 Opinion Article
Opinion Article
Physical Analgesia and Functional Recovery in Hip and Knee Osteoarthritis: Rehabilitation Algorithms
Ivet B. Koleva1,2*, Borislav R Yoshinov3, Radoslav R. Yoshinov4 and Teodora A Asenova3
1Department of Physiotherapy, Medical University of Sofia, Bulgaria
2Department of Physical and Rehabilitation Medicine, Specialized Hospital for long-term care and rehabilitation “Serdika” with Medical Center “ReGo”– Sofia, Bulgaria
3Medical Faculty of Sofia University, Bulgaria
4University of Library studies and Information Technologies UNIBIT – Sofia, Bulgaria
Ivet Koleva, Department of Physiotherapy, Medical University of Sofia and Department of Physical and Rehabilitation Medicine, Specialized Hospital for long-term care and rehabilitation “Serdika” with Medical Center “ReGo”– Sofia, Bulgaria.
Received Date: September 30, 2022; Published Date: October 07, 2022
Abstract
Osteoarthritis (OA) is a socially important disease, with a high level of alteration of the quality of life of many persons. Pain is a frequent symptom of several conditions, treated with numerous drugs. The goal of current article is to remain the potential of physical factors for treatment of pain (physical analgesia) and for functional recovery. Our purpose was to emphasize the potential of some contemporary physical modalities and to propose complex rehabilitation algorithms for pain management and for functional recovery of OA-patients.
Principal clinical and instrumental treatment methods are stated: electrotherapy (with low and middle frequency electric currents); magnetic field; ultrasound; laser; hydrotherapy and balneotherapy (mineral waters); physiotherapy (analytic exercises, mirror therapy, soft-tissue techniques, massage), balneophysiotherapy (underwater exercises, swimming); manual therapy, device-assisted mechano-therapy (passive, active or combined), robotic rehabilitation, etc.
In rehabilitation practice, for diagnostic: we apply functional scales, International Classification of Diseases and International Classification of Functioning. For treatment: we combine synergically different natural and preformed physical modalities. We insist on the importance of technical aids (canes, walking sticks, etc.).
Authors recommend structured rehabilitation algorithms for OA-patients, including elements of preformed physical modalities, physiotherapy, ergotherapy, and patient’s education. We present details of the application of these algorithms on typical forms of hip and knee OA, including after hip and knee arthroplasty.
Keywords: Osteoarthritis; Pain; Physical analgesia; Algorithm; Functional assessment; Functional recovery; Physical medicine; Rehabilitation
Abbreviations: ADL: Activities of Daily Life; ET: Ergotherapy; FES: Functional electrical stimulations; IASP: International Association for the Study of Pain; ICD: International Classification of Diseases; ICF: International Classification of Functioning, Disability and Health; IFC: Interferential currents; MF: Magnetic field; MTh: Manual therapy; OA: Osteoarthritis, osteoarthrosis; OT: Occupational therapy; PIR: Post-isometric relaxation; PRM: Physical and Rehabilitation medicine; PT: Physiotherapy; QF: Quadriceps femoris muscle; RoM: Range of motion; UEMS: Union Europeenne des Medecins Specialistes (European Union of Medical Specialists); US: Ultrasound; VAS: Visual Analogue Scale; WB: Weight Bearing; WHO: World Health Organization; WOMAC: Western Ontario and McMaster Universities Arthritis Index
Introduction
Osteoarthritis and osteoarthrosis
Osteoarthritis (OA) is a socially important degenerative joint disease, with a high level of alteration of the quality of life of many patients [1]. The term osteoarthritis derives from the ancient Greek words “osteon” (bone), “arthron” (joint) and “itis” (pertaining to). Later the suffix – “itis” is associated with inflammation and some rheumatologic schools denominate the disease osteoarthrosis, using the suffix “-osis” (from pathosis - state, condition), emphasizing the lack of inflammation [2]. In our country OA is a frequent disorder, involving commonly weight bearing joints of lower extremity - hip (hip OA or cox-arthrosis) and knee (knee OA or gon-arthrosis). Principal symptoms include joint pain, stiffness and tenderness; reduction of the range of motion; joint deformities; gait problems; difficulties in everyday activities and disability. Pain is recurrent OA-symptom, provoking necessity of consultation and aggravating the quality of life.
