Case Report
Case Report
Melioidosis Treatment Algorithm
Kewal Gangrade*
Department of orthopedic and arthroscopic surgeon, Bhopal, India
Kewal Gangrade, Department of orthopedic and arthroscopic surgeon, Bhopal, India.
Received Date:June 10, 2023; Published Date:January 09, 2024
Abstract
Melioidosis carries a very high mortality rate, clinical manifestation can range from acute fulminant sepsis to latent infection with 9% recurrence rate. The early diagnosis and long-term treatment plays a key role in patient recovery and in preventing recurrence. Being a mimicker of many other diseases, clinical suspicion and adequate diagnostic approach plays an important role in confirming melioidosis. It requires long term antibiotic control disease and prevent recurrence. In this series authors present the importance of clinical and specific radiological findings in raising an early suspicion of disease and modifying the laboratory work up accordingly to confirm the same and reduced morbidity and mortality.
Introduction
Melioidosis, a infectious disease caused by bacterium Burkholder Pseudo mallei acquired from contaminated water or soil [1]. It carries a very high mortality rate. Melioidosis infects approximately 165,000 people each year and kills 90,000. In addition, the recurrence rate is around 9% which further creates a health burden [2-4].
The early diagnosis and long-term treatment play a key role in patient recovery and in preventing recurrence. The successful outcome depends on confirmed microbial diagnosis, aggressive medical and surgical treatment. This case series covers the clinical aspects and treatment approach based on our experience with some red flag clinic-radiological signs to diagnose it early, melioidosis presentation can mimick other diseases and being missed many times [1, 5].
B Pseudo mallei is prevalent in southeast asia and was underdiagnosed in other subcontinent, but with improvement in diagnostic approaches, the incidence is rapidly increasing in rest of world [6, 7]. It is a gram-negative bacillus, lives in water, moist soil for months and replicates after rain. Humans acquire infection after exposure to contaminated water or soil during farming, wading or near drowning in floodwaters. It can enter the body by inoculation, inhalation or ingestion. Human-to-human transmission is extremely rare [2]. Patients having predisposing medical illnesses such as diabetes mellitus, alcohol addiction, chronic smokers, thalassemia, renal disease, chronic lung disease are at high risk of getting fulminant infection. Male population is at more risk compared to females.
Clinical presentation can range from acute fulminant disease to
latent infection with involvement of almost any organ in body [5, 8].
Clinical presentation can be categorized as,
a) Acute septicemic type-Presents as acute fulminant sepsis
and can lead to death in a day or two if not treated aggressively.
Difficult to differentiate from other endemic bacterial infection,
thus make diagnosis and treatment very difficult. The pathogen
is hematogenous disseminated to lung, liver, spleen, kidney,
skin, lymph nodes, subcutaneous tissue, bones, brain and forms
microscopic abscess. Jaundice, pneumonia, gastroenteritis
or meningitis may predominate clinically. The case fatality
rate is around 12-40% even with early antibiotic therapy and
intensive care [5].
b) Subacute stage - The patient presents with milder sepsis
and abscesses in lung, liver, spleen, psoas muscle, bone, brain,
eyes and soft tissues. If untreated the abscesses may progress
to chronic abscesses.
c) The chronic type follows the subacute type, either directly
or as a recurrence after treatment. The illness is characterised
by chronic abscesses, closely mimicking tuberculosis (even
histopathologic ally).
d) The latent or asymptomatic type may be detected
incidentally in patients who have lived in endemic areas. It can
lead to reactivation when the patient’s immunity fails [6, 7].
Table 1:Comparison of different forms of renal tubular acidosis.

Diagnosis
Non-specific laboratory findings include raised C-reactive protein (CRP) and anemia. The pathogen can be isolated by culture or detected by PCR from a wide range of specimens including blood, pus, sputum, urine, throat swab and cerebrospinal fluid. The pathogen grows on conventional culture media, but it is important to communicate with the laboratory staff unless they are familiar with melioidosis, because otherwise the growth may be discarded as a contaminant or Pseudomonas [9, 10].
