Case Report
Case Report
Clinical Presentation, Treatment, and Outcome
of Spontaneous Chronic Asymptomatic Bilateral
Dislocation After Total Hip Arthroplasty: Unusual
Case Report
Vianney Hope JM*, Paul Bitega J, Francis Mugabo, Edmond Mukimbili and Albert Ndata
Department of Orthopedics and Traumatology, Rwanda Military Hospital, Rwanda
Vianney Hope JM*, Paul Bitega J, Francis Mugabo, Edmond Mukimbili and Albert Ndata
Department of Orthopedics and Traumatology, Rwanda Military Hospital, Rwanda
Vianney Hope JM, Orthopedic and Spinal Surgeon, Department of Orthopedics and Traumatology, Rwanda Military Hospital, Rwanda.
Received Date: July 10, 2020; Published Date: July 23, 2020
Abstract
Dislocation of total hip prostheses is a multifactorial problem, with contributing factors from the patient, the implant, and the surgeon. It causes pain and patient dissatisfaction and must thus be reduced immediately or few days after its occurrence. Chronic dislocation of a total hip prosthesis refers to a dislocation which is unreduced at least 3 weeks (21 days) after its occurrence. We report clinical and radiological features, the surgical technique used for the treatment and outcome of a 11-year duration spontaneous chronic asymptomatic bilateral postero-superior dislocation of cemented total hip prostheses caused by excessive inclination of acetabular components in a 59-year-old patient. A 2-month-interval bilateral total hip revision has been carried out after continuous trans-condylar skeletal traction on Boppe splint. The patient made an uneventful recovery. At 7-year-follow up, the patient was satisfied with Postel Merle d’Aubigné score of 17/18 and Harris Hip Score of 99/100.
Keywords: Chronic dislocation; Asymptomatic; Bilateral total hip prosthesis; Revision.
Introduction
Total hip arthroplasty (THA) has become one of the most successful interventions in reconstructive orthopedic surgery. However, dislocation remains the well-recognized challenging complication for the surgeon and the cause for pain and dissatisfaction for patients. According to the registers, dislocation occurs after 0.3% to 10% of primary total hip arthroplasties and after up to 28% of revision total hip arthroplasties [1- 4]. Component malpositioning and abductor insufficiency are two of the most important recognized causes of dislocation [5-7]. Dislocation after THA is easily recognized immediately after its occurrence and reduced immediately or few days later. Therefore, chronic dislocation is exceptionally unusual. Only less than ten cases of unilateral chronic dislocation following THA have been reported to date [1-8]. We report the first case of chronic THA dislocation with bilateral involvement caused by a malpositioned acetabular component in a 59-year-old patient. We aimed to present clinical and radiological features, treatment, and outcome of spontaneous chronic asymptomatic bilateral dislocation of 11-year duration after cemented total hip arthroplasty.
Case Report
A 59-year-old man presented to the surgical clinic eleven years after single stage bilateral cemented primary THA following bilateral hip osteoarthritis. He was operated at another institution (abroad) and had never returned for follow up due to financial constraints. He remained pain-free, had 2 cm of true right leg length shortening with a good range of movement. Since the operation, he was unable to walk without orthopedic aids. However, he was able to walk unlimited distances with a rolling walker. Due to the dissatisfaction caused by long-standing limping associated with a leg-length discrepancy after THA, he decided to consult to our clinic. The patient denied any fall injury or accident. On general physical examination, he was healthy appearing; walking with bilateral axillary crutches; alert and oriented; responds appropriately; in no acute distress. His general status was conserved. Blood pressure measurement revealed a pressure of 155/85 mmHg, his pulse rate was 78 beats/minute, his respiratory rate was 19 cycles/ minute and his body mass index (BMI) was 27.8. There was right lower limb length discrepancy of 2 cm compared to the left side. A posterolateral operative scar, indicative of Austin Moore approach, was seen bilaterally.