Pain, physical analgesia, physical modalities for functional recovery
Pain is one of the most frequent sensations, formed in the nervous system. According to the definition of the International Association for the Study of Pain (IASP): pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage [3]. The Declaration of Montréal of the International Pain Summit of IASP identifies chronic pain as a serious chronic health problem [3]. Access to pain management is considered as a fundamental human right [4]. We proposed the concept of physical analgesia intended for the application of physical factors for pain treatment [5]. By our opinion the anti-pain effect of physical modalities is significant, with a high level of efficacy. Physical analgesia has not side consequences and may be applied in combination with other therapeutic factors.
For physical analgesia and for functional recovery, many physical modalities can be applied:
• Preformed modalities: Electric currents; Magnetic field; Laser; Deep Oscillation; Ultra-sound.
• Natural modalities: Cryo- and Thermo-agents; Hydro- and balneo-techniques; Physiotherapy (PT); Hydro and Balneophysiotherapy; Peloidotherapy.
• Reflectory methods: application of physical modalities in reflectory points and zones (e.g., biologically active points, acupuncture points).
Physical and Rehabilitation medicine (PRM)
According to the definition of the European Union of Medical Specialists – PRM Section [6]: Physical and Rehabilitation Medicine (PRM) is an „independent medical specialty, oriented to the promotion of physical and cognitive functioning, activities (including environment), participation (including quality of life) and changes in personal factors and environment”. In clinical rehabilitation practice, the role of medical doctor – physiatrist (specialist in PRM) is substantial [7].
Objective
The goal of current article is to remain the potential of some physical factors for pain management (physical analgesia) and functional recovery of OA patients. Our purpose was to emphasize the potential of some contemporary physical modalities and to propose complex OA rehabilitation algorithms, based on practice and research.
Common Rehabilitation Algorithm in OA
In rehabilitation clinical practice, our diagnosis is founded on the International Classification of Diseases (ICD) [8] and on the International Classification of Functioning, Disability and Health (ICF) [9]. According ICF principles, the complex functional assessment must include body functions, activities and participation. For OA patients, we accentuate on some important elements: pain measurement (using the Visual Analogue scale 0-10); evaluation of the range of motion (RoM = goniometry), joint stability and joint position sense; assessment of patients’ autonomy in activities of daily life (ADL). Basic rehabilitation algorithm for OApatients must include elements of preformed physical modalities, physiotherapy, ergotherapy, and patient’s education [10, 11].
In OA-rehabilitation practice we apply [12, 13, 14]:
• Preformed physical modalities: low-frequency electric currents (iontophoresis, transcutaneous electro neurostimulation – TENS); middle-frequency electric currents (interferential currents /IFC/, Kots-currents); electrostatic field (Deep oscillation /DO/); low frequency low intensity magnetic field /MF/; laser-therapy and laser-puncture.
• Physiotherapy (PT): analytic exercises, aerobic exercises, range-of-motion (ROM) exercises, strengthening exercises, soft-tissue techniques, massage).
• Hydrotherapy and balneotherapy (with mineral waters, containing sulfur); Peloidotherapy: mud applications, sealye compresses; Balneophysiotherapy: underwater exercises; underwater massages, swimming.
• Manual therapy (MTh: tractions, mobilizations and manipulations).
• Device-assisted mechano-therapy (passive, active or combined), robotic rehabilitation (Lokomat).
• Occupational therapy (OTh): Education of the person with disability by means of task oriented (task-specific) activities; application of technical aids (canes, walking sticks, crutches, rollators); home adaptations.
Rehabilitation of OA patients requires a coordination of medical doctors - specialists in Rheumatology and in Physical and Rehabilitation medicine (PRM). OA-rehabilitation is in the field of competence of PRM-doctors [6,7]. In the multi-professional multidisciplinary rehabilitation team, we include nurses, physiotherapists and occupational therapists (according to the nomenclature of our country – kinesiotherapists and ergotherapists).
