 Research Article
Research Article
Influence of the Covid-19 Pandemic on the Algo- Functional Status and the General Health of Osteoarthritis Patients
Yves Henrotin1,2,3*, Céline Mathy1, Françoise Alliot-Launois4, Gérard Chalès4, Laurence Seidel5, Adelin Albert5,6, R Lories7 and Laurent Grange4,8
1The Osteoarthritis Foundation, Boncelles, Belgium
2Musculoskeletal Innovative research Lab (mSKIL), University of Liège, Liège, Belgium
3Department of Physical Therapy and Rehabilitation, Vivalia, Marche-en-Famenne, Belgium
4AFLAR Association Française de Lutte Anti-Rhumatismale, Paris France
5Biostatistics, University Hospital of Liège, Liège, Belgium
6Department of Public Health, University of Liège, Liège, Belgium
7Laboratory of Tissue Homeostasis and Disease, Skeletal Biology and Engineering Research Center, KU Leuven and Division of Rheumatology, University Hospitals Leuven, Belgium
8Service de Rhumatologie CHU Grenoble Alpes hôpital sud Echirolles, France
Yves Henrotin, Musculoskeletal Innovative research Lab (mSKIL), University of Liège, Belgium.
Received Date:November 15, 2023; Published Date:November 22, 2023
Abstract
Objectives:This work reports the effects of the Covid-19 pandemic on the symptoms and the declared state of health of patients with osteoarthritis.
Design:
This is a cross-sectional study including 3465 participants and conducted online between September 2019 and January 2021. The questionnaire consisted of 230 items including socio-demographic items, diagnosis of the disease and affected joints, impact on sleep, leisure, daily activities, treatments and medications, physical activity, visual analog scale (VAS) scores for health status, pain, and discomfort, and morale, opinions about osteoarthritis and expectations.Results:
Overall, there was no significant difference in pain and function of osteoarthritis joints and in the general state of health between pre- Covid-19 and Covid-19 periods. However, a significant and relevant worsening of all VAS scores was discerned at the end of the lockdown. These may be associated with lower daily physical activity, the way participants appraised osteoarthritis impact on their family life, professional life, and hobbies, and the difficulties inflicted by osteoarthritis on fatigue and discouragement.Conclusions:
The study shows that the Covid-19 pandemic did not globally change the algo-functional status and the general state of health of patients with osteoarthritis. The first lockdown period, however notably impacted their condition for a while.Keywords:Osteoarthritis; Covid-19; Pain; Health
Introduction
The coronavirus disease 2019 (Covid-19) emerged in late 2019 in China causing millions of casualties around the world [1]. In March 2020, the World Health Organization (WHO) declared Covid-19 a pandemic; many countries imposed a lockdown and dedicated massive healthcare resources to meet medical needs, with many hospitals severely curtailing the number of elective surgeries [2]. Alongside these emergency measures, the governments did also impose social distancing measures, which strongly affected the social relations and mental health of patients, mostly patients suffering from chronic pain [3]. Osteoarthritis (OA) is the most common form of arthritis, affecting more than 500 million people globally [4,5]. OA is characterized by chronic mechanical pain and stiffness in the joint, limiting patients’ physical activities and leading them to a sedentary lifestyle and disability. OA was proposed as a risk factor for comorbidities such as metabolic syndrome, obesity, or even cardiovascular diseases and was considered a serious disease by the FDA in the United States.
The pandemic, the lockdowns, and the social distancing measures have severely impacted the lifestyle, the symptoms, and the care of OA patients. This situation caused a substantial interruption in health-care delivery, including the delay or cancelation of physician visits, prosthesis surgery, and physical therapy and rehabilitation which have been completely stopped because considered as non-essential [6]. Further, the pandemic has changed the lifestyle of OA patients and favored a sedentary lifestyle and weight gain [7]. One consequence was the appearance or the worsening of comorbidities such as diabetes or hypertension which are suspected risk factors for OA [8]. These changes were clearly demonstrated in the REUMAVID study [9]. This crosssectional study assessed the impact of the Covid-19 pandemic on patients with rheumatic and musculoskeletal diseases including OA. Throughout the first wave of the Covid-19 pandemic, patients with rheumatic diseases have experienced disruption in access to healthcare services, poor lifestyle habits, and negative effects on their overall health, well-being, and mental health. Other studies have clearly shown that lockdown had a significant impact on pain, joint function, physical function, and physical activity in patients with hip and knee OA [10].
