 Research Article
Research Article
Longevity of Endocrowns: Systematic Review and Meta-Analysis
Imen Kalghoum*, Balkiss khadhraoui, Zeineb Riahi, Mejri Oumayma, Mohamed Mouldi chebil, Chaouch Maha and Belhssan Harzallah Dalenda Hadyaoui
Department of prosthodontic, Academic dental clinic of Monastir, University of Monastir, Tunisia
Imen Kalghoum, Department of prosthodontic, Academic dental clinic of Monastir, University of Monastir, Tunisia.
Received Date:May 11, 2023; Published Date:June 05, 2023
Abstract
Introduction: The restoration of endodontically treated teeth remains a challenge. The use of post and core restorations is no longer justified.
The purpose of this systematic review is to determine whether endocrowns are a reliable option.
Materiel and Methods: Databases such as PubMed, Scopus, Web of Science, Cochrane Library were searched from 2009 up to 2022 in order to
find clinical studies that evaluated endocrowns. For the meta-analysis, survival rate of endocrowns and crowns was compared using a random effect
model and 95 % confidence intervals.
Results: 3 clinical trials fulfilled the inclusion criteria. Endocrowns showed an excellent survival rate from 86.9 % to 99%. Meta- analysis
showed no statistically significant difference between the two types of restorations.
Conclusion: Literature suggests that endocrown is a reliable option to restore damaged teeth. However, and given the lack of studies, these
results must be interpreted carefully. Further studies are necessary to confirm these findings.
Keywords:Endocrown; Crown; Survival; Success; Failure.
Introduction
On a daily basis, every dentist is required to carry out permanent fillings after root canal treatment. Those fillings should be watertight and fit ideally into the tooth morphology. However, the restoration of dilapidated teeth remains a real challenge until those days. In fact, the chosen treatments must preserve and protect the remaining dental structure while satisfactorily restoring aesthetics, shape and the function of that tooth. The popular idea that a pulp less tooth is more fragile than the vital tooth, until today, practitioners prefer to use full-coverage crowns with intra-radicular anchors for the restoration of these teeth. Still despite the considerable effect of intra-radicular anchors in reducing the failure rate of restorations of depulpated teeth, Dietschi shows that root post does not strengthen the tooth structure and may even increase the risk of fracture. Indeed, a post modifies the distribution biomechanics of the forces exerted on the tooth during its placement and during the masticatory function. This contributes to the formation of fragility along the root, explaining the increased risk of fracture root canal for teeth restored with a coronal-radicular reconstruction [34].
However, current trends have largely evolved and are moving towards less systematic and less invasive treatments. It is no longer possible to mutilate intentionally the teeth in order to adapt the tissues to a technique of restoration. It’s up to the technique to adapt to the residual tissue [13]. Indeed, thanks to increasingly efficient bonding protocols to enamel and dentin, new approaches to tooth restoration have emerged. Therefore, it becomes possible, when the conditions allow it, to eliminate intra-radicular anchoring elements thanks to bonding [18].
The endocrown seems to combine the desired qualities of the reconstruction on non-vital teeth which where tissue economy and biocompatibility, a bonded interface that absorbs stresses, and a material most often resistant to high stresses. The endocrown is therefore placed as an interesting alternative to the restoration of depulpated teeth. The endocrown is a monolithic prosthetic cap with cameral anchorage, in ceramic or composite resin, bonded to a depulped tooth. It offers a complete cusp covering and rests in the pulp chamber to meet the retention requirement, combined with the adhesion offered by bonding. This systematic review, through the available literature, seeks to establish a starting point for reconciling current views on what type of restoration. Indeed, it aims to determine the survival rate of long-term endocrowns with a minimum follow-up period of three years per compared to conventional full recovery crowns.