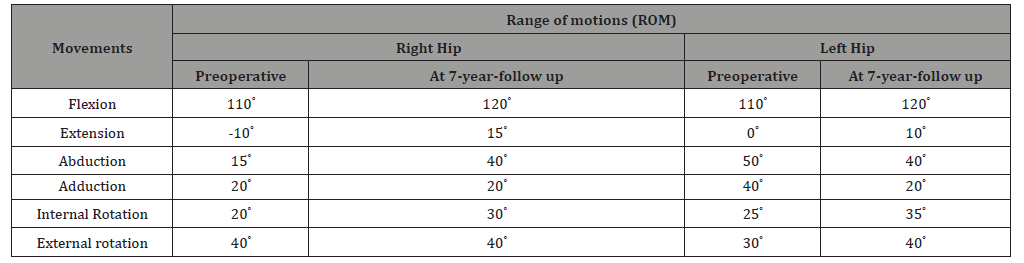
Musculoskeletal examination of the right hip showed that he could elevate the hell from the horizontal plane of the examination table; the muscle power of gluteal medius was at 3/5, adductor muscles at 4/5, hamstring muscles at 0/5 and quadriceps at 2/5. The hip flexion was at 110° and extension at -10°. On the left side, hell elevation from the horizontal plane of the bed was possible, muscle power of gluteus medius at 2/5, adductor muscles at 3 /5, hamstring muscles at 0/5 and quadriceps at 3/5. The hip flexion was at 110° and extension at 0°. Full range of motion (ROM) of both hips are presented in table 1. Postel Merle d’Aubigné (PMA) score was 10/18 and Harris Hip Score (HHS) 30/100 bilaterally. Neurovascular examination was unremarkable.
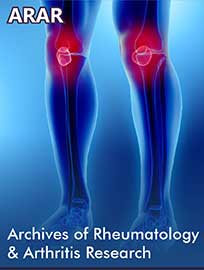
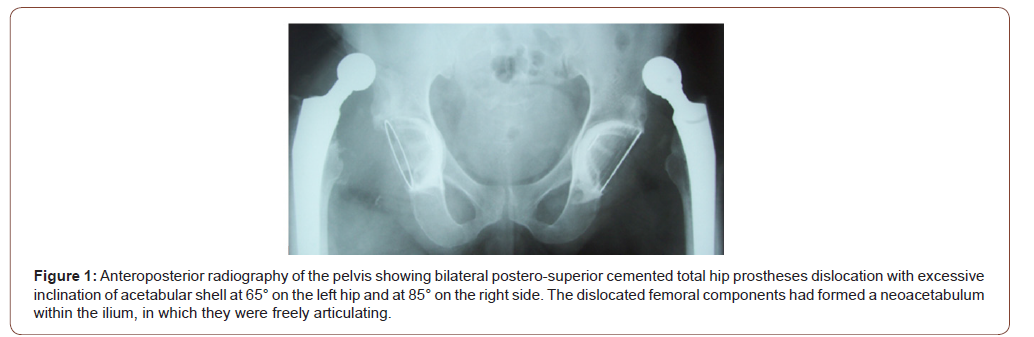
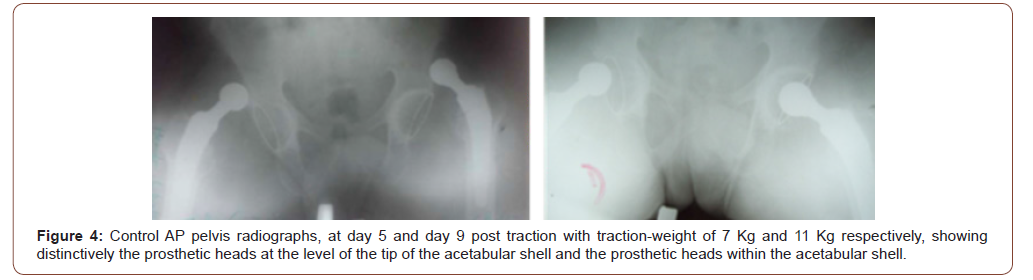
Conventional anteroposterior (AP) radiography of the pelvis showed bilateral postero-superior cemented total hip prostheses dislocation with excessive inclination of acetabular shell at 65° on the left hip and at 85° on the right side. The dislocated femoral components had formed a neoacetabulum within the ilium, in which they were freely articulating (Figure 1). Reconstructed axial and sagittal computed Tomography (CT) scans of both hips confirmed postero-superior total hip prostheses dislocation; muscle wastage with fat degeneration, aseptic loosening of both femoral and acetabular components with excessive inclination of acetabular components (Figure 2). The patient was put on bilateral trans-condylar skeletal traction using Boppe splint (Figure 3). Initial weight of 2 kilograms (Kg) was indicated with daily increase of 1 Kg and daily radiographic control to monitor the descent of the prosthetic heads. At day 5 post traction with traction-weight of 7 Kg, the heads were at the level of the tip of the acetabular shell. At day 9 post traction with traction-weight of 11 Kg, the heads were within the acetabular shell (Figure 4). The patient consented for a 2-month-interval bilateral total hip revision. Preoperative blood examination revealed WBC 8090/μl, Hb 11.4 g/dl, C-Reactive Protein 0.25 mg/dl, platelet 372000/μl, creatinine 10mg/l, uric acid 117mg/l and calcemia 87mg/l.