Understanding the effect of the pandemic on people with OA might help health professionals to better address their patient needs and inform policies to protect this potentially vulnerable population. The “Association Française de Lutte Anti-Rhumatismale (AFLAR, France)” jointly with the “Osteoarthritis Foundation/ Fondation Arthrose (OAF/FA, Belgium)” launched in 2019 a vast survey entitled “Stop-Osteoarthritis” to better know the needs, beliefs, and behaviors of OA patients. The survey was conducted online between September 2019 and January 2021 (17 months) in France and Belgium. The Covid-19 pandemic offered a unique opportunity to compare the participants’ responses before and after it started on April 1, 2020. Using real-world data from this survey, we aimed to describe the effect of the Covid-19 pandemic on symptoms and health status in adults with OA, in particular during the first imposed lockdown spanning from March 15 to June 15, 2020.
Methods
Study design
The survey was designed as a cross-sectional study using an online questionnaire to gather data from persons with a selfreported clinician-provided diagnosis of OA. Participants were recruited through national OA patients’ organizations that disseminated the survey link across their channels including social media, press releases, and websites. The survey has been conducted according to the “Declaration of Helsinki” published by the World Medical Association. The survey protocol was approved by the Commission Nationale de l’Informatique et des Libertés (CNIL) and obtained the agreement number 17/03/2019-849167. All participants were requested to provide informed consent before participating in the survey.
Table 1:Main areas of the “Stop-Osteoarthritis” survey and associated items and indicators.
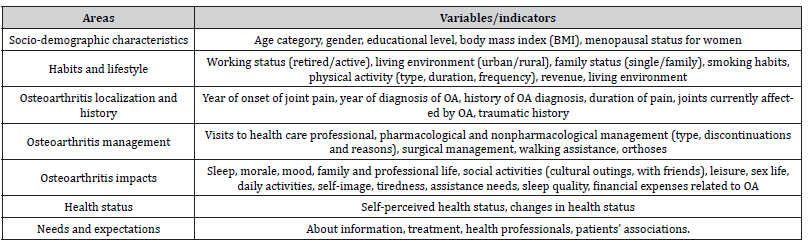
Table 2:Socio-demographic description of the participants (N=3465).
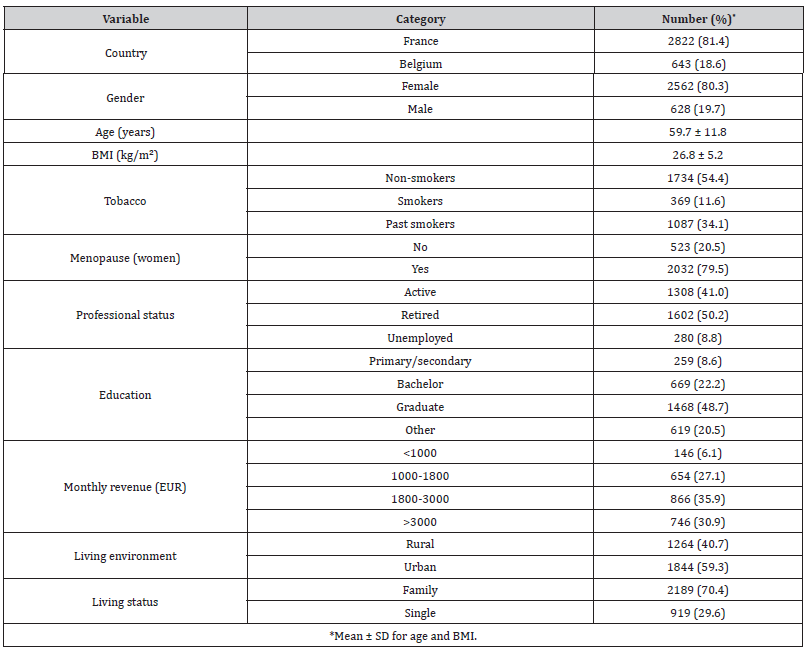
Table 3:Opinion of participants on OA (N=3465).