Materials and Methods:
This systematic review conformed to Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (Moher et al. 2009). Information Sources We searched the following databases for articles published between 2009 and 2019 that compared survival rate of endocrown and full crown: CDSR (via Cochrane Library), DARE (via Cochrane Library), CENTRAL (via Cochrane Library), CMR (via Cochrane Library), HTA (via Cochrane Library), EED (via Cochrane Library), Web of Science, Scopus, ScienceDirect, LILACS, OpenGrey et Google Scholar. References of the included articles were further checked manually.
Search Strategy
Initially, PICOS questions defined the search strategy as follows: P (population) comprised patients who has endodentically treated permanent teeth that needed prosthetic intervention; I (intervention) included endocrown and full crown; C (comparison) with full overage crown; O (outcomes and study design) was the survival rate; and S (study type) comprised cross-sectional retrospective prospective comparative studies longitudinal and cohort studies with a period of following time more than 3 years. The following MeSH terms, search terms, and their combinations were used in the MEDLINE search: (Endocrown) AND (crown) AND (2009:2019 [pdat])) AND ((survival) OR (success)) OR (failure) AND (2009:2022 [pdat])).
Study Selection and Eligibility Criteria
All titles and abstracts of the selected studies were first assessed for the following inclusion criteria: clinical studies (prospective studies, retrospective studies, or RCTs) with a follow up time up to 3years. The full text was evaluated for articles without abstracts or for abstracts with an insufficient description. After evaluating the full text of the articles according to the previously defined exclusion criteria: articles with the following features, in English or French, were considered ineligibles, articles with follow up period shorter than 3 years; case reports, literature reviews, protocols, interviews, and in vitro studies; studies conducted in isolated groups (bruxism, hypoplasia, others).
Data Collection Process
Two calibrated reviewers (I.K. and C M) collected the data from selected articles into structured tables. Disagreement for the variables collected occurred in 7% of cases. Discrepancies were resolved by consensus and a third examiner (N.S.) was consulted.
Results
Study Selection
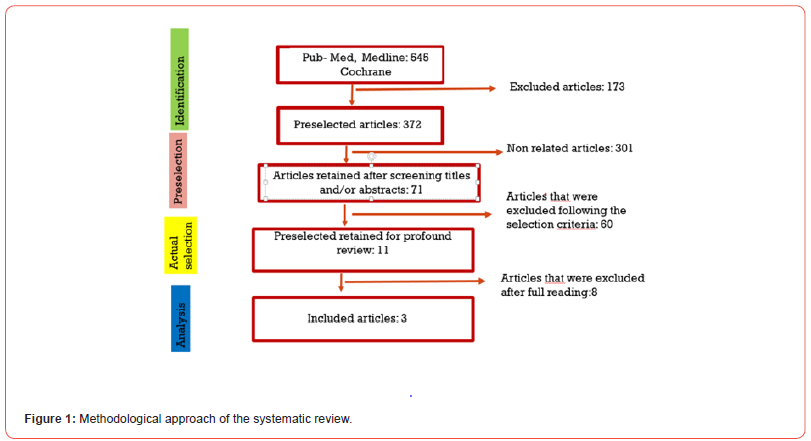
The literature search explored 13 different databases: MEDLINE (via PubMed), CDSR (via Cochrane Library) Library), DARE (via Cochrane Library), CENTRAL (via Cochrane Library) CMR (via Cochrane Library), HTA (via Cochrane Library), EED (via Cochrane Library), Web of Science, Scopus, ScienceDirect, LILACS, OpenGrey and Google Scholar. The search strategies employed yielded 545 studies [Figure 1]. After evaluating the titles and abstracts and eliminating duplicates, 371 articles were identified; 361 of these were excluded after title and abstract revision. Finally, 3 articles were included for quantitative analysis and analysis of risk of bias Study Characteristics [16,24,29].
