTSA may be indicated to provide biomechanical stability to the shoulder [4-7]. No registrar data or aggregate literature analysis currently exists on the time from HA or TSA to conversion to RTSA.
There were two purposes of this study. The primary purpose of this study was to determine the average time from HA/TSA to conversion RTSA. The secondary purpose of this study was to determine the factors leading to conversion to RTSA. The outcomes of a revised TSA can be predicted on whether the indication for revision a component-related problem or soft tissue deficiency is [8] Therefore, surgeons must be aware of the most common reasons for HA/TSA revision and take this into account into their planning and prognostic discussions with patients. Our hypothesis was that the most common indication for conversion to RTSA was rotator cuff insufficiency.
Materials and Methods
Article Identification and Selection
This study was conducted in accordance with the 2009 Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement. A systematic review of the literature regarding the existing evidence for conversion to RTSA was performed using the Cochrane Database of Systematic Reviews, the Cochrane Central Register of Controlled Trials, PubMed (1980-present), and MEDLINE (1980-present). The queries were performed in August 2019.
The literature search strategy included the following search: “(((total shoulder arthroplasty) OR total shoulder replacement) AND conversion”. Inclusion criteria were as follows: reporting of conversion of a HA or TSA to RTSA with a follow up of greater than 24 months, English language, and human studies. The exclusion criteria included: non-English articles, case reports, technique papers, and articles that did not mention a time to conversion surgery. All references within included studies were crossreferenced for inclusion if missed by the initial search. If a duplicate study population was encountered, the manuscript with the longer mean follow-up was included to avoid overlap.
Two investigators independently reviewed the abstracts from all identified articles. Full-text articles were obtained for review if necessary to allow further assessment of inclusion and exclusion criteria. Additionally, all references from the included studies were reviewed and reconciled to verify that no relevant articles were missing from the systematic review.
Bias
Studies classified as level of evidence 3 or 4 can potentially be affected by selection and performance bias because of the lack of randomization and prospective comparative control groups (level 4), especially in populations characterized by heterogeneity of injuries. Selected studies were reviewed to ensure that authors minimized bias while recognizing the constraints present with such studies.
Data Collection
The level of evidence of the studies was assigned according to the classification as specified by Wright et al. [9] The information was collected from the included studies. Patient demographics, follow-up, outcome scoring methods, primary surgery, time to conversion surgery and implant system used were extracted and recorded. For continuous variables (eg, age, timing, follow-up, outcome scores), the mean and range were collected if reported. Data were recorded into a custom Microsoft Excel spreadsheet (Microsoft Corp) using a modified information extraction table.
Results
Study Selection
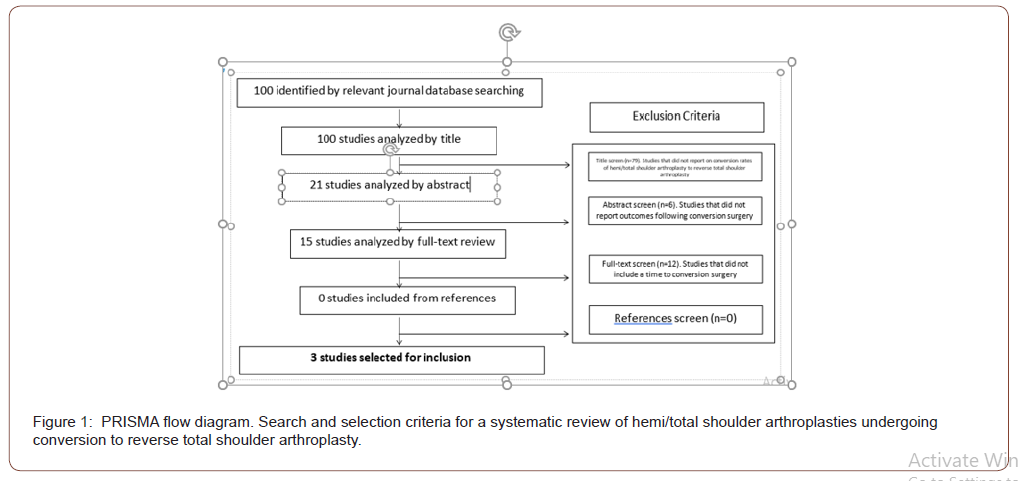
The systematic search performed using the above-mentioned keywords and phrases identified three studies, after removing duplicates and applying exclusion criteria [10-12]. One hundred articles were initially identified from the MEDLINE database. There were no additional articles from the Cochrane database. Each article was first screened by title leaving 21 articles. Excluded articles based on title screen were those that did not report on conversion surgeries from HA/TSA. The remaining articles were then screened by abstract yielding 15 articles. Excluded articles based on abstract screen were those that did not report outcomes following conversion surgery. After full text review, three studies met criteria and were included in the review. Studies that were excluded after full text screen were those that did not report a time to conversion surgery from primary surgery. Two studies that were included were of Level III evidence and one study was of Level IV evidence. Figure 1 is a PRISMA flowchart that demonstrates selection criteria of the systematic review. Following review of all references from the included studies, no additional studies met inclusion criteria.