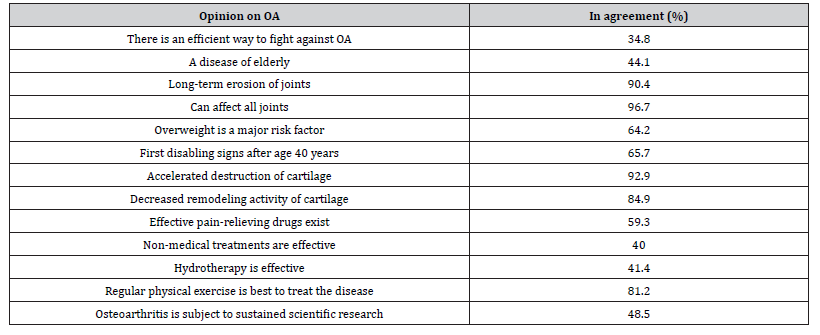
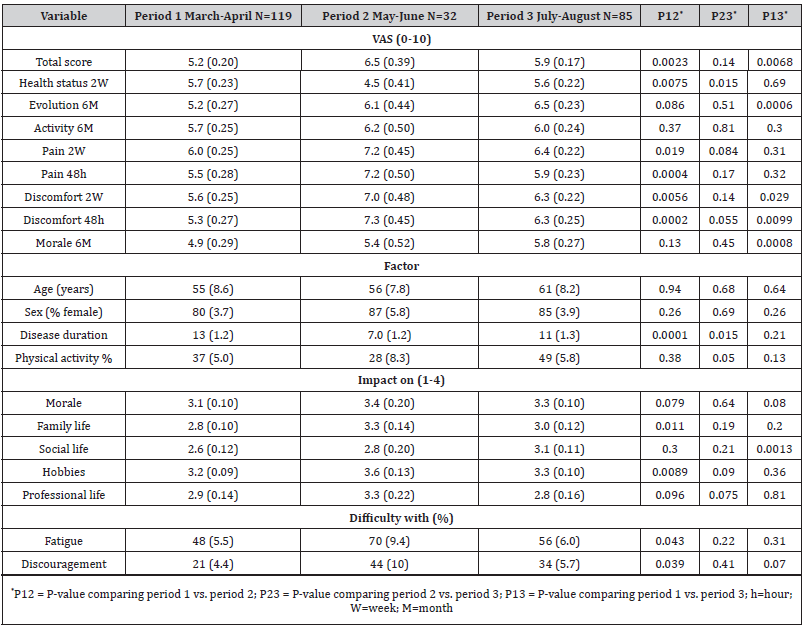
Table 4:Comparison of VAS scores and potentially influential factors around the lockdown in 2020. Data represented are means or percentages (standard errors).
Participants
Eligible participants were adults older than 18 years of age, with a self-reported clinician-provided diagnosis of OA and residing in France or Belgium. The diagnosis was ascertained through the following questions: How long have you had pain in your joint? Do you have joint pain during motion? When was OA diagnosed? Who diagnosed OA? Did you take an X-ray of your joint(s) at the time of diagnosis? Which joint (s) are affected by OA?