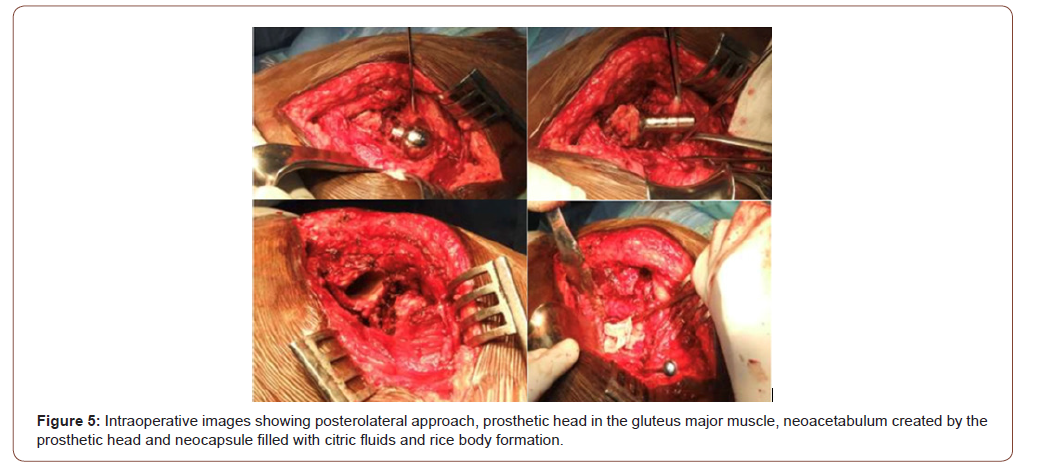
The right hip was first revised. In the left lateral decubitus position and under general anesthesia, the skin incision was made to the previous operative scar and hip was exposed through a standard posterolateral Austin Moore approach. Intraoperatively, a posterior and superior hip instability was identified as resulting from the combined movements of external rotation and adduction. We found that the prosthetic head has created a pseudoacetabulum and a neocapsule around it which was filled with citric fluids and rice body formations. The prosthetic head was found in the gluteus major muscle and both acetabular and femoral components were loosened with excessive inclination of acetabular component (Figure 5). We removed the implants along with the cement; and prepared for new implantation. Both acetabular and femoral components were revised using cemented modular shell and acetabular reconstruction with Kerboul reinforcement crossplate (acetabular lip). The femoral stem was cemented. The closure of the articular space and a good repair of the neocapsule and remaining short external rotators were performed. Intraoperatively satisfactory stability of the prosthesis movements in all directions was confirmed. The duration of the operation was 5 hours and the blood loss was 700 cc. The patient was transfused 2 units of whole blood. Postoperatively, the wound healed well by primary intention in 3 weeks. Two months later, the left hip was revised in the same way as the right one. Leg discrepancy was corrected. The second operation lasted 4 hours with blood loss of 600 cc. He was again transfused of two units of whole blood. The wound healed in 3 weeks.