Treatment
Early initiation of antibiotic therapy with adequate long-term regime is important to control and eradicate infection. Management of underlying disorders and surgical treatment of abscess or septic arthritis plays a crucial role in treatment algorithm. Treatment commences with an intensive phase therapy of 2-4 weeks with meropenem 1gram intravenous 8 hourlies to achieve resolution of fever, CRP levels and followed by eradication phase of 12-20 weeks with cotrimoxazole 320:1600mg 12 hourly combined with folic acid 5mg once daily to prevent recurrence [6, 11, 10].
Authors report a case series of melioidosis from central India over a short span of time duration that illustrates the difficulty of its diagnosis, risk factors, importance of aggressive treatment and do a brief review for literature on this topic.
Cases
Study included total of 12 patients being admitted to hospital over a short duration of time from June 2022 to February 2023. It includes patients presenting with fever and septic arthritis or abscess, which on workup turn out to be melioidosis..
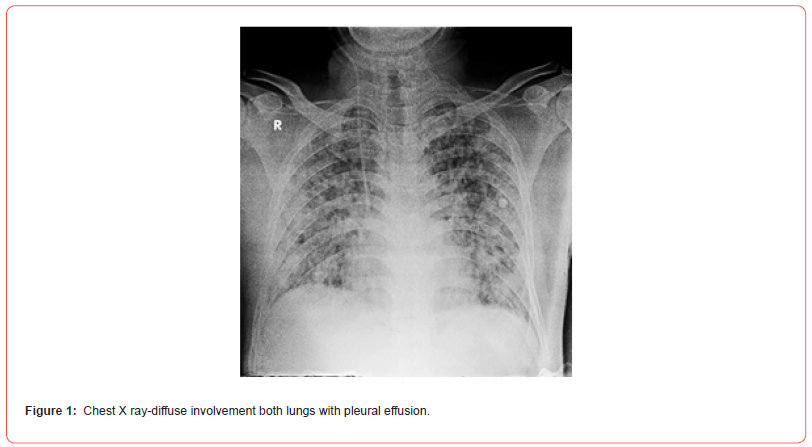
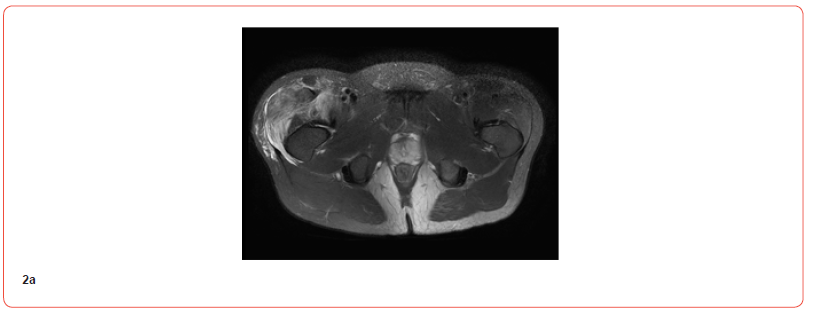
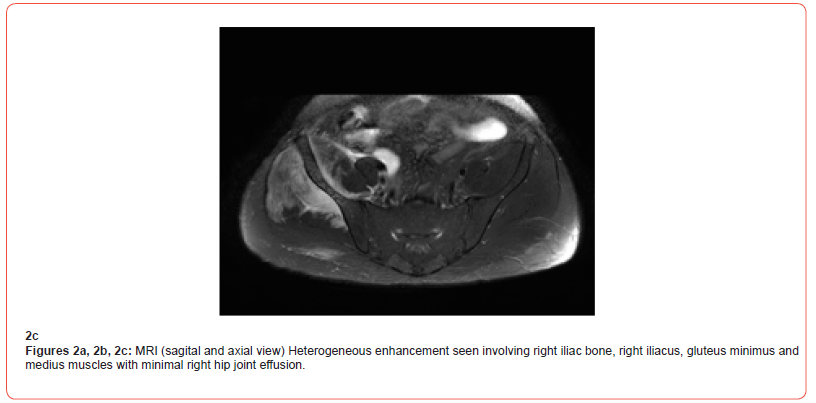
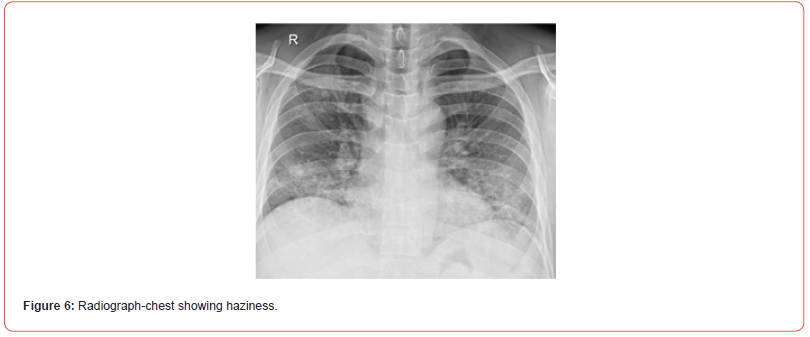
Two patient presented with acute fulminant sepsis had complaints of severe pain in his region, difficulty in walking and difficulty in breathing since 5-6 days. They were treated initially at another hospital. On admission they were evaluated clinicradiologically, and laboratory investigations sent. Synovial fluid aspirated from hip joint and sent for culture sensitivity along with blood culture. Considering the severity of sepsis, they were started