Questionnaire
The questionnaire written in French consisted of 230 items distributed in several domains: (a) sociodemographic characteristics, (b) habits and lifestyle, (c) OA localization and history, (d) OA management, (e) OA impacts, (f) health status, (g) needs and expectations. A summary of the main indicators of the “Stop-Osteoarthritis” survey is shown in (Table 1). Participants were asked to indicate the healthcare professional they attended during the past 12 months and were invited to share their opinion on OA, its impact on various daily life aspects and activities, the consequences of the disease, and the needs required. They were also asked about their current health status and potential comorbidities. They had to score on 10-point visual analog scales the evolution of their disease (past 6 months and past 2 weeks), the pain intensity (past 2 weeks and last 48 hours), and similarly of functional mobility and discomfort, morale, and general health status. For all assessments, high VAS scores were indicative of the poor condition, except for health status where the higher the score, the better the patient’s condition. The seven VAS scores (for health status the score was beforehand subtracted from 10) were added and averaged for each participant to provide a “global VAS score” representing the patient’s current condition and ranging from 0 = extremely good to 10 = extremely poor. Finally, participants were asked about their needs and expectations about OA treatment and the patients’ involvement in the community. Participants were volunteers and no selection was intended.
Statistical methods
Quantitative data were globally summarized by the mean and standard deviation (SD); the median and interquartile range (IQR) was added for the duration of pain and of disease. Frequency tables were used for categorical variables. Mean values were compared by the unpaired test or the non-parametric Kruskal-Wallis’s test. For proportions, the chi-squared test was utilized. In the analysis of periods during the lockdown, data were expressed as mean or percentage with standard error (SE) and were compared by an asymptotically normal Z-test. Similarly, on graphs means were associated with their standard error (SE). Results were considered significant at the 5% critical level (P<0.05). All calculations were performed with SAS (version 9.4) and R (version 4.1.0).
Results
Survey participation
During the 17-month survey period, 3465 subjects (2822 in France and 643 in Belgium) participated and filled in the questionnaire. The number of participants varied greatly over time, with two peaks, one in November 2019 (20.1% participants) and one in September 2020 (26.4% of participants). There were 1923 (55.5%) subjects who completed the questionnaire before the start of the Covid-19 pandemic and 1542 (45.5%) after it, including 116 (3.3%) during the first lockdown.
Demographics
The socio-demographic characteristics of the participants are described in (Table 2). There were 80% women and 20% men with a mean age of 59.7 ± 11.8 years and a BMI of 26.8 ± 5.2 kg/m² indicating an overweight. The proportion of smokers was 11.6%. Among women, 79.5% were menopaused. Half of the participants (50.2%) were retired and 41% declared to be still active. Over 70% had a bachelor’s or graduate education degree. The monthly revenue was higher than 3000 euros for 31% of the participants. A majority of subjects lived in an urban area (59.3%) and in a family environment (70.4%).
OA characteristics
The mean duration of pain was 16.4 ±13.2 years (median 13 years, IQR 6-21 years) and the duration of OA 12.6 ± 11.9 years (median 10 years, IQR 3-18 years). The disease was diagnosed by a general practitioner (55.3% of the cases), or a rheumatologist (36.5%) and the diagnosis was confirmed by X-ray in 87% of the cases. The affected joints were knees (left 49.1%, right 51.5%), thumbs (left 29.9%, right 32.7%), other fingers of the hand (left 22.9%, right 26.9%), hips (left 22.9%, right 26.0%), and feet (left 19.2%, right 20.9%). Over the past 12 months, patients visited mostly their GP (83%), physical therapist (51.2%), rheumatologist (48.1%), and radiologist (40.8%). OA-related pain varied with weather conditions (68.2%) and impacted sleep and night wakeups (51.2%). Almost half (49.3%) of the patients took medicines on a regular basis to relieve pain. Of note, 35.8% of participants reported complementary or alternative medicine therapies. Among patients, 38.6% had a daily physical activity, 24.6% a weekly physical activity, and 12.4% didn’t have any.