The control before and after rehabilitation is obligatory. At the end of every course, we realize a detailed clinical, para-clinical and functional (including instrumental) evaluation and (if necessary) reconsideration of the obtained results, control and periodic PRM courses. Functional evaluation is very important for control of the quality of rehabilitation, for stimulation of patients’ autonomy in everyday activities and for amelioration of health-related quality of life of patients. We adapt this basic algorithm on different forms of OA - hip and knee OA (including after hip and knee replacement).
Rehabilitation Algorithms in Different Types of OA
Usually, our patients are transferred to PRM department from Rheumatology Department (Clinic) of the University hospital, with proved diagnosis OA and with difficulties in everyday activities.
Hip OA (Coxarthrosis)
The hip is a joint of the type “ball and socket” with a concave acetabulum and a convex femoral head. Possible movements are flexion and extension in the sagittal plane, abduction and adduction in the frontal plane, external and internal rotation in the transversal plane and circumduction in all planes. The osteoarthritic patient suffers from pain, stiffness, difficult locomotion and reduced autonomy in activities of daily life (ADL).
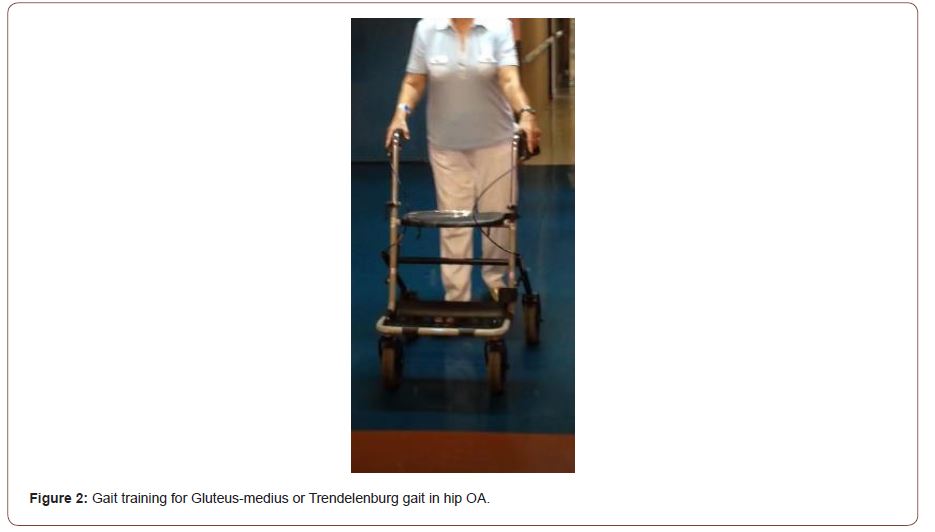
During clinical exam and functional assessment, we observe limited range of motion (ROM), especially abduction and rotations, in advanced stages - extension, flexion; pain and crepitation during movement; Trendelenburg sign; positive Patrick test (flexionabduction- external rotation /FABER/ test); abductor weakness and gait type “gluteus medius” or Trendelenburg. Evaluation according to Kellgren-Lawrence scale and ICF are obligatory. In some cases, we use Timed Up and Go test, 6 minutes’ walk test and others.
Objectives of rehabilitation in hip OA comprise pain reduction, restoration of ROM and muscle weakness, functional recovery of the hip arthro-kinematics and recapture of the “normal” gait.
Management of hip OA include joint supplements, antiinflammatory drugs, lifestyle modifications, weight control (eventually reduction), gait assistance with technical aids (cane, walker), sport (swimming).
Suitable rehabilitation methods for hip OA are:
• Physical therapy (progressive exercise program for ROM and strength, analytic exercises for hip abductors /gluteus medius muscle/, stationary bicycle, Rocher mobilizations, stretching).