Assessment of risk of bias [Figure 2]. Descriptive study
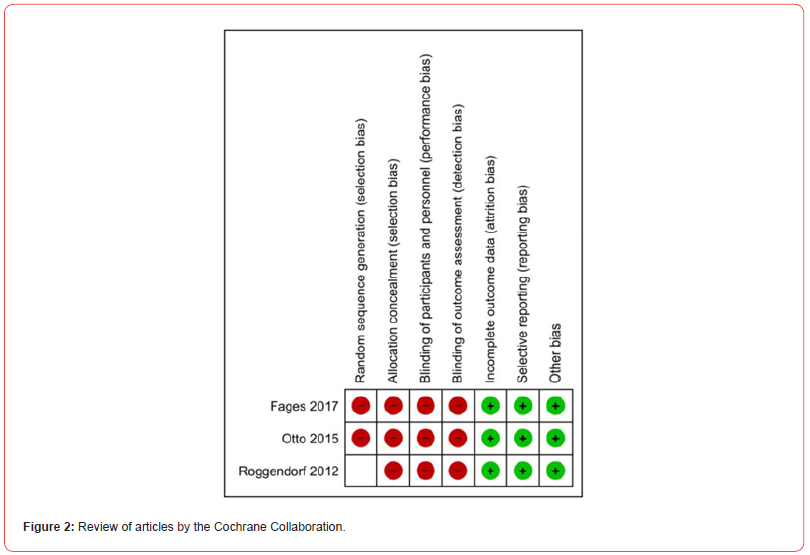
Table 1:Distribution of initial restorations.

Table 2:Distribution of failures according to each study.
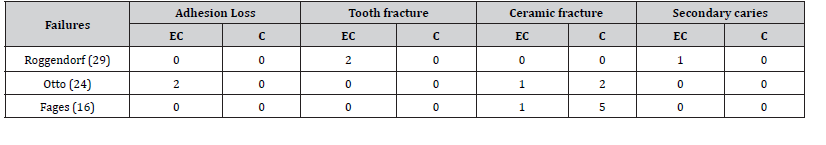
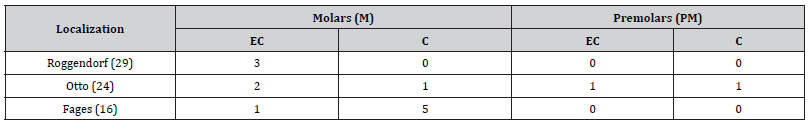
Three prospective clinical trials were included in the qualitative analysis. They were published between 2012 and 2017 [Table 1]. Summarizes the distribution of restorations for each sector. 272 endocrowns, 267 were molars and 5 premolars. Of the total 273 crowns placed, there were 7 incisors, 25 premolars and 241 molars. premolars and 241 molars. The follow-up periods ranged up to 7 years [29,16] and 10 years [24] [Table 2]. Throughout the follow-up period, patients were lost to follow-up (dropout) which explains the difference between the number of initial restorations and those examined. The modified USPHS criteria were used for the clinical evaluation of the restorations [29,24]. These include clinical verification of shade stability, surface condition, anatomical form and marginal adaptation and assign one of three one of the 3 adjectives (Alfa, Bravo or Charlie). For the marginal adaptation we add Delta to express a fracture, loss or mobility of the restoration which is considered a is considered a failure. Roggendorf [29] adds other evaluation criteria such as marginal discoloration marginal discoloration, proximal contact, proximal caries and statistical and dynamic occlusion.
He also evaluates, using a scoring system, the degree of satisfaction of the patients: 21 out of 25 patients answered very satisfied with their satisfied with their restorations, 3 satisfied and one patient was unable to express his degree of satisfaction because of his condition (dementia). In the last study, Fages [16] uses clinical criteria to evaluate the condition of the restorations such as partial fracture of the ceramic with a partial loss of the prosthesis, tooth fracture, marginal caries or endodontic complications. Out of a total of 271 endocrowns examined, 6 molars and one premolar failure resulting in secondary caries, 2 vertical fractures of supporting teeth, 2 losses of the supporting teeth, 2 bond losses and 2 ceramic fractures [Table 2]. Of the 265 crowns examined, 6 molars and one premolar failed, all resulting in of the 265 crowns examined, six molars and one premolar failed, all resulting in ceramic fracture [Table 3].