Opinion on OA
During the past 5 years, 62.7% of the participants changed their diet to lose weight. As described in (Table 3), more than a third (34.8%) believed that a cure exists against OA, 44.1% thought OA is a disease affecting the elderly, and 90.4% OA is related to an erosion of the joints. Among other opinions, OA impacts morale (80.8%), hobbies (78.1%), family life (61.9%), social activity (58.0%), professional life (43.7%), and sexual life (32.2%). Considering the undesirable consequences of OA, participants insisted on pain (87.8%), fatigue (47.9%), lack of hobbies (45.1%), uncertainty about disease evolution (44.2%), traveling difficulties (36.6%), daily household activities (34.2%), inefficiency of treatments (25.8%), despair (24.8%), physical deformation (22.4%), psychological impact (21.2%) and professional activities (18.8%).
Assessment of health condition
Health status over the last 2 weeks assessed on a VAS (0 = worst, 10 = best) averaged 5.8 ± 1.9, just above the middle of the scale. Among patients, 61.7% mentioned concomitant morbidity like cardiovascular disorders (39.9%), trauma (39.7%), anxiety (33.6%), depression (15.1%) and diabetes (8.7%). The assessment of the evolution of OA over the past 6 months on a VAS (0 =no evolution, 10=strong evolution) led to a mean score 5.4 ± 2.5 while the score for last 6-month disease activity was 5.5 ± 2.2 on a VAS ranging from 0=not active to 10 = extremely active. Pain scores averaged 5.8 ± 2.2 over the last 2 weeks and 5.5 ± 2.4 over the last 48 h on a VAS (0 = no pain, 10 = extreme pain). The pain varied with time for 63.7% of the patients and with physical activity for 48.4% of them. Functional discomfort due to OA assessed on a VAS (0=none to 10=extreme discomfort) was 5.7 ± 2.3 for the last 2 weeks and 5.5 ± 2.4 for the past 48h. The mean morale score was 4.9 ± 2.5 on a similar scale.
The overall impact of the pandemic
The pre-Covid-19 period (N=1943, September 2019 –March 2020) was compared to the Covid-19 period (N=1542, April 2020 – January 2021). There were more female participants during Covid-19 than before (82.6% vs. 78.4%, P=0.0032) and participants were older (61.0 ± 12 years vs. 58.7 ± 12 years, P<0.0001). There were also significantly more participants retired during the crisis (55.2% vs. 44.2%, P<0.0001). Daily physical activity only tended to be higher during the pandemic than before (41.2% vs. 36.4%, P=0.066), in particular inside cycling (18.8% vs. 15.9%, P=0.056). The characteristics of OA patients were generally comparable during the two periods and so were the opinions about the disease. More people fully agreed that OA was due to wearing of joints and related to overweight during the pandemic than before (respectively 55.0 vs. 46.2% and 24.7 vs. 19.2%, P<0.0001). As for the VAS scores, they were on average similar during the two periods. Thus, despite the Covid-19 pandemic, not much of a difference was seen between survey participants’ data in pre-Covid and Covid periods.
Effect of the lockdown
When focusing on the lockdown (15 March – 15 June 2020), a clear deterioration in almost all VAS scores was observed in May- June (end of lockdown) as compared to March-April (beginning of the lockdown) with values often returning to previous levels in July-August (immediate post-lockdown period) (Table 4). This is best visualized in (Figure 1) where the global VAS score is graphed over time. As of May, a marked increase (worsening) of the patient condition occurred which waned only after July and returned to pre- Covid levels in September 2020. When comparing the mean score ± SE of March-April with that of May-June, a significant increase was observed (6.5 ± 0.39 vs. 5.2 ± 0.20, P=0.0023). The July-August mean score (5.9 ± 0.17) slightly decreased compared to the May- June score (P=0.14) but remained significantly higher than the March-April score (P=0.0068). (Table 4) shows that the mean score was worse at the end of the lockdown (May-June 2020) for health status, pain 2 weeks and 48h, and discomfort 2 weeks and 48h. As for the last 6 months’ assessments of disease evolution, disease activity, and morale, the deterioration observed was not significant. Of note though, 6 months assessments of disease evolution and morale in July-August were far worse than those in March-April. By contrast, no change was observed for VAS disease activity assessed by participants, not only during lockdown but also over the entire survey period (September 2019 – January 2021) (data not shown).