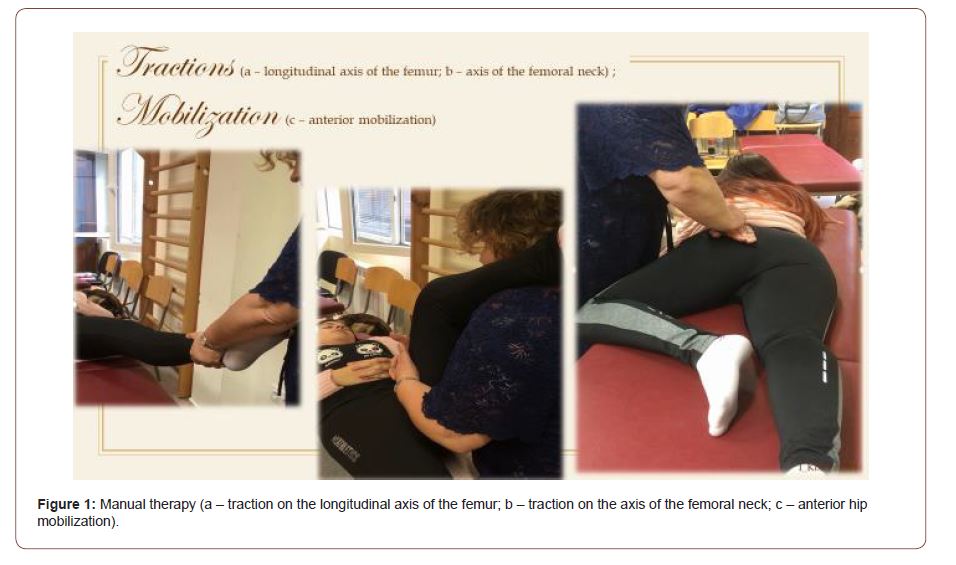
• Manual therapy (tractions and mobilizations – figure 1).
• Ergotherapy (occupational therapy - activities modification; static and dynamic balance exercises – on one leg, tandem stance, balance on instable surface; gait training with technical aids for “normalization” of the gait pattern – figure 2; ADL training).
• Preformed physical modalities (interferential currents /IFC/, magnetic field /MF/, transcutaneous electroneurostimulation /TENS/, LASER, Deep Oscillation).
• Thermo-therapy (paraffin, peloids /e.g., therapeutic mud/).
• Hydro-balneo-therapy and Hydro-physiotherapy (mineral baths in sulfured waters, underwater massage, underwater exercises).
The complex rehabilitation algorithm must include two or three preformed modalities, one thermo-agent of hydro-procedure, two or three physiotherapeutic and ergo therapeutic procedures.
In patients with advanced hip OA, a surgical procedure for hip replacement (endoprosthesis) is indicated. After the hip arthroplasty, the patients suffer from excessive pain and stiffness in the hip and muscles around it; difficulties in transfers and mobility; reduction of independence in ADL. Obligatory elements of the clinical exam are assessment of the possible (limited) range of motion of the correspondent lower extremity (hip goniometry), and inspection on the operative cicatrix (for eventual complications). The ICF assessment objectivizes impairments of body functions (hip pain, muscle weakness, and restricted hip ROM); changes in body structures; activity limitation (limited walking ability and problems with putting on socks); participation restrictions (reduced participation in work and leisure activities); decrease of patient’s level of autonomy. We estimate the rehabilitation potential (basic condition and comorbidities).
Our rehabilitation tasks include: recovery of the stability and mobility of the lower limb joints; restoration of the muscle and ligament balance, accentuating on muscles around the hip joint; keeping the hip in the economic limb biomechanics; pain control; control of the cicatrix; control of joint ROM; control of possible complications; education of transfers; gradual gait recovery with correction of eventual abnormal walking scheme; ADL training; amelioration of autonomy in everyday life; psychoemotional stimulation; amelioration of the health-related quality of life. Essentials of the rehabilitation program include: drugs (Fraxiparine; analgesics); patient’s education in correct posture & walking scheme (activity modification); electrotherapy (IFC, DO), magnetic field (MF); cryotherapy - for the hip joint (before the massage and the kinesitherapy); massage – classic massage (relaxing for the anterior group of muscles of the hip; stimulating for gluteal muscles); Individualized kinesitherapeutic and ergo therapeutic program; Occupational therapy & ADL training.