Table 3:Distribution of failures according to localization.
Meta-analysis:
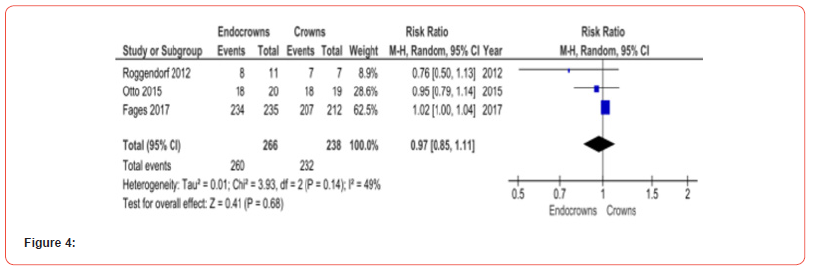
This meta-analysis was conducted for the dichotomous values which are the survivability of restorations using Revman 5.4 software The two groups of hypotheses compared are: the group restored by endocrown entitled ‘endocrowns’ vis-à-vis the group restored by classic crown entitled ‘crown’. The review that has no complications or a 100% survival rate for both groups was not included in the Forest Plot because it presents an event zero and a non-computable value of P. The selected effect mode is ‘Random’ taking into account intra- and inter-study variability and any non-standard studies are not taken into consideration during our research.
Results were considered significant if the P value calculated for the selected studies is less than 0.05, the 95% confidence interval.
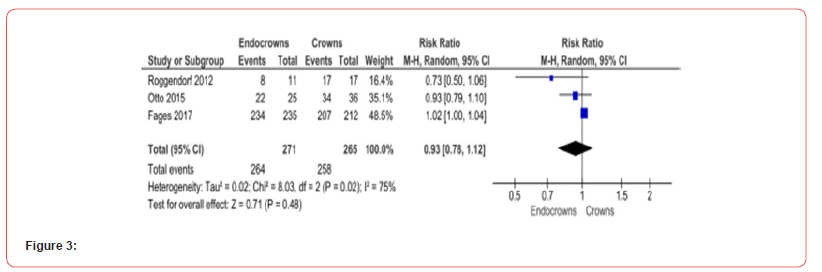
The ‘Events’ present the number of surviving restorations out of the ‘Total’ number of restorations studied in the group [Figure 3]. The Forest plot of the survival of prosthetic restorations for a long follow-up time ([7-10 years]) included 3 studies, with a total of 271 endocrown and 265 crowns. The overall effect diamond touches the no-effect line meaning there is no statistically significant difference in the survival of the 2 types of restorations (p=0.48; I2= 75%) [Figure 4]. The forest plot comparing the survival of prosthetic restorations covering the molars only also included 3 studies with a total of 266 endocrowns and 238 crowns. The overall effect diamond touches the no-effect line meaning there is no statistically significant difference in the survival of the 2 types of restorations (p=0.68; I2=49%).
Discussion
This study involved 271 endocrowns and 265 crowns, which is a relatively large number compared to other systematic reviews [1] 120 endocrowns in the systematic review by Alves de Carvalho et al [2] and 114 in that of Wittneben et al [33]. However, this result should be considered with caution since only three studies were included. An important consideration is that all of the included studies focused on posterior teeth, with only one study on molars and premolars [24]. Five premolars were restored by endocrown vs 25 premolars by classic crowns which does not allow us to compare them alone in a subgroup in the meta-analyses Although premolars are easier to restore compared to molars, thus explaining their preferable use in in vitro studies [26], the endocrowns have been shown to be more prone to failure when bonded to the premolars. Indeed, this is confirmed by the study of Bindl et al. [8], in 2005, which shows a clear difference in the longevity of the restorations compared to endocrowns between molars and premolars. The observed survival rate for molars is 87.1%, while it is only 68.8% for premolars. This can be explained by the fact that the surface available for the bonding was greater on molars compared to premolars. The relationship between the base of the crown and the height of the crown could cause a greater leverage effect for the premolars than for the molars [8].