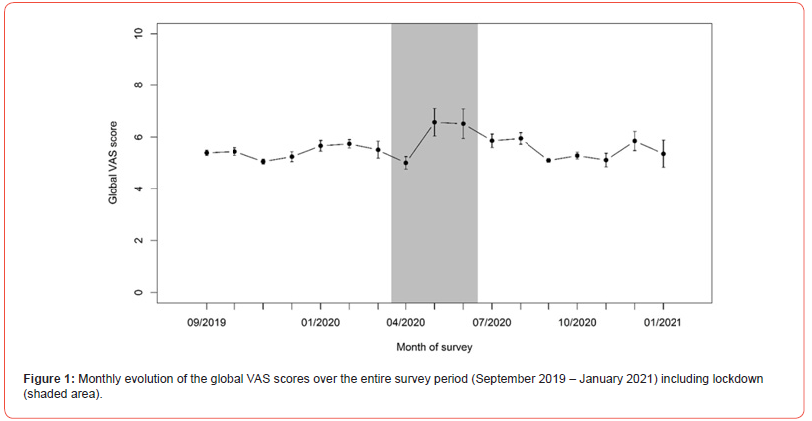
In order to discern potential factors and covariates potentially associated with the observed deterioration of the patients’ condition at the end of the lockdown period, comparisons were made of participants’ characteristics and responses between the March-April, May-June, and July-August periods. As seen in (Table 4), during the lockdown, the age and sex ratio of participants (predominantly women) remained unchanged. Similarly, no trend was found in BMI of the participants, in the proportions of retired, of people living in urban areas, and of those living in the family (data not shown). By contrast, the disease duration of the participants was significantly lower in the May-June period (P=0.0001). There was also a notable drop-in daily physical activity between the end and beginning of the lockdown (28% compared to 37% and 49%). When looking at how OA impacted patient’s condition (on a 1-4 scale), participants invoked more family life (P=0.011) and hobbies (P=0.0089), and to lesser extent morale (P=0.079) and professional life ((P=0.096) at the end than at the beginning of the lockdown. Social life was affected but much later in July-August. Finally, the percentages of participants reporting OA-related difficulties with fatigue and discouragement were significantly higher at the end of the lockdown (May-June) than before (P=0.043 and P=0.039, respectively).
Discussion
In this study, no significant difference in pain and function of OA joint and in the general state of health between pre-Covid-19 and Covid-19 periods has been reported, except during the lockdown (March-June 2020). Subjects recruited during this period reported higher scores for pain, joint discomfort, worse general health, and lower morale. These data are in line with those of Endstrasser et al. [10] demonstrating that the Covid-19 lockdown significantly affected the level of physical activity, joint and physical function in patients with advanced hip and knee OA. In contrast, these authors did not observe any change in mental health during the lockdown whereas in our study the participants showed lower morale later after the lockdown. This difference between the two studies can be explained on the one hand by the characteristics of the OA subjects questioned and on the other hand by the method of data collection. Endstrasser et al. telephoned patients whose knee or hip replacement has been postponed due to Covid-19, while we interviewed a heterogeneous population of OA patients in terms of severity, location, or management of the disease. Another major difference was the higher ratio of women (80%) in our study compared to the Endstrasser et al study (44%). Another study designed to address the consequences of the Covid-19 pandemic on patients with rheumatic diseases including OA, reported a higher prevalence of anxiety and depression cases during the lockdown than those reported in pre-pandemic studies [9]. Furthermore, patients also reported increased smoking and alcohol consumption, weight gain, and decreased physical activity, alongside the inability to continue with rehabilitation exercises or physiotherapy sessions. A recent Chinese study showed that social isolation during the Covid-19 lockdown significantly affected the psychological and physical health of the population in the Hubei province [11]. This was explained by the fact that the continuous decrease of physical activity is associated with an increase in pain and loss of joint function. In order to identify potential factors and covariates associated with the observed deterioration of patients’ condition at the end of the lockdown period, comparisons were made of participants’ characteristics and responses between the beginning, the end, and the immediate post-lockdown periods. Physical activity could be one explaining factor. Indeed, physical activity decreased in the second part of the lockdown. This observation could contribute to explaining the deterioration of health status during the lockdown. Inversely, we can also hypothesize that health status deterioration during the second half of the lockdown was not the consequence but the cause of