 Research Article
Research Article
Evaluation Of Medicine Use Pattern and Practices Among Pharmacy and Medicine Students of a Nigerian Federal University
Ogbonna Brian O1,2*, Achuagu Vera O1, Eze Uchenna IH5, Onwuchuluba Ebele E4, Omuta Michael C3, Egere Eustace C3, Osuafor Nkeiruka G3, Okengwu Ogadinma7, Ofor Amala C7, Nwafor Maureen N7, Oluigbo Kennedy E7, Ohiaeri Ifeyinwa G1, Nwafor Maureen N7, Onwumah Malachy3, Ogujiuba Chika U2, Ejie Izuchukwu L1,Umeh Ifeoma B1, Adenola Ugochi1, Anetoh Maureen U1, Achi James C1, Ezenekwe Njideka L1, Ofomata Chijioke P1, Maduka Anthony3, Nnamani Monica3, Okoye Ijeoma M1, Okpalanma Nneoma N6, Maduekwe Hilda N6, Okoye Ifunanya6, Okeke Anthony6, Offu Ogochukwu F7, Ajagu Nnenna7 and Ejim Chuka E7
1Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Nigeria
2Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, King David University of Medical Sciences, Nigeria
3Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmaceutical Sciences, Madonna University, Nigeria
4Department of Clinical Pharmacy and Bio-Pharmacy, Faculty of Pharmacy, College of Medicine University of Lagos, Nigeriaa
5Department of Clinical Pharmacy and Bio pharmacy, Faculty of Pharmacy, Olabisi Onabanjo University, Nigeria
6Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Chukwuemeka Odimegwu Ojukwu University, Nigeria
7Department of Clinical Pharmacy and Bio-Pharmacy, Faculty of Pharmaceutical Sciences, Enugu State University of Sience and Technology, Nigeria
Ogbonna Brian O, Department of Clinical Pharmacy and Pharmacy Management, Faculty of Pharmaceutical Sciences, Nnamdi Azikiwe University, Awka and Department of Clinical Pharmacy and Pharmacy Practice, Faculty of Pharmacy, King David University of Medical Sciences, Uburu, Nigeria.
Received Date:October 17, 2022; Published Date:Novemeber 25, 2022
Abstract
Inappropriate handling of medicines is a limitation that encourages irrational and careless use of medicine. We evaluated the medicine use pattern and practices among pharmacy and medical students in the university. The study was a prospective cross-sectional survey. The study took place between September 2021 and October 2022. All the students who gave their informed consent were sampled using the questionnaire. We used students t-test to compute differences in two means, and Chi square for differences in proportion. All interviews were transcribed verbatim by a research assistant into written transcripts. A p-value of p<0.05 was considered significant. The total sample size was 205 (100%). The following describes majority of the study population; male (54.63%), 21-25 years (60.98%), pharmacy (53.17%), Christians (98.05%), Igbos (97.07%). majority of the students (60.98 %) who participated in the survey fell within the age 21-25 years and a little percentage of them (7.32 %) were between 30-35 years old. Majority of the students were males (112, 54.63 %) and females (98, 45.37 %). The prevalence of self-medication among the pharmacy students was 87.80 % and 12.20 % for medical students. Most of the medical students and one -fifth of the pharmacy students considered the quality of health care service and facilities before visit, p=0.000. the students had good knowledge of self-medication. The prevalence of self-medication was high among the pharmacy students but low among their medicine counterparts. Long physicians waiting time was a major limiting factor reported by the students. The predictors friends and family recommendations.
Keywords:Self-medication; Rational drug use; Medicine utilization; Drug misuse; Nigeria
Introduction
Medicines are substances used to combat disease process which can lead to harmful outcomes when used inappropriately. Depending on a patient’s patho-physiologic factors and pharmacologic characteristics of the medicine; this event can be as dangerous and devastating as death [1]. In most developing countries, drug monitoring system is very poor and there is easy access to drugs with or without a prescription [2]. Rational use of medicine is defined by the World Health Organization as a situation where,” patients receive medications appropriate to their clinical needs, in doses that meet their own individual requirements, for an adequate period of time, and at affordable prices” [2]. More than 50% of all medicines prescribed, dispensed, or sold around the globe are seen to be somehow inappropriate and at the same time, 50% of patients fail to take these medicines appropriately [2]. Irrational use of medicines can occur in different form but self-medication and recommendation of drug by chemists and quacks are seen as the most frequent forms. Besides, in a number of countries, the quality of drugs and inappropriate use of antibiotics is a growing concern. When analyzed from a public health viewpoint, this situation needs special attention because owing to these malpractices, mass population has become more vulnerable due to excess healthcare cost, adverse drug reaction and allergic reactions seen, toxic poisoning, exacerbation, or perilous treatment. Antibiotic resistance increases the cost of treatment, and the poor people often have to choose between going without treatment and spending so much money on drugs.