Immediately after the hip replacement we survey the operated leg position (hip adduction and rotations are forbidden, the hyperflexion over 90 degrees is not permitted). Initially, in bed, we begin with respiratory exercises; analytic exercises for the distal parts of the operated lower extremity and for the healthy limbs; movements for stimulation of the circulation and for prevention of thrombosis, oedema, muscle hypotrophy or joint contractures. After, we apply continuous passive motion for the operated leg, using a mechanotherapy device. Training goals include improvement of motor skills (ROM and muscle strength), restoration of correct gait pattern and prevention of complications (contractures, thrombosis, etc.). We insist on some elements: correct posture of lower limb; analytic exercises for gluteal muscles (especially for gluteus medius muscle); lower limb joint mobilization (active range of motion); post-isometric relaxation /PIR/ for iliopsoas muscle; gait training with supporting walker or two crutches; education in mobility up and down the stairs. The gait initially must be with walker or crutches, if possible, with an assistant. We insist on gait training with progressive weight bearing (WB): from non-weight bearing during the first 2-4-6 weeks, after that: 25% - 50 % - 75 % up to full weight bearing and gait recovery at the 6th month (at the beginning – with crutches, after that – with cane, finally - without technical aids). For some patients, stationary bicycle or underwater exercises and swimming are recommended.
Periodically, we evaluate the efficacy of rehabilitation, applying different tests, as: 10 meters walk test (10mWT - in seconds before & after rehabilitation); Timed Up and Go test (TUG in seconds - before rehab); 6 Minutes’ Walk Test (6 MWT in meters - after rehabilitation). At the discharge, we recommend a long-life hip conditioning program, including stretching and strengthening exercises for restoration of muscle balance around the hip joint – especially oriented to gluteus maximus, gluteus medius, ilio-psoas and hamstrings muscles. NB! Exercises must be done without pain (or increase of current pain). We permit to the patient this auto-PTtraining at home, only if the therapist guarantee the correct practice of exercises.
Knee OA
The knee kinematic complex includes tibio-femoral and patellofemoral joints, with a common joint capsule. Normal movements are flexion and extension, and internal and external rotation (rotations only from sitting position, with knee flexion at 90 degrees). The stabilization of the knee in ventro-dorsal direction is secured by cruciate ligaments (anterior and posterior) and in medio-lateral direction – by collateral ligaments (medial and lateral). Knee OA (or gonarthrosis) is the most frequent localization of OA, with serious impact on locomotion and with functional limitations, especially in the elderly.
During functional assessment we insist on: VAS; ROM; manual muscle test; presence of hypotrophy of vastus medialis muscle (especially vastus medialis obliquus); joint deformities (genu varum or genu valgum); evaluation of pain, stiffness and of physical function according to the Western Ontario and McMaster Universities Arthritis Index (WOMAC), ICF evaluation. We consider as imperative the capacity to walk and climbing stairs, and the necessity of technical aids.
Principal goals of the rehabilitation algorithm in knee OA comprise pain control; restoration of muscle balance around the knee joint; recovery of knee stability and mobility; correction of the abnormal walking schema and recovery of the normal gait, with respect to the economy of lower limb biomechanics; optimizing the knee function.
For this, we apply many therapeutic methods:
• Patient education, diet (for weight reduction), activity modification; knee orthoses.
• Rehabilitation using different physical modalities.
• Pharmacological methods: analgesics, anti-inflammatory drugs; chondroprotectors.
• Surgery (joint replacement procedure – in advanced cases).
From the group of physical modalities, we use:• Thermo- or Cryotherapy (ice or paraffin applications, cold packs or hot packs).
• PT with ROM-exercises; Analytic exercises for quadriceps femoris muscle (QF) – especially for m. vastus medialis (obliquus).