In addition, the premolars can be subjected to horizontal forces (not axial) during function, which can cause stress to the adhesive interface and lead to more failure [6]. Endocrowns have demonstrated excellent survival rates, around 86.9% [29], 90.5% [24] and 99% [16] which are close to crowns. These very good results confirm the results of previous studies on the endocrown with present a survival rate of 82.3% for Wittneben et al. [33], 88% for Alves de Carvalho and coll. [2] and 87.1% for Bindl et al. [8]. Knowing this, these results show that endocrown restorations are a reliable approach and can replace crowns to restore the endodontically treated teeth. However, these results should be considered with caution given the small number of studies included in this review.
In this review, a total of seven endocrowns failed compared to seven crowns. The most common technical failures were loss of adhesion of the restorations (n=2) and ceramic fractures (n=2). The most encountered biological failures resulted in the fracture of the supporting tooth (n=2) and secondary caries (n=1). For crowns, ceramic fracture (n=7) is the main cause of failure. Roggendorf et al. [29] explained that these complications were not caused by the design of the endocrown, but they were mostly related to other factors (bruxism, poor hygiene) [21-23]. For Otto [24], the loss of adhesion can be explained by the stabilization insufficient through the retentive part of the pulp chamber. In that case residual wall height was 2mm. However, the depth of the cavity within the pulp chamber should be at least 3 mm [15-19]. For Fages [16], the endocrown having failed following a partial fracture of the ceramic was a wisdom [27] that is rarely restored prosthetically. This fracture occurred 3 months after bonding. For crowns, the majority of failures occurred during the first year which indicates a mechanical problem between the material used, the occlusion preparation rather than a problem of fatigue.
For the feasibility and to improve the mechanical properties, the studies have used the CAD/CAM technique for milling prostheses. Only one material has been used which is feldspathic ceramic (Vita Mark II). As a result, no comparison could be made and no conclusion could be drawn to designate the best restorative material [28,29].
Most of the in-vitro studies found in the literature have used as restorative material hybrid ceramic (Cerasmart) and glassceramic (lithium disilicate) [3-9]. The endocrowns in ceramic resin restoring the premolars had higher fracture toughness and failure rates lower than those of glass-ceramic endocrowns [30-34]. A possible explanation for this is that the modulus of elasticity of the ceramic resin is comparable to that of dentin and can thus better distribute the occlusal forces along the adhesion surface of the premolars, thus improving the resistance to fracture and reducing failure rates [35-36].
Limits of the revue
The search in this review is limited, because some search engines were not free of charge. The number of included studies was limited, especially after extrapolation of comparable data and the development of the qualitative and quantitative study (the meta-analysis). Further comparative studies and especially randomized controlled trials with a long follow-up period are follow-up period are still needed to confirm that the restoration of restoration of pulped teeth with endocrown is a feasible option. These studies must include a larger number of participants, a welldetailed clinical protocol, several types of materials and different groups of teeth.
Conclusion
We conducted a systematic review of the literature in the aim of identifying studies focusing on the longevity of endocrowns compared to conventional crowns along the length term. We have, at the end of this work, demonstrated that there is no significant difference concerning the survival rate of the two groups. However, given the small number of studies conducted, the clinical follow-up not considerable and especially the absence of randomized clinical trials dealing with this subject, caution should be exercised in interpreting these results.
Acknowledgement
None.
Conflict of Interest
No Conflict of interest.
References
- lshibri S, Elguindy J (2017) Fracture Resistance of Endodontically Treated Teeth Restored with Lithium Disilicate Crowns Retained with Fiber Posts Compared to Lithium Disilicate and Cerasmart Endocrowns: In Vitro Study Dentistry 7(12): 1-9.