Demographics
In this review a total of 99 patients were included. Study sizes ranging from 17 patients to 56 patients. The review included 99 patients (31 male, 68 female) with a mean age 69 (range: 67 – 73). The average follow up was 35.8 months (range: 32.3 – 37.4). Demographics of each included study are reported in Table 1.
Table 1:Study design, patient demographics and outcome scores of included conversion RTSA studies. VAS = Visual analog scale.
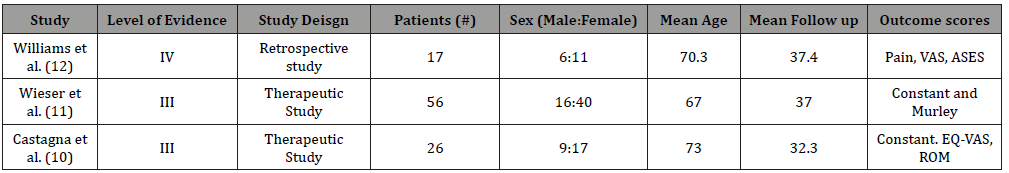
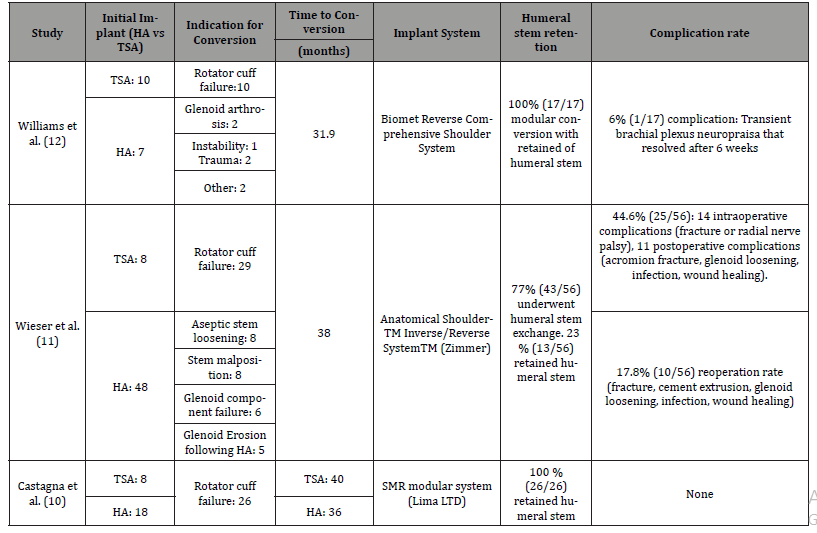
Table 2:Primary surgery implant, indication for conversion, time to conversion, implant system, retention of primary humeral stem and complication rates for included conversion RTSA studies. HA = hemiarthroplasty. TSA = total shoulder arthroplasty.
Time to conversion RTSA
The weighted mean time to conversion of HA/TSA to RTSA was 36.8 months (31.9 – 40). Individual times reported by each study are detailed in Table 2. All three studies contained patients whose primary surgery was a HA or TSA. Castagne et al. was the only of the three who compared the time to surgery between HA and TSA [10].
Indications for Conversion
Rotator cuff failure occurred in 66% of cases (65/99), while component loosening occurred in 14% (14/99) of cases. Among the component loosening, glenoid occurred in 6% (6/99) of cases and humeral stem occurred in 8% (8/99) of cases. Castagne et al. reported that 100% (26/26) patients who underwent conversion did so due to rotator cuff insufficiency [10]. None of the studies reported evaluation of rotator cuff integrity prior to primary TSA.