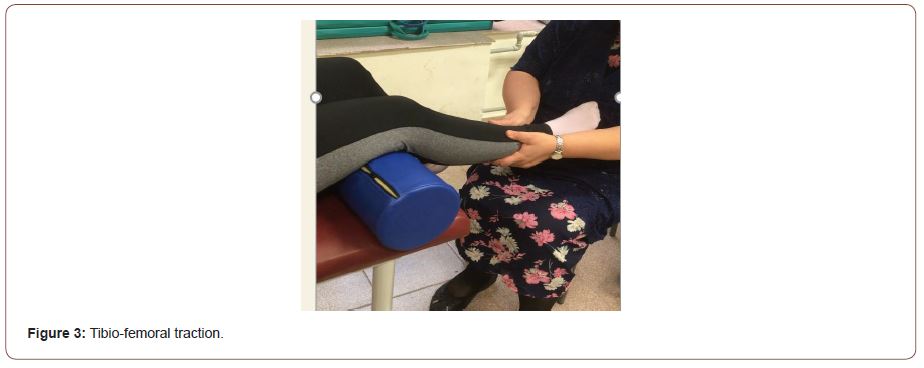
• Manual Therapy: Tractions (distractions) and Mobilizations.
• Gait training with cane and knee orthosis.
• Soft-tissue techniques: post-isometric relaxation (PIR) for rectus femoris muscle; massage (classic or special massages, e.g., Cyriax Massage).
• Underwater exercises and underwater jet massage; in a pool or bath with sulfured mineral waters.
• Peloidotherapy (therapeutic mud, sea lye compresses, fango).
• Preformed physical modalities: MF, IFC, TENS, Deep Oscillation, Laser. In some cases, functional electrical stimulations (FES) of vastus medialis muscle are needed.
We insist on the necessity of knee OA prevention using manual therapy, especially tibio-femoral traction (figure 3) and patellar mobilizations (figure 4).

Knee arthroplasty for OA is generally a planned operation in advanced stages. In the pre-operative period, we apply preparation of several muscles with analytic exercises: deep low abdominal and pelvic muscles, buttock muscles, flexors and extensors of the knee joint. Early after total knee replacement, we apply continuous passive motion machine for gradual augmentation of the ROM of the operated knee. Immediately post-op we apply breathing exercises; stimulation of the circulation in lower limbs trough ankle circles and ankle pumps (contraction and relaxation of triceps surae muscle) – from lying and sitting position; swelling control by position therapy of the operated knee (elevation with pillows); knee squeezes. We start with ROM exercises for the knee joint (up to 90 degrees of flexion), and after – we include strengthening exercises for knee flexors and extensors muscles. We include knee stretch and bending exercises for the operated knee. Gradually we begin with standing exercises and gait training with control of the weight bearing (from partial to total WB): standing from sitting position with the operated leg ahead of the healthy lower extremity, walking with a walker and gait training upstairs and down-stairs. Finally, we include lateral step-up movements. After the 6th week post-op, the patient generally adheres to home exercise program. Return to functional activities is possible after restauration of the appropriate balance, proprioception and correct gait pattern. At the discharge, we prescribe a long-life knee conditioning program, including stretching and strengthening exercises for restoration of muscle balance around the knee joint – accentuating on quadriceps femoris and hamstrings muscles. At the beginning, exercises must be done under control of the respective therapist.
Discussion
Efficacy of rehabilitation algorithms in clinical practice
Common results of the complex rehabilitation program include Increase of the range of motion of the lower limbs; Amelioration of the functional capacity; Pain reduction; Independent stand up and transfers; Independent gait (with or without technical aids) in the room and the corridor; Balance & Gait stabilization; Decrease of dysesthesias in distal parts of lower limbs; Stabilization of cardiovascular and metabolic patterns; Amelioration of autonomy in ADL.
Our opinion is that the role of different elements of the complex rehabilitation programs must be considered for stimulation of functional recovery, pain reduction and improvement of everyday quality of life of OA patients. The rehabilitation algorithms must be adapted individually in every case.