on meropenem 1 gram intravenous 8 hourly. Chest radiograph findings of severe pneumonia changes were there and MRI hip suggestive of hip arthritis with involvement of metaphysis of femur and inflammatory changes in surrounding muscle compartment was noted. In spite of aggressive treatment approach with injectable antibiotics, fluids and oxygen support, both patients don’t respond and expired in 24 hours of admission time. The blood culture had grown pseudomonas species.

Six patients presented in subacute stage with complaints of septic arthritis involving the metatarsophalangeal joint right foot, inter-tarsal joint right foot and right knee joint respectively.
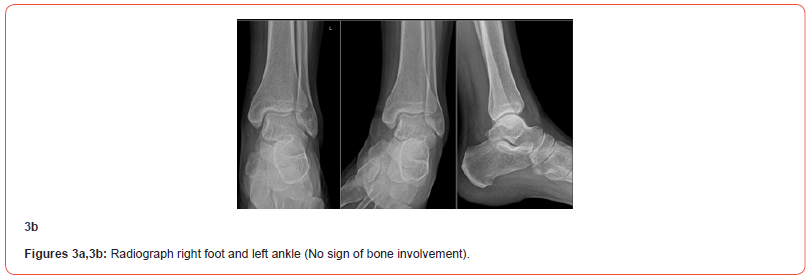
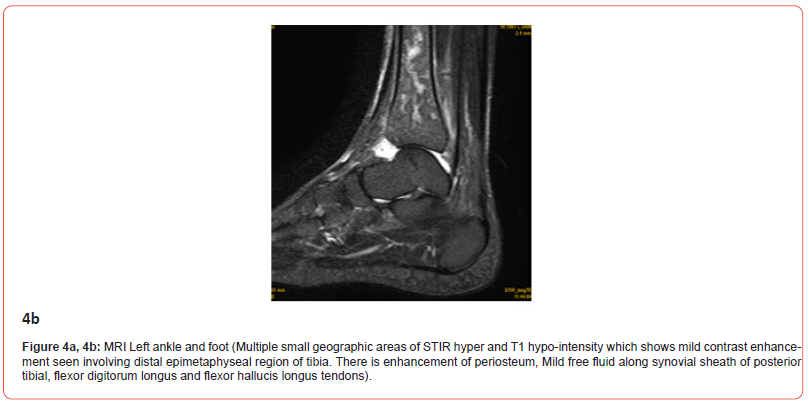
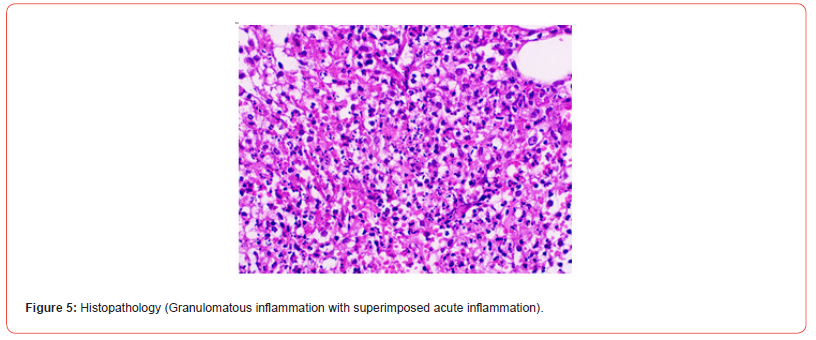
The first patient presented with complaints of pain and swelling right great toe, for which he was treated initially being gouty arthritis. But over 5-6 days he developed an abscess around MTP joint of great toe, which was debrided and sent for culture. Culture came out to be negative. Another lab workup patient was diagnosed with borderline diabetes and over the next 7 days he started getting severe pain in left ankle and leg. MRI findings were of inflammatory or infective etiology. Since clinically patient was not responding to anti-inflammatory and analgesics, decision made to debride the ankle. Tissue and fluid from ankle sent for histopathology and culture by coordinating with microbiologist to consider pseudo mallei. Patient started on meropenem 1g intravenous 8 hourlies. The culture came positive for the same and patient respond well to intensive and eradication phase treatment.