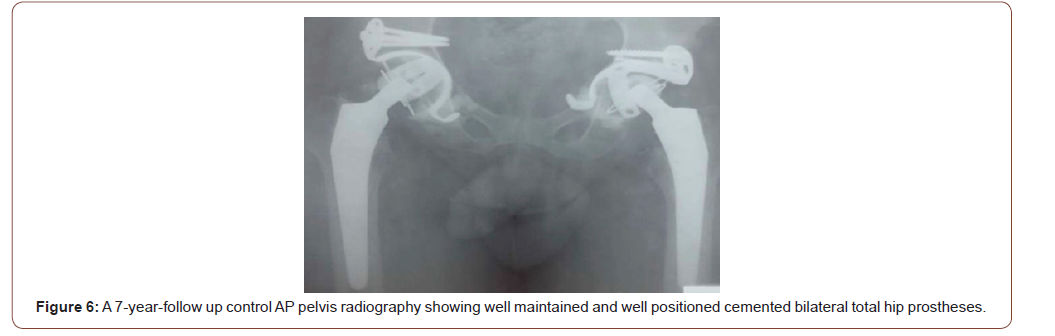
He was thereafter scheduled for rehabilitation and monthly follow up. He made an uneventful recovery and returned to fulltime employment 8-month post left hip revision. At 7-year-follow up, he was satisfied and pain-free. The ROM of both hips were satisfactory (Table 1). The PMA score was 17/18 whereas the HHS was 99/100. Control AP pelvis radiography show well maintained total hip prostheses. Femoral and acetabular components are well positioned and fixed. No signs of loosening or impingement were detected (Figure 6).
Table 1:Preoperative and at 7-year-follow up range of motion (ROM) of both hips.
Discussion
Dislocation following total hip arthroplasty (THA) is a complication which alarms both patient and surgeon. There have been numerous reports instancing the frequency of dislocation, with an overall incidence ranging from 0.3% to almost 10% after primary THA, with the highest risk believed to be within the first three months after surgery [1-5]. The incidence can be as high as 28% after revision surgery [9-15]. The definition of THA dislocation is complete loss of contact between the femoral head and acetabular component. This usually requires intervention to reduce the prosthetic head into the acetabular component. Dislocation may occur early or late and be single or recurrent. Early dislocation occurs in first 3 months postoperatively, and more than two dislocations are defined as recurrent [14]. The term chronicity refers to the time between the occurrence of dislocation and its reduction; thus, we have defined chronic dislocation as dislocation which is unreduced at least 3 weeks (21 days) after its occurrence. Very little has been written about chronic dislocation after THA, and less than ten cases of chronic dislocation following THA have been reported in the English literature. All these reported cases are unilateral [1-8]. We attribute the rarity of this lesion to the factor that hip dislocation is severely painful and patients with THA have a regular medical follow up. Thus, the dislocation is early diagnosed and immediately managed accordingly. At our center, the incidence of dislocation after THA is 0. 6%. For, this reported case of 11-year chronic asymptomatic bilateral dislocation, the primary THA was done in another institution and the patient failed to respect follow up program. Furthermore, the good range of movement and the absence of pain may explain the longstanding nature.
