 Case Report
Case Report
Successful Clozapine Trial After Leucopenia/ Neutropenia Secondary to Haloperidol Plus Quetiapine: Ten-Year Follow-Up Case Report
Emerson Arcoverde Nunes1*, Lízie Emanuelle Eulálio Brasileiro2
1 Department of Clinical Medicine, Onofre Lopes University Hospital – Federal University of Rio Grande do Norte, Brazil
2Multicampi School of Medical Sciences of Rio Grande do Norte – Federal University of Rio Grande do Norte, Brazil
Emerson Arcoverde Nunes, Department of Clinical Medicine, Onofre Lopes University Hospital – Federal University of Rio Grande do Norte, Brazil.
Received Date:September12, 2023; Published Date:September 21, 2023
Abstract
Introduction: Antipsychotics can cause neutropenia, but with haloperidol, this has been reported rarely. Here we report a case of neutropenia
caused by haloperidol plus quetiapine in a patient with treatment-resistant schizophrenia, managed with haloperidol withdrawal, and the successful
later trial with clozapine.
Case report: 27-year-old man, with treatment-resistant schizophrenia, symptomatic for 3 years despite apparent regular use of medications.
He arrived at our service using quetiapine 800mg, associated with haloperidol 10mg/day, still presenting auditory hallucinations and persecutory
delusions, in addition to bradykinesia, facial hypomimia, and discrete tremors of the extremities. With indication of the use of clozapine, he had an
altered leukocyte count, with a leukocyte count of 2700 (with an absolute neutrophil count - ANC - of 1350). After hospitalization and withdrawal of
antipsychotics, his blood count and motor symptoms improved, while hallucinations and delusions continued. It was decided to carefully introduce
clozapine, with blood counts performed every two days. He was discharged after 40 days, using 300mg of clozapine, with significant improvement
in symptoms, without changes in blood count. He has been attending the schizophrenia clinic at the University Hospital regularly for 10 years, with
normal blood counts, with good functionality, and minimal residual symptoms.
Discussion: Cases of leukopenia with the use of both haloperidol and quetiapine exist in the literature, and their association probably increases
the risk of such side effects. To our knowledge, this is the first reported case of important leukopenia/neutropenia due to the association of
haloperidol with quetiapine with subsequent successful exposure to clozapine.
Conclusion: Although hematological changes may contraindicate the use of clozapine, careful introduction with more frequent blood tests
seems to be an appropriate option in refractory cases such as the one presented here.
Keywords:Case report; Neutropenia; Clozapine; Haloperidol; Quetiapine
Introduction
Any antipsychotic can cause neutropenia, but with haloperidol, this has been rarely reported. It has already been shown that both typical and atypical antipsychotics can lead to leukopenia, neutropenia, and agranulocytosis as adverse effects, threatening life or even the continuity of treatment, with the consequent resurgence of psychotic symptoms [1]. Moderate leukopenia (white blood cell count less than 3,000 per mm3), decreased absolute neutrophil count (less than 2,000 per mm3) and agranulocytosis (neutropenia less than 500 per mm3) are the main blood changes, especially related to the use of clozapine [Table1] [2-6]. Atypical antipsychotics that have closer structure similarities with clozapine, like olanzapine and quetiapine have been mostly described as causes of blood cell count changes [1], although these cases are not enough to raise concern in clinical practice about the occurrence of blood dyscrasia with antipsychotics other than clozapine, even if more recent publications suggest that this risk is not so different between antipsychotics and clozapine [7]. One of the biggest challenges in clinical practice in the management of treatmentresistant schizophrenic patients who have already experienced an episode of antipsychotic-associated neutropenia/leukopenia is the need to use clozapine in an individual at increased risk of white blood cell count changes [8-10]. Here we describe a case report of a ten-year follow-up of a successful clozapine trial after neutropenia secondary to haloperidol plus quetiapine.
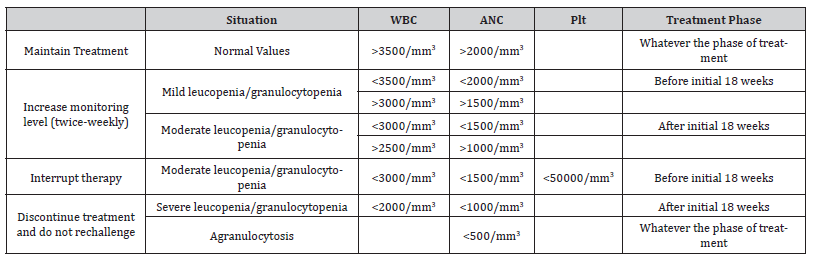
Table 1:Clozapine hematological monitoring and appropriate management based on CBC results [6].