The most prevalent form of irrational drug use known to be self-medication which is one aspect of self-care, involves the selection and use of medicines by people to treat self-recognized illness [3]. Self-medication is common in the world today especially among the young ones and there are so many reasons which could be attributed to it. Some of them are ignorance, the urge of selfcare, lack of health services, feeling of sympathy toward family members in sickness, extensive advertisement, financial constraint, misbelieves, lack of time and availability of drugs in other than drug shops are responsible for growing trend of self-medication especially the patent medicine shops [4]. In developing countries, both orthodox and non-orthodox medicines are commonly seen in self-medication cases. Medicines for self-medication are generally referred to as Non-prescription or over the counter (OTC) and they are available without a doctor’s recommendation through pharmacies or patent medicine stores. In some countries, OTC products are also available in supermarkets and other outlets like public transport, open market and so on. Medicines that require a doctor’s prescription are called prescription only medicine (POM) [5]. Self-medication with OTC medicines is somewhat viewed as responsible self-medication, this is to differentiate it from the practice of self-purchasing and use of a prescription medicine without prescription by the doctors. Self-medication is common around the globe. The prevalence of self-medication from studies carried out in Europe is 68%, while it is higher in African countries (40.7-81.8%). Nigeria showed a prevalence of self-medication of 85% [4].
The OTC drugs that can be easily accessed by the public without a prescription from the physicians are seen to be relatively safe with less regulation when the assurance of rationale used is endured. These OTC are grouped according to the WHO Anatomical Therapeutic Chemical (ATC) as analgesics, antacids, laxatives, antihistamines, antithrombotic agents, cold and cough preparations, antihistamines, throat, and throat preparations, dermatological, and antidiarrheals [6]. At the community level, the practice of the rationale use of drugs provides some benefits such as saving scarce resources from being used on minor illness, controlling chronic diseases to prevent frequent hospital visitation, and reducing absenteeism from work because of negligible illness. However, irrational medicine use of OTC can have serious health hazards especially deaths in worst case scenarios and could occur mostly in extremes of ages (geriatrics and pediatrics), lactating and pregnant mothers, and patients with co-morbidities.
Improper medicine use pattern and practice among students pose a progressive threat to the health sector globally as selfmedication could lead to variety of health problems ranging from under treatment, increased cost of resulting sickness, wrong doses of drugs, addiction in the case of habit-forming medications and complications that can lead to death. In under-developed and developing countries, most episodes of illness are treated by selfmedication especially in rural areas and among health sciences students who feel they already gathered enough knowledge to treat themselves. In some under-developed and developing countries including Nigeria, medicines are dispensed over the counter (OTC) with little or no supervision. Here, self-medication seems to provide a lower cost of treatment for people who cannot afford the medical professional’s services. Irrational use of medicine and abuse could lead to inaccurate diagnosis and medication therapy, and it could also cause side-effects, drug interaction, toxicity, and unnecessary expenditure [7].
Medicines are commonly used in universities by students; hence a rational use of these medications should help combat the problems faced from their improper use, leading to an improvement in the health outcome. These can be achieved through adequate information from the health care personnel to suit the clinical needs of the students. A research work reported in 2010 in Ahmadu Bello university campus, Zaria, showed that students of healthrelated facilities practiced self-medication more than students of non-health related facilities and no data is available on the current status of the medicine use pattern and practices among pharmacy and medicine students hence the need for this research geared towards adding to existing data worldwide. Pharmacists and physicians play key roles in providing helpful recommendations on proper and safe use of pharmaceutical products. Therefore, the purpose of this study was to investigate knowledge, attitude, and practice toward self-medication in pharmacy and medical students. We evaluated the medicine use pattern and practices among pharmacy and medical students in the university.
Methods
Study area and setting
The study was conducted in Nnamdi Azikiwe University; Nnewi and Agulu campuses for medical and pharmacy students respectively. Nnamdi Azikiwe University is a federal university located in the Southeastern part of Nigeria; Anambra state to be precise. The university has many campuses (Awka, Nnewi, Agulu, Mbaukwu and Ifite-ogwali); of which the faculties of Medicine and Pharmaceutical sciences are located in Nnewi and Agulu respectively.