Primary surgery hardware retention and complication rates
Retaining the humeral stem when performing RTSA conversion surgery occurred in 57% (56/99) of patients. Humeral stem exchange was performed in 43% (43/99) of patients. All three studies reported on complications. Overall, there was a 26.2% (26/99) complication rate among conversion RTSA’s. Reoperation rate was 10% (10/99) and all reoperations occurred within Wieser et al. [11].
Discussion
This review found that the reported time to conversion of HA/ TSA to RTSA was 36.8 months on average with the most common indication for conversion being rotator cuff insufficiency. This highlights the importance of rotator cuff integrity when performing a primary HA or TSA.
TSA has historically been indicated in patients with pain due to isolated glenohumeral arthritis while RTSA has been indicated in cases of rotator cuff arthropathy [13]. Survivorship studies have demonstrated that 85% of primary TSA’s will survive 20 years, with the most common need for revision being component loosening. [14] However, restoring range of motion and activity in previously arthritic shoulder may predispose the rotator cuff to damage. The resultant loss of function in the shoulder may be addressed through conversion of a TSA to RTSA, which recovers shoulder function through restoring the deltoid muscle and altering the functional fulcrum in a rotator cuff deficient shoulder [15]. In fact, a recent study has suggested that RTSA’s may have a role over TSAs in select populations with glenohumeral arthritis even in the presence of an intact rotator cuff [16]. Our study corroborates this idea given the high incidence of rotator cuff insufficiency that necessitated conversion to RTSA.
Due to anticipated rotator cuff insufficiency that may follow TSA, modular components of the humeral stem and glenoid have been designed to facilitate conversion to RTSA [17-20]. Retaining the humeral stem when performing conversion RTSA has been demonstrated to result in lower complication rates [21-24] Of the three studies included in our review, Wieser et al was the only one to include a cohort of patients undergoing humeral stem exchange and also found that stem exchange was associated with a higher complication rate than stem retention [11].
Complication rates for RTSA have been reported to be approximately 15% in the primary surgery and become higher (40%) when RTSA in the revision setting [25]. The complication rate in our studies was 26.2% (26/99) rate among conversion RTSA’s, with the majority of complications being from a cohort of patients that included humeral stem exchange. This finding emphasizes the importance of proper component alignment in the primary surgery to minimize complications if a revision surgery is required.
An important limitation of this study was the level of evidence of the included studies. All were Level III or IV of retrospective cohorts of patients. Subsequently, it is difficult to give definitive quantification of arthroplasty longevity and predisposing factors to revision surgery. Being that not all primary HA’s TSA’s were included and followed for an extended period, this was not a survivorship study suited to answer how long HA/TSA last. Rather, we were able to provide insight as to when primary HA/TSA’s are typically converted to RTSA and the underlying etiology necessitating revision. Based upon available literature, this manuscript is able to provide reasonable analysis to aid the physician in prognostic factors in conversion RTSA.
Conclusions
Among patients that undergo conversion of HA/TSA to RTSA the reported time to conversion was 36.8 months on average. The most common indication for conversion to RTSA was rotator cuff failure, highlighting the importance of rotator cuff integrity when performing a primary HA or TSA.
Conflict of Interest
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
The authors, their immediate family, and any research foundation with which they are affiliated did not receive any grant sport or research funding.
Acknowledgement
None.
References
- Day JS, Lau E, Ong KL (2010) Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg 19(8): 1115-120.
- Khatib O, Onyekwelu I, Yu S (2015) Shoulder arthroplasty in New York State, 1991 to 2010: changing patterns of utilization. J Shoulder Elbow Surg 24(10): e286-291.
- Kim SH, Wise BL, Zhang Y (2011) Increasing incidence of shoulder arthroplasty in the United States. J Bone Joint Surg Am 93(24): 2249-2254.
- Boileau P, Watkinson D, Hatzidakis AM, Neer Award (2006) The Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg 15(5): 527-540.
- Guery J, Favard L, Sirveaux F (2006) Reverse total shoulder arthroplasty. Survivorship analysis of eighty replacements followed for five to ten years. J Bone Joint Surg Am 88(8): 1742-1747.
- Samitier G, Alentorn-Geli E, Torrens C (2015) Reverse shoulder arthroplasty. Part 1: Systematic review of clinical and functional outcomes. Int J Shoulder Surg 9(1): 24-31.