Case Report
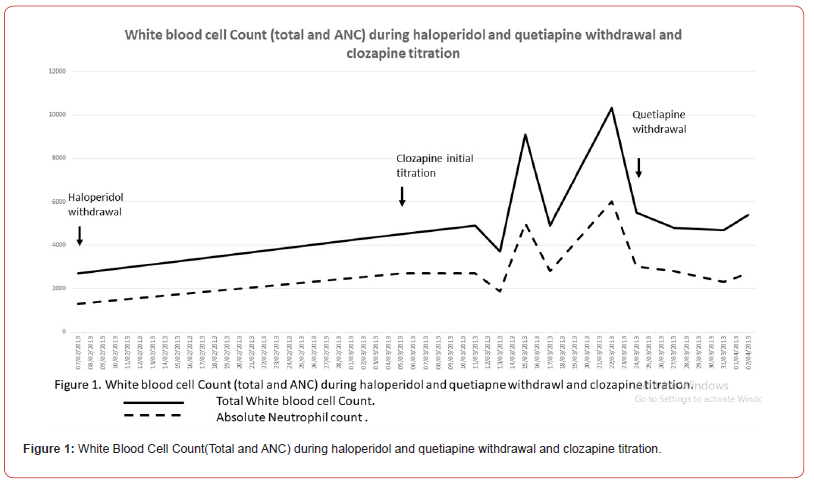
A 27-year-old man with treatment-resistant schizophrenia, came to a first visit to the outpatient clinic, after a few years of symptoms despite regular use of medication. Symptoms began when he was working, three years ago, when he began to hear voices that cursed him and commented on his behavior. He started to get aggressive with co-workers, even assaulting one of them. He started treatment in an outpatient clinic in the city, with haloperidol, up to 10mg/day, without improvement of symptoms, with worsening of social isolation, in addition to presenting motor slowing. Risperidone and olanzapine were tried, with no apparent improvement in each trial, so quetiapine was tried. Despite reaching 800mg/day, he kept hallucinating. They opted for the association with haloperidol, thus arriving at our outpatient clinic, using quetiapine 800mg, associated with haloperidol 10mg/day, still presenting auditory hallucinations and persecutory delusions, in addition to bradykinesia, facial hypomimia, and discreet tremors of the extremities. It was indicated for the use of clozapine, he had an altered leukogram, with a leukocyte count of 2700 (1300 neutrophils). Initially, haloperidol was reduced, and was introduced lithium carbonate, leading to an increase in the white blood cells (leukocyte count of 9000, 4000 neutrophils). The quetiapine and the other medications were maintained for the slow withdrawal. The patient was admitted to the inpatient care to perform a careful introduction of clozapine, with a blood cell count performed every two days. The quetiapine and the lithium carbonate were then removed day by day, while it was introduced clozapine with slow titration and permanence of the normal hematological values. After hospitalization and withdrawal of haloperidol, the patient evolved with an improvement of motor symptoms, maintaining hallucinations and delusions. He was discharged after 40 days, using 300mg of clozapine, with significant improvement of symptoms, without changes in blood count [Figure 1]. He has been regularly seen at the schizophrenia outpatient clinic at the University Hospital for more than ten years, coming asymptomatic with normal blood counts.
Discussion
The case described reports a case of management of treatment-resistant schizophrenia, demonstrating response and improvement in the patient’s quality of life after exposure to the atypical antipsychotic most associated with blood dyscrasia, even after hematological alterations with another antipsychotic, with a follow-up period of ten years of observation after the introduction of clozapine. Treatment-resistant schizophrenia has been defined using the following criteria: history of partial or total lack of response using 2 antipsychotics in appropriate doses and periods, with permanence of psychopathological symptoms [11]. Although clozapine has been recognized as the antipsychotic most implicated in leukopenia and agranulocytosis, other neuroleptics have also been linked with blood dyscrasias, such as olanzapine, quetiapine, risperidone, and haloperidol [12-15]. Due to the high mortality caused by agranulocytosis, consequent to drugs in which blood tests are not mandatory, there is a need to reconsider the value of the hematological routine [7].