The second patient with inter-tarsal arthritis was treated primarily else over 2-3 weeks duration but doesn’t respond to antibiotics. On admission MRI, laboratory workup along with blood cultures sent. Five days later he started developing knee synovitis and effusion, for which knee aspiration was done and fluid sent for culture. Blood culture reported as pseudomonal growth. As per culture, the patient is being started on intesive phase with meropenem. Inflammation and pain responded well to antibiotics.
Third patient came with complaint of septic arthritis knee, for which knee aspiration done and fluid sent for cultures. Patient denied further treatment and took discharge on day 2. The fluid cultures came positive for pseudomonas growth.
Another two-patient presented with fever and joint pain of 2 to 3 weeks duration. They were earlier treated else with injectable antibiotics from cephalosporin group but doesn’t responded and joint pain and swelling persisted. On evaluation with joint aspiration, fluid culture and blood culture they reported to be pseudomonal growth in culture media. They started intensive phase therapy of 2 weeks. Patients respond well to meropenem over 3-4 days of starting it.
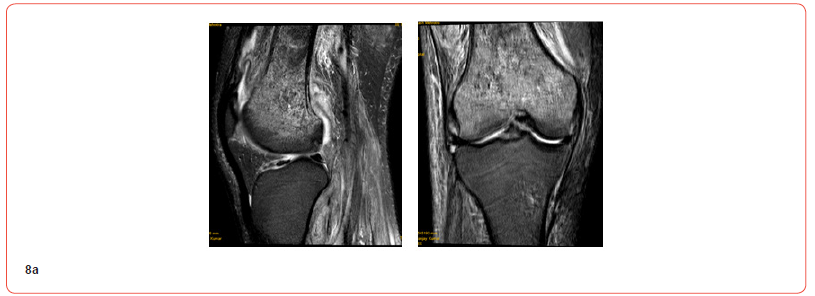
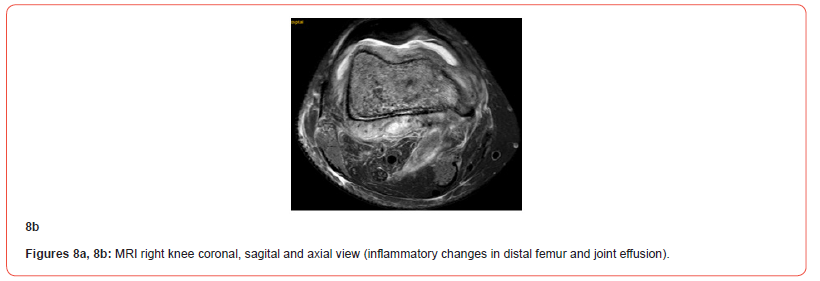
Sixth patient a known diabetic and hypertensive presented with synovitis right knee since 2-3 weeks. MRI findings were of septic arthritis with involvement of proximal tibia showing marrow changes. Knee arthrotomy and debridement done. Culture from site were negative. Patient kept on empirical antibiotics, to which he responded partially. One month later patient presented with pain and swelling in opposite knee and thigh. On MRI there was knee effusion along with involvement of distal femur marrow changes.
The aspirate from knee sent for culture, which came out positive for Burkholder. Patient started on meropenem to which he responded well and being kept on trimoxazole for 6 months.