Conclusion
In our clinical practice we apply systematically our structured rehabilitation algorithms, individualized and adapted to the concrete patient. We published periodically our results [11, 12, 13, 14], proving the amelioration of the quality of life of different types of OA patients. In case of synergic combination of procedures, we received statistically significant favorable effects on pain, range of motion, muscle force, grasp and gait, independence in ADL, quality of life of patients.
Authors consider that rehabilitation must be included in OA-therapeutic guidelines. Complex rehabilitation stimulates functional recovery of patients with invalidating diseases and conditions of the motor system, ameliorating their health-related quality of life.
Acknowledgement
We express gratitude to our staff of all PRM-Departments and Clinics – base of our work. The coordinated teamwork is the crucial circumstance for a successful rehabilitation process.
Ethical approval
Requirements of the Declaration of Helsinki for patients’ rights are accomplished. ‘Written informed consent’ was obtained from every patient before any examination, procedure and photo.
Conflict of Interests
Authors declare the non-existence of any financial interest or any conflict of interests.
References
- Cross M, Smith E, Hoy D (2014) The global burden of hip and knee osteoarthritis: estimates from the Global Burden of Disease 2010 study. Annals of Rheumatic diseases 73(7): 1323-1330.
- Mohammed A, Alshamarri T, Adeyeye T, Lazariu V, McNutt LA, et al. (2020) A comparison of risk factors for osteo- and rheumatoid arthritis using NHANES data. Prev Med Rep 5(20): 101242.
- www.iasp-pain.org
- UNESCO (2005) Universal Declaration on bioethics and human rights.
- Koleva I, Yoshinov R, Yoshinov B (2018) Physical analgesia. Monograph. – Saint-Denis, France: “Connaissances et saviors”, Science Santé, 146 pages.
- European Physical and Rehabilitation Medicine Bodies Alliance (2018) White Book on Physical and Rehabilitation Medicine (PRM) in Europe. Chapter 7. The clinical field of competence: PRM in practice. Eur J Phys Rehabil Med 54(2): 230-260.
- White Book on Physical and Rehabilitation Medicine in Europe. Third Edition (2018). European PRM Bodies Alliance: European Academy of Rehabilitation Medicine, European Society of PRM, EUMS – PRM Section, European College of PRM. European Journal of Physical and Rehabilitation Medicine 54(2): 1-204.
- World Health Organization (2018) International Classification of Diseases (ICD – revision XI) – WHO, Geneva.
- World Health Organization (2001) International Classification of Functioning, Disability and Health (ICF). – WHO, Geneva.
- Коleva I (2006) Repetitorium physio-therapeuticum (basic principles of the modern physical and rehabilitation medicine). Book for English Speaking Students of Pleven Medical University. Sofia: SIMEL.
- Koleva I, Yoshinov B (2016) Rehabilitation algorithms in Osteoarthrosis. - In: Abstracts of the V-th national conference (with international participation) of the Bulgarian Medical Society on Osteoporosis and Osteoarthritis, Bansko, Bulgaria: 33-34.
- Koleva I (2014) Physical analgesia and Deep Oscillation. A monograph. – Sofia: SIMEL. [in Bulgarian]
- Koleva I, Yoshinov R, Marinov M, Hadjijanev A (2015) Efficacy of hydro-, balneo- and peloidotherapy in the pain management and quality of life of patients with socially important diseases and conditions of the locomotory and nervous system: Bulgarian experience. Balnea, 10, Serie de Monografías Pg No: 273-274.
- Koleva I, B R Yoshinov (2016) Physical analgesia in osteoarthritis – methods and mechanisms. - In: Abstracts of the V-th national conference (with international participation) of the Bulgarian Medical Society on Osteoporosis and Osteoarhtrosis. Bansko Pg No: 25-26.
-
Ivet B. Koleva*, Borislav R Yoshinov, Radoslav R. Physical Analgesia and Functional Recovery in Hip and Knee Osteoarthritis: Rehabilitation Algorithms. Arch Rheum & Arthritis Res. 2(3): 2022. ARAR.MS.ID.000538.
-
Joint, Inflammation, physiotherapy, Peloidotherapy, Coxarthrosis, Knee OA, Surgery.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