- Alves de Carvalho IF, Santos Marques TM, Araújo FM, Azevedo LF, Donato H, et al. (2018) Clinical Performance of CAD/CAM Tooth-Supported Ceramic Restorations: A Systematic Review. Int J Periodontics Restorative Dent 38(4): e68-e78.
- Báez A, Durán G, de Nordenflycht D, Fuentes M (2019) Anterior composite resin crown in an adverse situation: A dental technique with a 3-year follow-up. J Prosthet Dent 121(1): 13-6.
- Bankoğlu Güngör M, Turhan Bal B, Yilmaz H, Aydin C, Karakoca Nemli S, et al. (2017) Fracture strength of CAD/CAM fabricated lithium disilicate and resin nano ceramic restorations used for endodontically treated teeth. Dent Mater J 36(2): 135-41.
- Bartala M, d’Incau E, Blanchard JP, Soenen A (2019) Prothèse fixée. In: Zunzarren R, ed. Guide Clinique D'odontologie (Troisième Édition). Paris: Elsevier Masson: 227-242.
- Belleflamme MM, Geerts SO, Louwette MM, Grenade CF, Vanheusden AJ, et al. (2017) No post-no core approach to restore severely damaged posterior teeth: An up to 10-year retrospective study of documented endocrown cases. J Dent 63: 1-7.
- Bindl A, Mörmann WH. Clinical evaluation of adhesively placed Cerec endo-crowns after 2 years-preliminary results. J Adhes Dent 1999 Autumn 1(3): 255-265.
- Bindl A, Richter B, Mormann WH (2005) Survival of ceramic computer-aided design/manufacturing crowns bonded to preparations with reduced macroretention geometry. Int J Prosthodont 18(3): 219-224.
- Carlos RB, Thomas Nainan M, Pradhan S, Roshni S, Benjamin S, et al. (2013) Restoration of endodontically treated molars using all ceramic endocrowns.Case Rep Dent: 210763.
- Conejo J, Nueesch R, Vonderheide M, Blatz MB (2017) Clinical Performance of All-Ceramic Dental Restorations. Curr Oral Health Rep 4(2): 112-123.
- Dickens N, Haider H, Lien W, Simecek J, Stahl J, et al. (2019) Longitudinal Analysis of CAD/CAM Restoration Incorporation Rates into Navy Dentistry. Mil Med 184(5-6): e365-e372.
- Dickersin K, Scherer R, Lefebvre C (1994) Identifying relevant studies for systematic reviews. BMJ 309(6964): 1286-1291.
- Dietschi D, Duc O, Krejci I, Sadan A (2008) Biomechanical consideration for the restoration of endodontically treated teeth: a systematic review of the literature, Part II (Evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int 39(2): 117-29.
- Eden J, Levit L, Berg A, Morton S (2011) Finding What Works in Health Care: Standards for Systematic Reviews. Washington : National Academies Press.
- Fages M, Bennasar B (2013) The endocrown: a different type of all-ceramic reconstruction for molars. J Can Dent Assoc 79: d140.
- Fages M, Raynal J, Tramini P, Cuisinier FJG, Durand JC, et al. (2017) Chairside computer-aided design/computer-aided manufacture all-ceramic crown and endocrown restorations: A 7-year survival rate study. Int J Prosthodont 30(6): 556-560.
- Furuse AY, Cunha LFd, Pirolo R, Runnacles P, Mondelli J, et al. (2013) Endocrown para o tratamento de dentes despolpados. Full Dent Sci 4(16): 611-614.
- Heydecke G, Butz F, Strub JR (2001) Fracture strength and survival rate of endodontically treated maxillary incisors with approximal cavities after restoration with different post and core systems: an in-vitro study. J Dent 29(6): 427-433.
- Higgins JP (2011) Cochrane handbook for systematic reviews of interventions. London: Cochrane.