It may happen that an early postoperative total hip prosthesis dislocation is not diagnosed for few days in patients without weight-bearing, but this condition is extremely rare [16-17]. Often, THA dislocation is evident to both the patient and his neighborhood by the position of the dislocated limb and pain. The flexionadduction- external rotation and extension-abduction-internal motion positions are signs of posterior and anterior dislocation, respectively. Furthermore, in active patient’s total hip prosthesis dislocation may occur after a traumatic event (secondary or late dislocations). In our case, there is no possible link to traumatic events, and we think the dislocation is either spontaneous or positional.
Numerous factors influence the rate of dislocation after THA such as greater age, female gender, Musculo ligamentous laxity, previous surgery to the affected hip, revision surgery, infection, concomitant neurological deficiencies and other medical comorbidities, excessive alcohol intake, nonunion of the greater trochanter and cognitive impairment preventing adequate patient education. All cause soft-tissue imbalance and increase the risk of dislocation [9- 17]. Some authors have reported a higher rate of dislocation when using a posterior surgical approach and Kristiansen et al, noted less acetabular version with this approach [16-18]. Hedlundh U, et al. [19], registered twice the number of dislocations for inexperienced surgeons as compared with their more experienced colleagues, a correlation which was also reported by other authors [19]. Fackler CD and Poss R [20] observed a frequent association of dislocation with malposition of the component of which the surgeon was unaware at the time of surgery. This was seen more often among less experienced surgeons. The main reason for the higher rate of dislocation of inexperienced surgeons is malpositioning of the cup [20]. Soft-tissue imbalance and malposition are thought to be the two main causes of dislocation. Nonetheless, several authors have reported that excessive femoral anteversion may lead to dislocation [2]. Prosthetic design and selection can have an important effect on the incidence of dislocation. The most commonly considered implant factor is head diameter. In the author’s opinion, the perception that larger femoral heads would diminish the risk of dislocation [11]. In our case, there was excessive inclination of acetabular shell at 65° on the left hip and at 85° on the right side, and we have concluded that the cause of dislocation was malposition of acetabular components. There was soft tissue imbalance as a posterior dislocation injured the capsulo-muscular elements. Fortunately, the sciatic nerve was preserved. Intraoperatively, there were neocapsule around the prosthetic head which was filled with citric fluids and rice body formations which are the signs of chronicity. The prosthetic heads were found in the gluteus major muscle and both acetabular and femoral components were loosened.
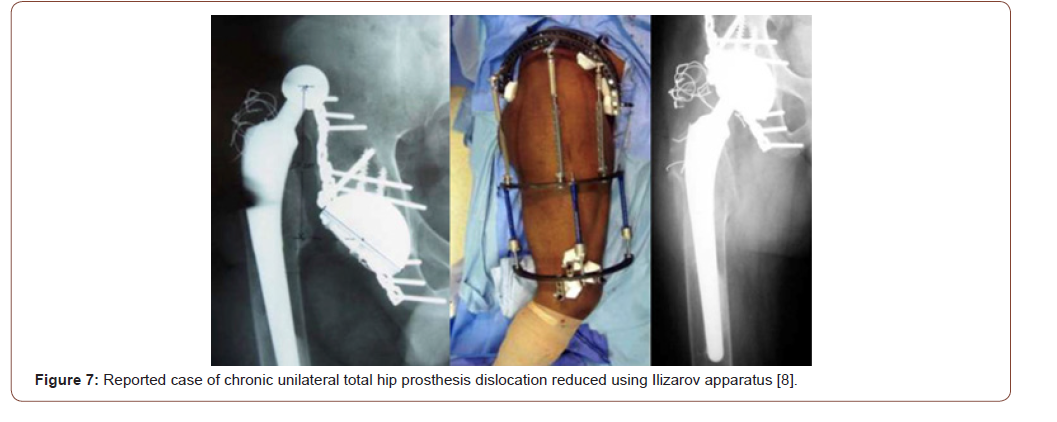
Prevention of dislocation is much easier than treatment. This includes careful pre-operative templating and surgical planning. Proper patient positioning, care of the soft tissues, precise component position, intra-operative assessment of stability, and leg length are compulsory. Treatment of dislocation after THA begins with an assessment of the cause. Component position should be carefully evaluated, and hip offset and leg length should be assessed [2-4,7,11]. Surgical options include exchange of modular components to increase soft-tissue tension, or a switch to a larger head diameter, including bipolar or tripolar arthroplasty, and use of an acetabular lip. Malposition and impingement must be corrected. Soft-tissue or trochanteric advancement, and the use of constrained liners should be a last resort [15, 21-25]. In case of chronic dislocation, Butler et al, have used an Ilizarov apparatus to perform closed reduction of a chronic dislocation following THA (Figure 7). In our case, we started with a skeletal traction with progressive increment of traction-weight to preserve the sciatic nerve injury by elongation and to prevent muscle injuries as muscles were already weakened by fat degeneration. After the prosthetic heads were in the acetabular shells, bilateral total hip revision was carried out with a 2-month-interval. As there were loosening of both femoral and acetabular components, both components were revised. Treatment outcomes were uneventful. At 7-year-follow up, he was pain-free with excellent functional satisfaction.