Other four patients presented as chronic stage with history of either uncontrolled diabetes or severe pneumonia for which treated at other center with injectable antibiotics.
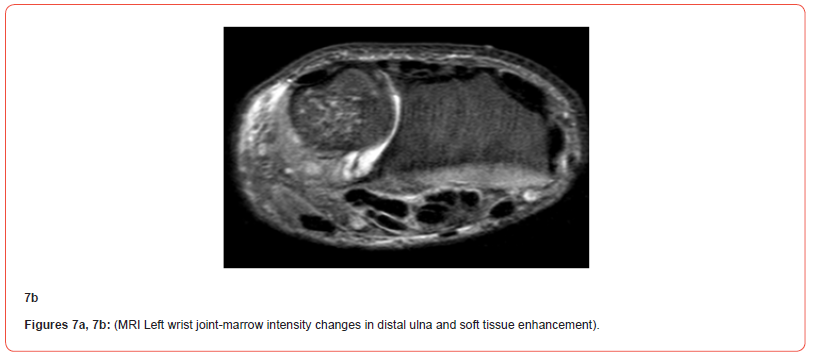
One patient presented with history of severe pneumonia and joint pain for which he was kept on ventilatory support and injectable antibiotics for 5 to 7 days due to respiratory failure. Three weeks post recovery from pneumonia patient developed severe pain and swelling right knee, ankle and fever episodes. Laboratory work-up was not conclusive. Knee joint fluid and blood culture sent. As patients were not responding to empirical antiobiotic , the debridemnt surgery planned for knee and ankle and tissue sent for culture. As per history we suspected melioidosis as differential and started him on meropenem, to which he responded well. Patient started on meropenem 8 hourly and clture report confirmed the Burkholderia psudomonas growth at 5th day. Over next 4-5 days he started developing pain and swelling left wrist, which was not improving inspite of strong analgesics. Surgical debridement of distal ulna done, patient had immediate pain relief from next day of surgery. Meropenem continued as per intesive phase for 2 weeks along with co-trimoxazole 12 hourlies. The surgical wound kept open and patient kept on regular dressing, over a 3 weeks’ time surgical wound healed well and patient was able to ambulate without support and knee, ankle and wrsit movements were free.

Another patient, a known diabetic presented with septic arthritis right knee. The knee joint aspirated and fluid sent for culture. Considering the MRI changes of septic knee with marrow changes in distal femur, debridement surgery performed and patient started on meropenem as per positive blood culture and synovial fluid cultures. The surgical wound kept open and regular dressing continued. The wound healed over next 3 weeks’ time. Patient responded well to meropenem.
Discussion
The incidence of disease is rapidly increasing in India [5, 12]. It is estimtaed to be around 44% of global disease in South Asia and being most prevalent in Bangladesh, Sri Lanka and Pakistan [13, 4]. Melioidosis has high case fatality range from 16-50 % and according to study by Direk L and Nick G there is around 165,000 human melioidosis cases per year worldwide, of which 89,000 die. Authors highlighted the underreporting of this condition in many endemic zones and the possibility of rise in disease burden [14, 15].
In India most cases being reported from southwestern coastal Karnataka and northeastern Tamil Nadu. This most likely reflects the presence of research centers capable of diagnosing and treating melioidosis [4]. This case series is probably the first of its kind from centra India with culture proven diagnosis. From literature Currently, India has no surveillance data for melioidosis, so there are no exact numbers of cases [4, 11].
Risk factors for contracting melioidosis include pre-existing conditions such as diabetes mellitus, chronic alcohol usage, smoking, chronic lung disease and chronic renal disease. The most common comorbidity of melioidosis is type two diabetes mellitus. The prevalence of DM detected in this study is comparable to those of other cohorts from literature review.
Outbreaks are most common after heavy rainfall, typhoons, monsoons, and flooding in general. The association of acute melioidosis with the wet season in certain regions concurs with other studies that there is a connection between illness and rainfall intensity [16]. Soil erosion and higher turbidity levels are associated with a greater prevalence of the bacterium [14].
Various authors have pointed out that there can be a wide variety of clinical presentations, with average duration ranging from few days to few months. Pulmonary involvement is the most common presentation, followed by splenomegaly, abscesses, septic arthritis and osteomyelitis. Incidence of sepsis reported by Birnie, et al. in there study correlates with our case series [17].