decreased physical activity. Other explaining factors could be those that impacted OA patients’ condition. The participants invoked more family life and hobbies at the end than at the beginning of the lockdown. Finally, fatigue could contribute to patient deterioration during the lockdown since it was reported by participants that fatigue and discouragement were significantly higher at the end of the lockdown than before. The effect of physical isolation on mental health also cannot be overlooked. Loneliness is particularly affecting those living alone and without children, and is strongly associated with depression, generalized anxiety and poor health behavior [12]. These findings contribute to explaining the increased disease activity and decreased morale observed in our study during the lockdown. One may also suspect that during the lockdown OA patients have stopped their treatments because they had less contact with their physician and/or physical therapist or to avoid exposing patients to additional risks.
An important and original finding of our study is that the observed deteriorations seem to be reversible. Indeed, after the lockdown all the affected variables returned to a level equivalent to the pre-pandemic period. This indicates that the changes observed in OA disease activity were related to the particular lockdown condition and not related to the pandemic situation by itself. This again underlines the importance of patient’s lifestyle on the symptoms of OA. Some studies have reported that lockdown was associated with a decrease of physical activity and increased weight, two conditions that may enhance symptoms in OA patients. Further, NSAIDs which are used as the first line option for managing OA symptoms, have been accused of increasing the Covid-19 pleuropulmonary complications [13]. This has led physicians to be cautious about their use in the treatment of chronic pain such as OA. The decrease of NSAIDs consumption mainly during the lockdown could explain the worsening of OA symptoms [14].
The results of the present survey should be interpreted in the context of several limitations. Firstly, as any survey based on a voluntary basis, it is prone to bias and population selection. Secondly, it was limited to two European countries and therefore did not reflect the worldwide situation. Thirdly, this study was not initially designed to investigate the Covid-19 on the OA disease symptoms and management. Fourthly, some questions about the impact of Covid-19 on the health status, social conditions or OA management were missing which is a limiting factor for the interpretation of the data. Finally, the number of participants during the lockdown was somewhat limited and probably not enough representative of the global population during this particular period.
Conclusion
This survey conducted over 17 months and involving 3465 participants was unfortunately hit by the Covid-19 pandemic emerging in 2020. When comparing the pre-Covid period with the 2020 Covid period which started effectively at the end of March 2020, no major differences were highlighted. Patient characteristics, not only socio-demographic but also clinical, remained roughly the same, and similarly for participants’ opinions and behaviors. However, a closer look at months encompassing the first wave of the pandemic and lockdown (March-August 2020) revealed some striking changes in patients’ assessment scores of health status, disease evolution, and activity, pain, discomfort, and mood, in particular when the assessment was asked over a short time period (last 48h or 2 weeks).
Acknowledgments
The authors thank Tilman SA, Pfizer and Laboratoires Expanscience, LABHRA and Genevrier for partly funding this survey.
Ethical statement
The survey protocol was approved by the Commission Nationale de l’Informatique et des Libertés (CNIL) and obtained the agreement number 17/03/2019-849167. All participants were requested to provide informed consent before participating in the survey.
Authors Contributions
YH, CM, FA and LG wrote the protocol and the questionnaires. YH drafted the manuscript and CM, RL, LG, AA reviewed it. AA and LS performed the statistical analysis.