Conclusion
Chronic dislocation after total hip arthroplasty (THA) refers to unreduced dislocation at least 3 weeks (21 days) after its occurrence. It is believed that several factors contribute to chronic dislocation such as surgical approach, inadequate restoration of soft-tissue tension, prosthetic design, and orientation of the prosthetic components. We have reported an unusual case of a longstanding (11-year duration), but asymptomatic, dislocated bilateral total hip replacement in a 59-year-old man. Our case illustrates that a dislocated total hip replacement may occasionally not cause symptoms that cause significant discomfort or reduction in range of movement. The prosthetic femoral head can form a neoacetabulum allowing a full range of pain-free movement.
Statement of Informed Consent
Written informed consent was obtained from the patient to publish this article, along with his photographs.
Statement of Human and Animal Rights
All procedures were performed in accordance with the ethical standards of the responsible committee on human institutional and national experimentation and with the Helsinki Declaration of 1975, as revised in 2008.
Acknowledgement
None.
Conflicts of Interest
No conflict of interest.
References
- Lidder S, Ranawat VS, Ranawat NS, Tudor L Thomas (2009) Chronic asymptomatic dislocation of a total hip replacement: a case report. J Med Case Rep 19(3): 8956.
- Nellensteijn JM, Nellensteijn DR, De Jong T (2013) Case Report: Painless Chronic Liner Dissociation of a Total Hip Arthroplasty. Clin Orthop Relat Res 471(6): 1769-1772.
- Salvi AE, Florschutz AV, Grappiolo G (2014) Asymptomatic Chronic Dislocation of a Cemented Total Hip Prosthesis. West J Emerg Med 15(1): 107-108.
- Suh KT, Moon KP, Kim IB, Lee JS (2009) Open Reduction of a Chronic Proximal Dislocation After Total Hip Arthroplasty. The Journal of Arthroplasty 23(5): 791-793.
- Vaughn BK (1993) Managing Chronic Dislocated Total Hip Arthroplasty. Semin Arthroplasty 4(1): 16-24.
- Dorr LD, Wan Z (1998) Causes of and Treatment Protocol for Instability of Total Hip Replacement. Clinical Orthopaedics (355): 144-151.
- Parvizi J, Picinic E, Sharkey PF (2008) Revision Total Hip Arthroplasty for Instability: Surgical Techniques and Principles. Journal of Bone & Joint Surgery. 2008; 90(5): 1134-1142.
- Butler RA, Hsu JR, Barrack RL (2000) Use of an Ilizarov Apparatus to Perform Closed Reduction of a Chronic Dislocation Following Total Hip Arthroplasty. J Bone Joint Surg 88(2): 411-414.
- Alberton GM, High WA, Morrey BF (2002) Dislocation After Revision Total Hip Arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg 84(10): 1788-1792.