Some authors report cases of neutropenia with the use of olanzapine, often this drug being implicated in neutropenia after “sensitization” of clozapine [1,9]. Blood dyscrasia resulting from the use of haloperidol is rarely described, although there are some reports, including one recent report of haloperidol-related neutropenia [14]. Leukopenia and neutropenia related to the association of antipsychotics also had already been described [16], what was noted in our case, was that haloperidol was previously tried without blood count changes, but the patient presented with neutropenia during the association of haloperidol and quetiapine, with posterior normalization of the total leukocyte and neutrophil count with the withdrawal of haloperidol. Following the withdrawal of haloperidol, we decided to start lithium carbonate because there are studies that demonstrate that it can cause a reversible leukocytosis, as well as maintain the neutrophil count in children and adults, although studies are still scarce and with a small number of samples [17].
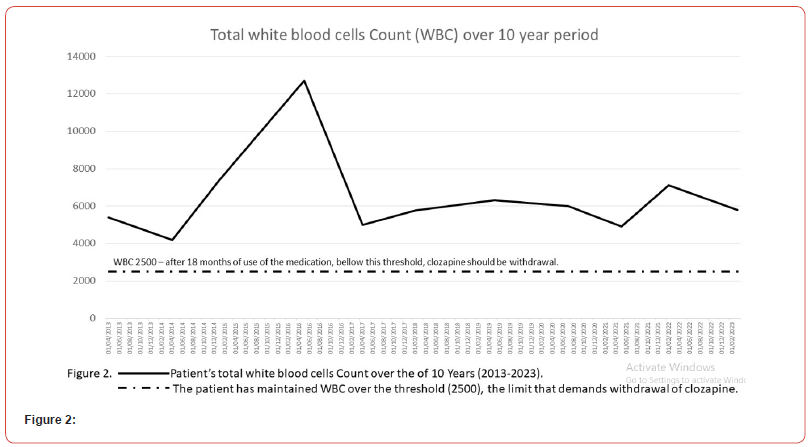
The chemical structure of quetiapine is similar to that of clozapine, although the former’s safety in terms of leukopenia, neutropenia, or agranulocytosis is superior [4,13]. Clozapine is metabolized by peroxidases, which form a reactive metabolite that binds to cellular proteins covalently in white cells, exerting its toxicity. In the structure of quetiapine, there is no bioactivation by peroxidases in the nitrous ion, however, it has a hydroxylated metabolite that covalently binds to white cells in the sulfhydryl group of nucleophiles [4]. There is a recent case report of agranulocytosis after a clozapine trial following quetiapineinduced leukopenia, raising even more questions about the safety of clozapine in a patient who has previously experienced leukopenia and neutropenia with quetiapine [18]. After the introduction of clozapine in the hospital environment, leukocytes and absolute neutrophil counts were maintained in the normal range, and the follow-up of ten years did not show any alteration suggesting leukopenia or neutropenia [Figure 2]. It is known that alteration of the white blood series is the main concern with the use of clozapine, with the risk of agranulocytosis being 1 in 100 patients [3,6,19]. Patients with a history of blood dyscrasia with an antipsychotic would be more likely to have dyscrasia with an antipsychotic of the same chemical class [17], but this correlation was not observed. Our case differs from this previous report mainly because it was suggested that haloperidol was the main drug related to the decrease in neutrophils, and in view of the greater distance in the molecular structure of haloperidol in relation to clozapine, we insisted on trying a trial with clozapine for the patient in the reported case. Another difference in our case report is the long period of follow-up, which brings more security regarding the reintroduction of a medication such as clozapine in a patient with a previous event of leukopenia, as long as this event has not been severe, and the titration of clozapine is performed in a hospital environment with more frequent blood counts, as illustrated in the present clinical case.
Conclusion
To our knowledge, the present case report is the first successful trial of clozapine after quetiapine plus haloperidol-related neutropenia, which suggests that patients who have already tried an antipsychotic that has led to blood dyscrasia, unless they have had agranulocytosis, would not be absolutely contraindicated to make a trial with clozapine.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Kodesh A, Finkel B, Lerner AG, Kretzmer G, Sigal M, et al. (2001) Dose-dependent olanzapine-associated leukopenia: three case reports. Int Clin Psychopharmacol 16(2): 117-119.