Study design
The study was conducted among different class of the students in the university where to collate a reasonable response. Subjects who reported using medicines at the time of the study or in the previous month were invited to participate in this study. Only students in these departments were eligible for this study. A convenience sampling method was used to select the participants from different backgrounds including the variety of age group, gender, and education level and health status to get more details and experiences with medicines use. The required sample was determined by reaching the saturation point when no more new ideas can be obtained.
Study population
The study population involved Medicine and Pharmacy students from different levels of the two faculties schooling in Nnamdi Azikiwe University, Anambra state who were willing to participate.
Description survey tool
The survey tool is divided into three sections in the questionnaire. Each section aiming to collect specific data for this study following the study objectives and Study criteria.
Inclusion criteria
All pharmacy and medicine students from second year to final year in 2020/2021 academic session.
All pharmacy and medicine students from second year to final year who were available and willing to participate in the study.
Exclusion criteria
All pharmacy and medicine students from second year to final year who were not willing to participate in the study.
All pharmacy and medicine students not available/present at the point of study
Sample size calculation
The sample size for the study was determined using the Yamane’s formula n = N/[1+N(e)2]
Where n = population size (this will depend on the number of pharmacy and medical students in the university)
Assuming that the population of pharmacy students is 630, the
sample size of the students will be calculated as shown below.
e = acceptable margin of error
From our data,
N = 630
e = 0.05
n = 630/1 + 630(0.05)2
n = 630/1 + 1.575
n = 630/2.575
n = 245
Using an estimated attrition rate of 5%,
5% of 245 = 12.25
12.25 + 245 = 257
Hence the number will be adjusted to two hundred and fiftyseven (257) to accommodate incorrectly filled questionnaires and compensate for attrition.
For medicine students, Yamane’s formula will be used as well and a population of 690; attrition rate of 5%, their number will be adjusted to two hundred and sixty-six (266).
Data collection
Data was collected from sample population using questionnaires which were retrieved, and data were analyzed using appropriate statistical method. From the data collected, the medicine use, pattern and practice among medicine and pharmacy students were assessed.
Pilot testing
The study was pretested for content, design, readability and comprehension amongst ten (10) students from the faculties of Medicine and Pharmacy respectively in Nnamdi Azikiwe University; and modifications were made accordingly. This was to validate the questionnaire before use. The questionnaire was then adjusted from the response obtained. Nevertheless, those who partook in the pilot testing study were excluded in the main study.
Sampling method
The questionnaire was adopted from previous studies at Bangladesh and Ethiopia. The students assessed were stratified by their course of study (pharmacy and medicine). The questionnaires were printed and shared at both faculties to obtain the response from the students. The population of the students (2nd year to final year) of faculty of pharmaceutical science and medicine as at 2020/2021 are approximately 630 and 690 respectively. Thus, given a total population of 1320 students with a sample size of 257 and 266. All pharmacy and medicine students who gave their consent were surveyed in the study using clustered sampling method.
Data analysis
Data collated was analyzed using statistical package for social sciences (IBM-SPSS) and descriptive statistics to run frequencies and proportion. We used studnts t-test to compute differences in two means, and Chi square for differences in proportion. All interviews were transcribed verbatim by a research assistant into written transcripts.
Ethical consideration
Before the commencement of this study, ethical approval for the study protocol was obtained from the Research and Ethics Committee of Nnamdi Azikiwe University Teaching Hospital (NAUTH).
Result
Overall, 12.20 % of the pharmacy students consult their physician while 73.17% of the medical students see their Physician. 60.49% of the medical students considers quality facility as regard their treatment when they are ill. Only 21% of the pharmacy student that do consider good health care facility as far their health is concerned. 14.63% of Pharmacy student consults a physician when sick, were as 55.61% of medical student do same, when they fall ill. About 22.93% of the pharmacy department do follow their prescribed drugs always unlike the medical department were 65.37% involved in this. 82.93% of the medical student said they provide details of their health status when asked by a physician and 35% of the pharmacy also do same when necessary. From the respondent 26.34% of the pharmacy department give details of previous treatment while 73.66% of the medical students do so when in a visit to a physician. 97% of medical student in this study consider the choice of medication based on previous use against 5.85% of pharmacy student. 58.54% of the medical student always discuss any underlying illness that might affect the medication they take while only 3.41% of pharmacy students does the same. 3.41% of pharmacy student against 48.29% of medication student go for checkups. 57.56% of the medical students says they go for second option only when necessary, so do 1.46% of the pharmacy student. 50.0% of the medical students go a second option only when their health is complicated from medications taken, this is also the case of 4.39% of pharmacy students. In conclusion 94.15% of the pharmacy believes in self-medication and they recommend it too. And it was discovered that 87.80% of the pharmacy student practice self-medication while 22.20 % of the medical student do too
Table 1:The Demographic variables of respondents.