- Biedermann R, Tonin A, Krismer M, Rachbauer F, Eibl G, Stöckl B (2005) Reducing the risk of dislocation after total hip arthroplasty: The effect of orientation of acetabular component. J Bone Joint Surg [Br] 87(6): 762-769.
- Brooks PJ (2013) Total hip replacement: avoiding & managing problems. Dislocation following total hip replacement: Causes and cures. Bone Joint J 95-B (11 Suppl A): 67-69.
- Dargel J, Oppermann J, Brüggemann GP, Eysel P (2014) Dislocation following total hip replacement. Dtsch Arztebl Int 111(51-52): 884-890.
- Krenzel BA, Berend ME, Malinzak RA, Faris PM, Keating EM, et al. (2010) High Preoperative Range of Motion Is a Significant Risk Factor for Dislocation in Primary Total Hip Arthroplasty. J Arthroplasty 25(6 Suppl 1): 31-35.
- Meek RMD, Allan DB, Mc Phillips G, Kerr L, Howie CR (2006) Epidemiology of Dislocation after Total Hip Arthroplasty. Clin Orthop Relat Res 447: 9-18.
- Soong M, Rubash HE, Macaulay W (2004) Dislocation After Total Hip Arthroplasty. J Am Acad Orthop Surg 12(5): 314-321.
- Vicor AJ, Colemar CR (1984) A comparison of the anterolateral trochanteric and posterior surgical approach in primary total arthroplasty. Ciln Orthop (188): 152-159.
- Ali Khan MA, Brakenbury PH, Reynolds IS (1981) Dislocation following total hip arthroplasty. J Bone Joint surg 63-B (2): 214-218.
- Kristiansen B, Jorgensen L, Holmich P (1985) Dislocation following total hip arthroplasty. Arch Orthop Trauma Surg 103(6): 375-377.
- Hedlundh U, Ahnfelt L, Hybbinette CH, Weckstrom J, Fredin H (1996) Surgical experience related to dislocations after total hip arthroplasty. J Bone Joint Surg [Br] 78-B: 206-209.
- Fackler CD, Poss R (1980) Dislocation in total hip arthroplasties. Clin Orthop 151: 169-178.
- Di Schino M, Baudart F, Zilber S, Poignard A, Allain J (2009) Anterior dislocation of a total hip replacement. Radiographic and CT-scan assessment. Behavior following conservative management. Orthop Traumatol Surg Res 95(8): 573-578.
- Jolles BM, Zangger P, Leyvraz PF (2002) Factors Predisposing to Dislocation After Primary Total Hip Arthroplasty: A Multivariate Analysis. The Journal of Arthroplasty 17(3):282-288.
- Sikes CV, Lai LP, Schreiber M, Michael A Mont, Riyaz H Jinnah, et al. (2008) Instability after total hip arthroplasty: treatment with large femoral heads vs constrained liners. J Arthroplasty 23(7Suppl): 59-63.
- Zwartelé RE, Brand R, Doets HC (2004) Increased risk of dislocation after primary total hip arthroplasty in inflammatory arthritis: A prospective observational study of 410 hips. Acta Orthop Scand 75(6): 684-690.
- Masonis JL, Bourne RB (2002) Surgical Approach, Abductor Function, and Total Hip Arthroplasty Dislocation. Clinical Orthopaedics (405): 46-53.
-
Vianney Hope JM, Paul Bitega J, Francis Mugabo. Clinical Presentation, Treatment, and Outcome of Spontaneous Chronic Asymptomatic Bilateral Dislocation After Total Hip Arthroplasty: Unusual Case Report. Arch Rheum & Arthritis Res. 1(2): 2020. ARAR. MS.ID.000509.
-
Chronic dislocation, Asymptomatic, Bilateral total hip prosthesis, Revision, Hip arthroplasty, Boppe splint, Surgeon, Surgical technique
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.