- Atkin K, Kendall F, Gould D, Freeman H, Liberman J, et al. (1996) Neutropenia and Agranulocytosis in Patients Receiving Clozapine in the UK and Ireland 169(4): 483-488.
- Zahid Latif, Faraz Jabbar, Brendan D Kelly (2011) Clozapine and blood dyscrasia. The Psychiatrist Online 35(1): 27-29.
- Li X, Cameron M D (2012) Potential role of a quetiapine metabolite in quetiapine-induced neutropenia and agranulocytosis. Chem Res Toxicol 25(5): 1004-1011.
- Shuman MD, Trigoboff E, Demler TL, Opler LA (2014) Exploring the potential effect of polypharmacy on the hematologic profiles of clozapine patients. J Psychiatr Pract 20(1): 50-58.
- Clozaril (2010) Prescribing information, Quebec. Novartis Pharmaceiticals Canada Inc.
- Nicholas M, Hannah M, Shelley X, M Large, R Bird, et al. (2019) A meta-analysis of controlled studies comparing the association between clozapine and other antipsychotic medications and the development of neutropenia. Australian & New Zealand Journal of Psychiatry 53(5): 403-412.
- Dunk L, Annan L, Andrews C (2006) Rechallenge with clozapine following leucopenia or neutropenia during previous therapy. The British Journal of Psychiatry 188(3): 255-263.
- Wu Szu-Ying, Liu Chen-Chung, Hsieh Ming H (2008) Successful re-exposure to clozapine following uneventful rechallenge with olanzapine in a patient with neutropenia related to both agents. Prog Neuropsychopharmacol Biol Psychiatry 32(4): 1089-1090.
- Shuman MD, Trigoboff E, Demler TL, Opler LA (2014) Exploring the potential effect of polypharmacy on the hematologic profiles of clozapine patients. J Psychiatr Pract 20(1): 50-58.
- Kane J, Honigfeld G, Singer J, Meltzer H (1988) Clozapine for the treatment-resistant schizophrenic. A double-blind comparison with chlorpromazine. Arch Gen Psychiatry 45(9): 789-796.
- Abdullah N, Voronovitch L, Taylor S, Lippmann S (2003) Olanzapine and haloperidol: potential for neutropenia? Psychosomatics 44(1): 83-84.
- Ruhé HG, Becker HE, Jessurun P, Marees CH, Heeringa M, et al. (2001) Agranulocytosis and granulocytopenia associated with quetiapine. Acta Psychiatr Scand 104(4): 311-313.
- Şahan E (2019) Haloperidol-related neutropenia. Indian J Psychiatry 61(3): 307-310.
- Fryer V, Billings J (2020) Low-Dose Quetiapine Causing Agranulocytosis and Leucopenia in a Patient with Benign Neutropenia: A Case Report. Cureus 12(6): e8505.
- Mattai A, Fung L, Bakalar J, Overman G, Tossell J, et al. (2009) Adjunctive use of lithium carbonate for the management of neutropenia in clozapine-treated children. Hum Psychopharmacol 24(7): 584-589.
- Almaghrebi AH (2019) Safety of a Clozapine Trial Following Quetiapine-Induced Leukopenia: A Case Report. Curr Drug Saf 14(1): 80-83.
- Esposito D, Rouillon F, Limosin F (2005) Continuing clozapine treatment despite neutropenia. Eur J Clin Pharmacol 60(11): 759-764.
- Stergiou V, Bozikas VP, Garyfallos G, Nikolaidis N, Lavrentiadis G, et al. (2005) Olanzapine-induced leucopenia and neutropenia. Prog Neuropsychopharmacol Biol Psychiatry 29(6): 992-994.
-
Emerson Arcoverde Nunes*, Lízie Emanuelle Eulálio Brasileiro. Successful Clozapine Trial After Leucopenia/Neutropenia Secondary to Haloperidol Plus Quetiapine: Ten-Year Follow-Up Case Report. Arch Phar & Pharmacol Res. 3(5): 2023. APPR.MS.ID.000572.
-
Antipsychotics, Neutropenia, Haloperidol, Schizophrenia, Quetiapine, Clozapine
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