Helpful clues to suspect melioidosis may include seasonal occurrence during rains and epidemiological exposure to water or soil and rapid progression to sepsis. In our case series the greatest number of cases presented in subacute stage with involvement of large joint, which was not responding to routine antibiotic preparations. The patient who was suspected and started on meropenem responded very well.
Localized infections are presented as pain or swelling in joint, abscesses with or without history of fever. Patient who had pulmonary infections presented with cough, chest pain, fever and loss of appetite. Blood stream infections typically consist of fever, headache, respiratory distress, abdominal discomfort and joint involvement. Disseminated infections without any specific treatment may develop sepsis with central nervous system involvement. Melioidosis is an opportunistic infection that is unlikely to kill a healthy person [12, 9]. In this study all of patient were having some medical illness most common being diabetes and many of patients had pulmonary and joint involvement as a primary symptom, while many of previous studies reported joint involvement as infrequent finding contrary to our case series.
Misdiagnosis is a common problem in areas of the world where the disease isn’t well known. Melioidosis can be diagnosed by using the patient’s bodily fluids to grow cultures [5]. Unfortunately, this process is time-consuming, and it may take up to seven days to confirm the diagnosis [3, 10]. It is possible that patients will die before the disease is confirmed to be melioidosis, due to likely ineffective antibiotics. If infection is suspected, it can be confirmed in laboratory by detection- isolation, culture identification and genotyping. Recently, researchers have been able to design multiplexing four single plex PCR assays that can identify various strains that fall under the Burkholder pseudo mallei complex [3, 11].
A lateral flow immunoassay (LFIA) is gaining popularity as a point of care test. The LFIA had an average specificity of nearly 100%. LFIA takes a few minutes, which detects the capsular polysaccharide antigen of B. pseudo mallei directly from tissue samples [10]. LFIA, though promising in authors study, has limitation of being availability and high cost.
The other diagnostic modalities utilized for assessment are ultrasonography, CT and MRI scan to confirm the disease extension. The lung is commonly involved, and chest radiographs show multifocal nodular, patchy consolidation with cavitary lesions. There may be rapidly progressive patchy consolidation and enlarging coalescent nodules. The lung consolidation can be in any lobe of the lung, progressing to abscess and cavity formation that mimics tuberculosis. The importance of an early diagnosis cannot be overemphasized, as it progress rapidly if pulmonary involvement is there. If patient is presenting during or post rainy season with probable history of exposure to bacteria and involvement of lungs with other signs such as myositis, septic arthritis that is not responding to analgesic and antibiotics of 48 hours one should keep Melioidosis as differential and work up should be done accordingly and microbiologist also be informed regarding the same so fluid or blood cultures can be performed accordingly.
The presence of common broad-based signs and symptoms, the clinical diagnosis is usually missed or delayed because of a lack of awareness or familiarity with this disease. The radiological findings may help to streamline our diagnostic and treatment approach. South Asia, where tuberculosis is widely prevalent, any disease like tuberculosis is misdiagnosed, leading to a delay in proper management Burkholderia pseudomallei looks like Pseudomonas sp, a common contaminant and is easily misidentified in microbiology laboratories. The diagnosis is often overlooked because of blood or tissue culture’s low diagnostic sensitivity (nearly 60%) [8, 16, 14]. To our experience tuberculosis rarely shows involvement of two or three joints simultaneously, while patient who presented to us with Melioidosis has two or three joint involvements either simultaneously or over in a sequence over a very short duration. Thus if patient is known diabetic with history of exposure and clinical presentation of septic arthritis of two or more joints and radiological picutre of joint involvement with secondary bony inflammatory changes should raise suspicion of meioidosis.
In the acute septicemic type, early intensive care for sepsis is crucial. Abscesses or septic joints should be surgically debrided if large enough and painful. Detection and treatment of predisposing conditions such as diabetes, kidney disease and immunosuppression are important. In this case series there were three patient who presented in acute septic stage with gross involvement of chest and major joints. They could not be reviewed in spite of aggressive intensive treatment; possible reason can be a delayed presentation to us. If patient being presented at onset of symptoms and started on meropenem at day 1 or 2 of symptoms, possibly patient could have been reviewed. But due to lack of awareness regarding severity of melioidosis and treatment approach patients fail to get proper treatment at the beginning. This case series tries to raise awareness regarding condition, type of clinical presentation, diagnostic approach and aggressive treatment protocol to be followed to get best outcome.