- Stechel A, Fuhrmann U, Irlenbusch L (2010) Reversed shoulder arthroplasty in cuff tear arthritis, fracture sequelae, and revision arthroplasty Acta Orthop 81(3): 367-372.
- Dines JS, Fealy S, Strauss EJ (2006) Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am 88(7): 1494-500.
- Wright JG, Swiontkowski MF, Heckman JD (2003) Introducing levels of evidence to the journal. J Bone Joint Surg Am 85(1): 1-3.
- Castagna A, Delcogliano M, de Caro F (2013) Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop 37(7): 1297-1305.
- Wieser K, Borbas P, Ek ET (2015) Conversion of stemmed hemi- or total to reverse total shoulder arthroplasty: advantages of a modular stem design. Clin Orthop Relat Res 473(2): 651-660.
- Williams PN, Trehan SK, Tsouris N (2017) Functional Outcomes of Modular Conversion of Hemiarthroplasty or Total to Reverse Total Shoulder Arthroplasty. HSS J 13(2): 102-107.
- Neer CS, Craig EV, Fukuda H (1983) Cuff-tear arthropathy. J Bone Joint Surg Am 65(9): 1232-1244.
- Deshmukh AV, Koris M, Zurakowski D (2005) Total shoulder arthroplasty: long-term survivorship, functional outcome, and quality of life. J Shoulder Elbow Surg 14(5): 471-479.
- Drake GN, O’Connor DP, Edwards TB (2010) Indications for reverse total shoulder arthroplasty in rotator cuff disease. Clin Orthop Relat Res 468(6): 1526-1533.
- Wright MA, Keener JD, Chamberlain AM (2020) Comparison of Clinical Outcomes After Anatomic Total Shoulder Arthroplasty and Reverse Shoulder Arthroplasty in Patients 70 Years and Older With Glenohumeral Osteoarthritis and an Intact Rotator Cuff. J Am Acad Orthop Surg 28(5): e222-e229.
- Chuinard C (2015) CORR Insights®: conversion of stemmed hemi- or total to reverse total shoulder arthroplasty: advantages of a modular stem design. Clin Orthop Relat Res 473(2): 661-662.
- Kirsch JM, Khan M, Thornley P, et al. Platform shoulder arthroplasty: a systematic review. J Shoulder Elbow Surg 27(4): 756-763.
- Teschner H, Albrecht UV, Meller R (2014) Conversion of hemi into reverse shoulder arthroplasty: implant design limitations. Arch Orthop Trauma Surg 134(12): 1683-1689.
- Valenti P, Katz D, Kany J (2018) Convertible Glenoid Components Facilitate Revisions to Reverse Shoulder Arthroplasty Easier: Retrospective Review of 13 Cases. Am J Orthop 47(2).
- Crosby LA, Wright TW, Yu S (2017) Conversion to Reverse Total Shoulder Arthroplasty with and without Humeral Stem Retention: The Role of a Convertible-Platform Stem. J Bone Joint Surg Am 99(9): 736-742.
- Dilisio MF, Miller LR, Siegel EJ (2015) Conversion to Reverse Shoulder Arthroplasty: Humeral Stem Retention Versus Revision. Orthopedics 38(9): e773-779.
- Weber-Spickschen TS, Alfke D, Agneskirchner JD (2015) The use of a modular system to convert an anatomical total shoulder arthroplasty to a reverse shoulder arthroplasty: Clinical and radiological results. Bone Joint J 97-B (12): 1662-1667.
- Werner BS, Boehm D, Gohlke F (2013) Revision to reverse shoulder arthroplasty with retention of the humeral component. Acta Orthop 84(5): 473-478.
- Barco R, Savvidou OD, Sperling JW (2016) Complications in reverse shoulder arthroplasty. EFORT Open Reviews 1(3): 72-80.
-
David S Constantinescu, Kevin J Lacy, James R Satalich, Alexander R Vap. Time To Conversion of Hemi/Total Shoulder Arthroplasty To Reverse Total Shoulder Arthroplasty: A Systematic Review of Longevity and Factors Influencing Conversion. Arch Rheum & Arthritis Res. 1(4): 2021. ARAR.MS.ID.000517.
-
Arthroplasty, Arthritis, Hemiarthroplasty, surgery, Shoulder
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.