Data availability statement
All data and statistical reports are available and can be requested to Yves Henrotin.
Additional information
The authors have no conflict of interest to declare in relation to the subject of the paper. The funding source did not have any influence on study design, collection, analysis, and interpretation of data, in the writing of the manuscript and in the decision to submit the manuscript for publication.
Conflict of Interest
No conflict of interest.
References
- Hasell J, Mathieu E, Beltekian D, Macdonald B, Giattino C, et al. (2020) A cross-country database of COVID-19 testing. Sci Data 7(1): 345.
- Huang C, Wang Y, Li X, Ren L, Zhao J, et al. (2020) Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395(10223): 497-506.
- Stein RA (2020) COVID-19 and rationally layered social distancing. Int J Clin Pract 74(7): e13501.
- Mobasheri A, Fonseca JE, Gualillo O, Henrotin Y, Largo R, et al. (2021) Editorial: Inflammation and Biomarkers in Osteoarthritis. Front Med (Lausanne) 8: 727700.
- Hunter DJ, March L, Chew M (2020) Osteoarthritis in 2020 and beyond: a Lancet Commission. Lancet 396(10264): 1711-1712.
- Dell'Isola A, Kiadaliri A, Turkiewicz A, Hughes V, Magnusson K, et al. (2021) The impact of first and second wave of COVID-19 on knee and hip surgeries in Sweden. J Exp Orthop 8(1): 60.
- Larghi MM, Grassi M, Luca F, Placenza E, Rampulla C, et al. (2020) Clinical outcome before and after COVID-19 quarantine in patients’ effect of knee and hip osteoarthritis. Acta Biomed 91(4): e2020150.
- Ragni E, Mangiavini L, Viganò M, Brini AT, Peretti GM, et al. (2020) Management of Osteoarthritis During the COVID-19 Pandemic. Clin Pharmacol Ther 108(4): 719-729.
- Garrido-Cumbrera M, Marzo-Ortega H, Christen L, Plazuelo-Ramos P, Webb D, et al. (2021) Assessment of impact of the COVID-19 pandemic from the perspective of patients with rheumatic and musculoskeletal diseases in Europe: results from the REUMAVID study (phase 1). RMD Open (1): e001546.
- Endstrasser F, Braito M, Linser M, Spicher A, Wagner M, et al. (2020) The negative impact of the COVID-19 lockdown on pain and physical function in patients with end-stage hip or knee osteoarthritis. Knee Surg Sports Traumatol Arthrosc 28(8): 2435-2443.
- Ahmed MZ, Ahmed O, Aibao Z, Hanbin S, Siyu L, et al. (2020) Epidemic of COVID-19 in China and associated Psychological Problems. Asian J Psychiatr 51: 102092.
- Beutel ME, Klein EM, Brähler E, Reiner I, Jünger C, et al. (2017) Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry 17(1): 97.
- Wong AY, MacKenna B, Morton CE, Schultze A, Walker AJ, et al. (2021) Use of non-steroidal anti-inflammatory drugs and risk of death from COVID-19: an OpenSAFELY cohort analysis based on two cohorts. Ann Rheum Dis 80(7): 943-951.
- Robb CT, Goepp M, Rossi AG, Yao C (2020) Non-steroidal anti-inflammatory drugs, prostaglandins, and COVID-19. Br J Pharmacol 177(21): 4899-4920.
-
Yves Henrotin*, Céline Mathy, Françoise Alliot-Launois, Gérard Chalès, Laurence Seidel, Adelin Albert, R Lories and Laurent Grange. Influence of the Covid-19 Pandemic on the Algo-Functional Status and the General Health of Osteoarthritis Patients. Arch Phar & Pharmacol Res. 3(5): 2023. APPR.MS.ID.000573.
-
Osteoarthritis, Covid-19, Health Status, Pain, Cardiovascular Diseases, Physical Therapist, Rheumatologist
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