Patient who presented to us in subacute and chronic stage were initially treated at other centers with various antibiotics but failed to respond and condition kept on deteriorating, later when they presented at our center, considering the possibility of melioidosis as differential patients shifted to meropenem and within 2-3 days of starting it patient started showing clinical improvement.
B pseudo mallei is intrinsically resistant to the bactericidal antibiotic’s penicillin’s (except co-amoxiclav), third generation cephalosporins (except ceftazidime), aminoglycosides. It is relatively resistant to quinolones and macrolides. Among bacteriostatic antibiotics, it is sensitive to cotrimoxazole and tetracyclines.
Antibiotic treatment is given in two phases. Treatment commences with an intensive phase of 2–4-week duration, to achieve stabilization, resolution of fever and improvement in CRP level. Then treatment moves to the eradication phase, to prevent recurrence of disease. Current choice is between ceftazidime and carbapenems (imipenem or meropenem). In the acute septicaemic and subacute types, since microbiological diagnosis is not immediately available and the differential diagnosis is wide, a carbapenem is the frequent choice (often combined with other empirical antibiotics such as vancomycin). In the other types, since antibiotic treatment is often commenced after microbiological diagnosis, ceftazidime can be the choice. Oral cotrimoxazole can be started from begining if there are significant deep-seated foci not amenable to surgical drainage or severe pulmonary involvement.
With successful treatment the patient will stabilise and begin to feel better in a 5-7days time. But the fever and high CRP levels may continue for a week or more and blood cultures may continue to yield the organism. There is no need to reconsider the antibiotic regimen if the patient is clinically improving and CRP is reducing. The time of switching from intensive to eradication phase must be judged carefully, because this is a common time for recurrence. Though few studies suggested to continue intensive phase till negative blood cultures, but to our experience inspite of clinical and CRP improvement, the blood culture can remain positive at 2-3 weeks of antibiotics.
For the eradication phase, current choice is between cotrimoxazole, doxycycline and chloramphenicol. Since the eradication phase lasts for months, the side effect profile must be carefully considered in relation to the patient. Although high-dose cotrimoxazole (320:1600mg 12-hourly) has been recommended, it is not usually well tolerated over prolonged periods. Folic acid should be prescribed along with cotrimoxazole.
In survivors, the commonest long-term complication is recurrence of infection. It is important to educate the patient that re-infection is possible, because about half of recurrences are believed to be due to re-exposure and reinfection [7, 6]. In addition, a quarter of septicemic patients relapse despite taking antibiotics, which led to the concept of having a second round of eradication treatment [9, 10]. In our case series patients are under follow up to assess clinical improvement and being counselled regarding recurrence risk and importance of regular follow ups.
There is limited knowledge of melioidosis in India because people from poor, rural regions are underdiagnosed. There is speculation that India will lead the global melioidosis map by 2030 with the highest predicted cases due to the number of diabetics in the country [13, 14]. Melioidosis has the potential to spread to areas where it isn’t typically found. Travelers who visit endemic areas can contract infection and transfer it to other places. This can be a possibilty of rise in incidence in central India.
A limitation to note is that, as a tertiary care center sample size is small, but relatively speaking, in context to the present Indian scenario, most cases were reported in a very short duration, and this is a probably a first report from centra India with wide range of patients and detailed clinic-radiological findings.
Conclusion
One should have a high index of suspicion in patients presenting from endemic zones and having pulmonary and joint infection. Radiology and fluid cultures help to confirm the diagnosis. In the acute septicemic and subacute types, early aggressive therapy is essential to save life. Surgical drainage of abscesses and septic joints helps in early recovery and rapid response to antibiotics. Patients having either chronic kidney disease or high CRP levels (more than 100 IU/l) or hypoalbuminemia should be identified as high-risk patients and require close monitoring to pick up complications. Counselling of patients regarding importance of proper antibiotic regime for 5-6 months and possibilty of recurrence should be explained.