- Jeong H, Kim S, Kim J, Choi N (2019) Post-endodontic restoration on erupting permanent first molars using endocrown with a polyglass composite resin: report of two cases. J Korean Acad Pediatr Dent 46(1): 111-118.
- D Moher, A Liberati, J Tetzlaff, DG Altman (2009) Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PloS Med 6(7): e1000097.
- Nandini S (2010) Indirect resin composites. J Conserv Dent 13(4): 184-94.
- Nishimori LE, Annibelli RL, Sábio S, Oliveira e Silva Cd, Progiante PS, et al. (2012) Endocrown passo a passo: do laboratório à clínica. Rev Dental Press Estét 9(4): 54-61.
- Otto T, Mörmann WH (2015) Clinical performance of chairside CAD/CAM feldspathic ceramic posterior shoulder crowns and endocrowns up to 12 years. Int J Comput Dent 18(2): 147-61.
- Pissis P (1995) Fabrication of a metal-free ceramic restoration utilizing the monobloc technique. Pract Periodontics Aesthet Dent 7(5): 83-94.
- Porto JA (2017) Influence of the restorative material and restorative protocol on the physic-mechanical performance of endocrown restorations [Thèse]. Pelotas: Faculté d’Odobtologie.
- Raman N, Manish K, Jain S (2019) Restoration of endodontically treated teeth with different crowns: A comparative study. Int J Med Biomed Stud 3(12): 237-244.
- Rocca GT, Krejci I (2013) Crown and post-free adhesive restorations for endodontically treated posterior teeth: from direct composite to endocrowns. Eur J Esthet Dent 8(2): 156-179.
- Roggendorf MJ, Kunzi B, Ebert J, Roggendorf HC, Franken Berger R, et al. (2012) Seven-year clinical performance of CEREC-2 all-ceramic CAD/CAM restorations placed within deeply destroyed teeth. Clin Oral Invest 16(5): 1413-1424.
- Rossato DM (2010) Évaluation du noyau métallique fondu, du noyau en fibre de verre et de l'endocrown céramique: analyse comparative par la méthode des éléments finis Araraquar: Faculté de Dentisterie d'Araraquara.
- Suarez-Almazor ME, Belseck E, Homik J, Dorgan M, Ramos-Remus C, et al. (2000) Identifying clinical trials in medical literature with electronic databases: MEDLINE alone is not enough. Control Clin Trials 21(5): 476-487.
- Valcanaia AJ, Garcia R, Gressler AE (2013) Reconstrução unitária posterior com coroas endocrown: relato de caso. Clín Int J Braz Dent 39(1): 6-77.
- Wittneben JG, Wright RF, Weber HP, Gallucci GO (2009) A systematic review of the clinical performance of CAD/CAM single tooth restorations. Int J Prosthodont 22(5): 466-471.
- Zhu Z, Dong XY, He S, Pan X, Tang L, et al. (2015) Effect of Post Placement on the Restoration of Endodontically Treated Teeth: A Systematic Review. Int J Prosthodont 28(5): 475-483.
- Zhu J, Rong Q, Wang X, Gao X (2017) Influence of remaining tooth structure and restorative material type on stress distribution in endodontically treated maxillary premolars: A finite element analysis. J Prosthet Dent 117(5): 646-655.
- Zou Y, Bai J, Xiang J (2018) Clinical performance of CAD/CAM-fabricated monolithic zirconia endocrowns on molars with extensive coronal loss of substance. Int J Comput Dent 21(3): 225-232.
-
Imen Kalghoum*, Balkiss khadhraoui, Zeineb Riahi, Mejri Oumayma, Mohamed Mouldi chebil, Chaouch Maha and Belhssan Harzallah Dalenda Hadyaoui. Longevity of Endocrowns: Systematic Review and Meta-Analysis. Arch Phar & Pharmacol Res. 3(4): 2023. APPR.MS.ID.000570.
-
Root canal, Tooth morphology, Endocrown, Crown, Molars and Premolars, Stabilization
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