Conflict of interest
None.
Acknowledgements
No conflict of interest.
References
- Panduka K (2022) CME tropical medicine. Clinical Medicine 22(1): 6-8.
- Dance DA (2000) Melioidosis as an emerging global problem. Acta Tropic 74(2-3): 115-119.
- L Morici, A G Torres, R W Titball (2019) Novel multi-component vaccine approaches for Burkholderia pseudomallei. Clinical and Experimental Immunology 196(2): 178-188.
- Chiranjay Mukhopadhyay, Tushar Shaw, George M Varghese, David A B Dance (2018) Melioidosis in South Asia (India, Nepal, Pakistan, Bhutan and Afghanistan). Tropical Medicine and Infectious Disease 3(2): 51.
- Cheng AC, Currie BJ (2005) Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev 18(2): 383-416.
- Peacock SJ, Limmathurotsakul D (2017) Melioidosis, Infectious Disease, (4th edn,) vol 2. Elsevier, 2017:1073-1077.
- R Gopalkrishnan, D Sureshkumar, M A Thirunarayan, V Ramasubramanian (2013) Melioidosis: an emerging infection in India. J Assoc Physicians India 61(9): 612-614.
- Kusugodlu R, Kavitha S, Chiranjay M, Ananthakrishna S B (2013) Melioidosis: an underdiagnosed disease in India (epidemiology, clinical features, and outcomes). Asian Biomedicine 7(2): 249-256.
- Timothy J J Inglis, Dionne B Rolim, Anástacio De Queiroz Sousa (2006) Melioidosis in the Americas. American Society of Tropical Medicine and Hygiene 75(5): 947-954.
- Lowe, Benjamin A Satterfield, Daniel B Nelson, Joseph D Thiriot, Michael J Heder, et al. (2016) A Quadruplex Real-Time PCR Assay for the Rapid Detection and Differentiation for the Most Relevant Members of the B.pseudomallei Complex: B. mallei, B. pseudomallei, and B. thailandensis 11(10): e0164006.
- Vivek Pandey, Sripathi P Rao, Sugandhi Rao, Kiran Kv Acharya, Sarabjeet Singh Chhabra (2010) Burkholderia pseudomallei musculoskeletal infections (melioidosis) in India. Indian J Orthop 44(2): 216-220.
- Cheng, Currie (2005) Melioidosis: Epidemiology, Pathophysiology, and Management. Clinical Microbiology Reviews 18(2): 383-416.
- Prasant R M, B Mala (2022) Burden of melioidosis in India and South Asia: Challenges and way forward.
- L Manivanh, A Pierret, S Rattanavong, O Kounnavongsa, Y Buisson, et al. (2017) Burkholderia pseudomallei in a lowland rice paddy: seasonal changes and influence of soil depth and physico-chemical properties. Scientific Reports 7(1):3031.
- Direk L, Nick G, David AB D, Jane P Messina, David M Pigott, et al. (2016) Predicted global distribution of Burkholderia pseudomallei and burden of melioidosis. Nat Microbiol 1(1): 15008.
- K Vidyalakshmi, S Lipika, S Vishal, S Damodar, M Chakrapani (2012) Emerging clinico-epidemiological trends in melioidosis: analysis of 95 cases from western coastal India. International Journal of Infectious Diseases 16(7): e491-7.
- Raviraj Menon, Poornima Baby, Anil Kumar V, Sandeep Surendran, Manu Pradeep, et al. (2021) Risk Factors for Mortality in Melioidosis: A Single-Centre, 10-Year Retrospective Cohort Study. Scientific World Journal 2021: 8154810.
-
Richmond Ronald Gomes, Habiba Akhter. A Rare Case of Recurrent Hypokalemic Paralysis Associated with Distal (Type1) Renal Tubular Acidosis Due to Primary Sjogren’s Syndrome with Type 3 Cryoglobulinemic Vasculitis with Autoimmune Hypothyroidism. Arch Rheum & Arthritis Res. 2(2): 2022. ARAR.MS.ID.000550.
-
Postural orthostatic tachycardia syndrome, Neuropathy, Autoimmune diseases, Inflammation, Rheumatoid arthritis, chronic fatigue syndrome, Immunizations.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.