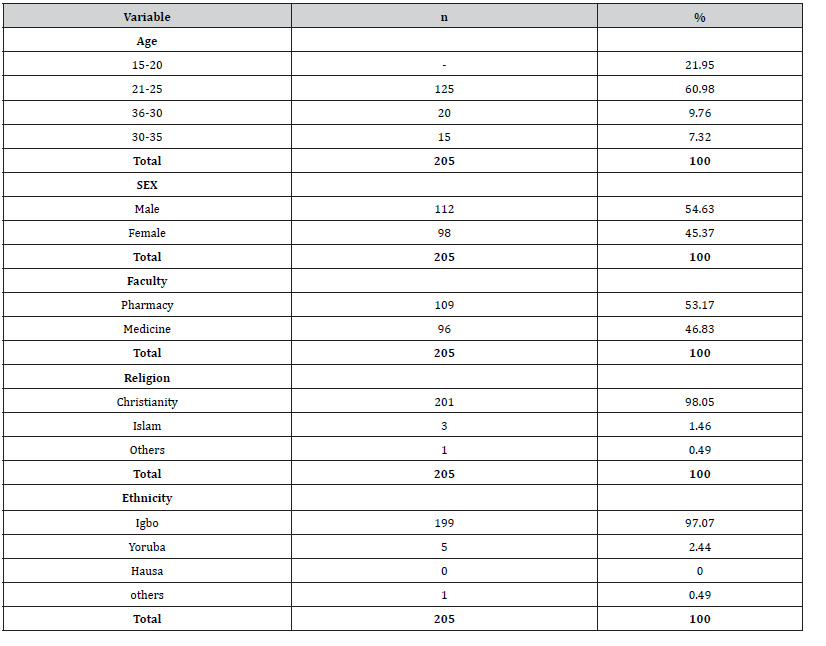
Table 2:The prevalence, pattern and practice of medicine use among the students under study.
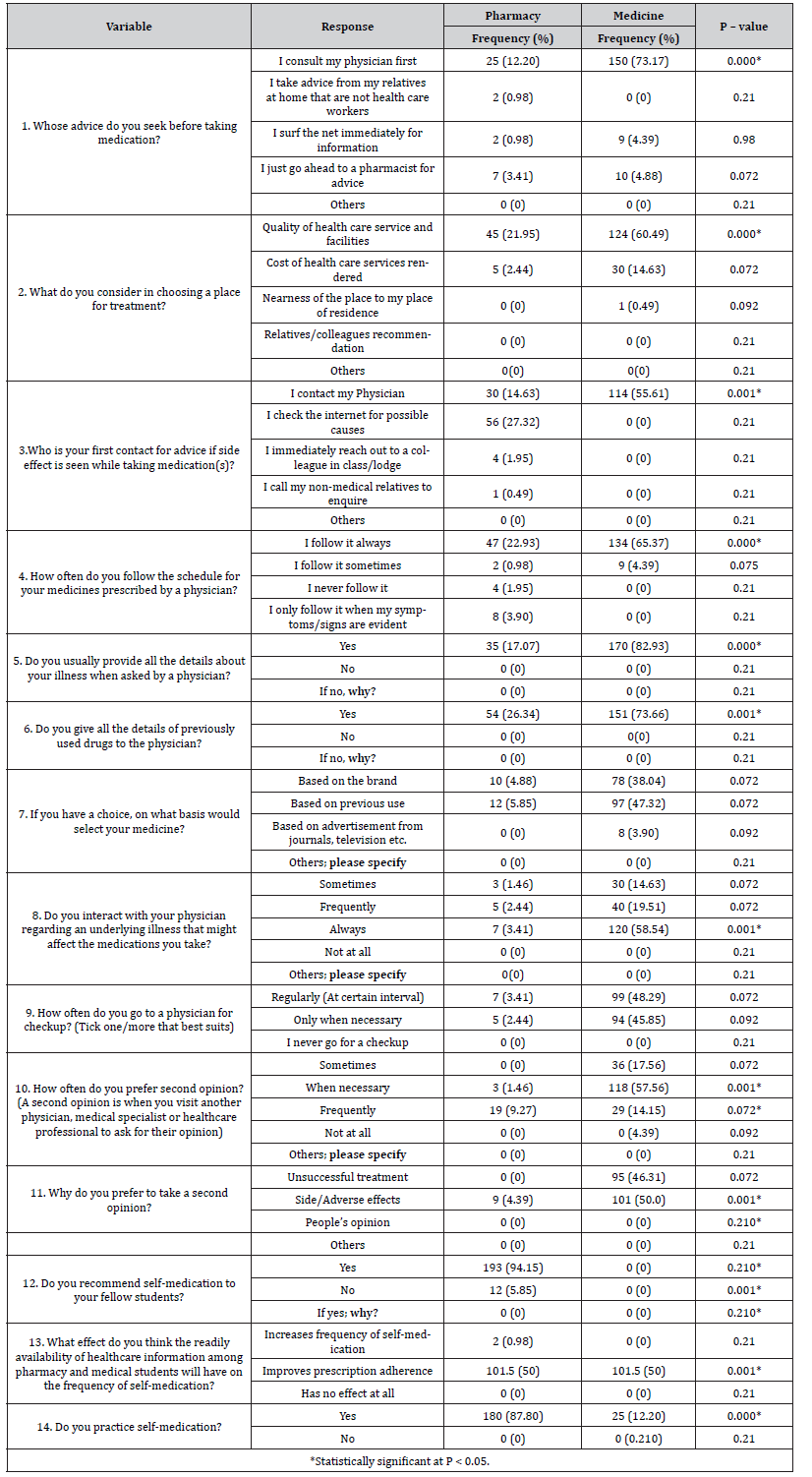
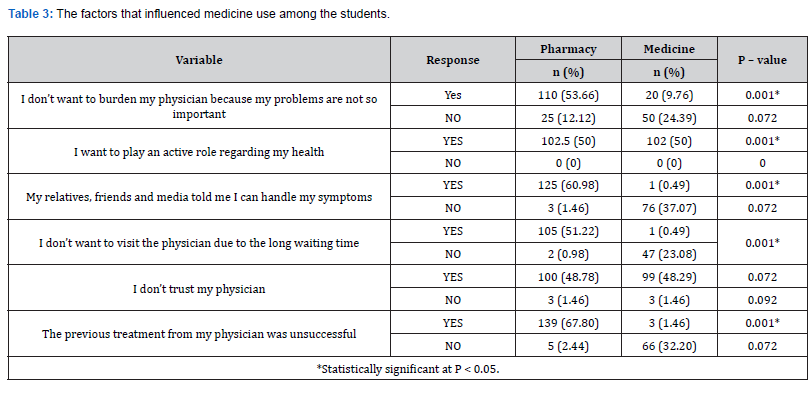
Table 3:The factors that influenced medicine use among the students.
Discussion
The students have good knowledge of self-medication and agreed that they recommended self-medication to their fellow students. The reason for this could be due to their pharmacology and clinical knowledge, which was common among the final year students medical and pharmacy students. The prevalence of selfmedication among the students was determined through their responses on the use of medicine in which majority of them indicated that they are frequently involved in the practice self-medication. The findings revealed that the practice of self-medication was relatively high among the medical students but low among the pharmacy students. The observed prevalence rates for medical students were slightly higher than that reported in a previous study by Idoko et al., whose study reported a prevalence of 85.7% [8]. However, another study by Mgbahurike et al., reported a high prevalence rate (83.8%) of self-medication among pharmacy students as against the 22.20 % prevalence recorded among the pharmacy students in this study [9]. In another study by Auta et al., the prevalence of self-medication among pharmacy students was 53.2%, which was more than twice the value in our study [10]. A study by Gelayee, reported a similar low prevalence of self-medication (32.7%) among students from Ethiopia, which is in line with our findings among the pharmacy students [11]. The prevalence among medical students in Ethiopea and Bahrain was below average [12,13]. While that obtained among strudents in India Egypt, Palestine, Slovania and Serbia were well above average [14-18].
The medication profile, pattern, and practice of medicine use among the students were assessed, and the result showed a significant difference between the response of the pharmacy students and the medical students. The finding revealed that relatively, the pharmacy students (25, 12.2 %) consulted their physicians when seeking medication advice. Majority of the medical students do the same. Very few of them took advice from their relatives, surf the internet and go to the pharmacists for advice. The difference in their perception could be due to their individual exposure in their respective departments. The gap in knowledge between the pharmacy and medical student proposes a need to revise the curriculum of the students. This is in line to incorporate relevant concepts of self-medication to equip the students for their future responsibilities. The outcome is in line with the study by Akande-Sholabi et al., where the pharmacy students in their study showed relatively higher knowledge of self-medication than their counterparts in nursing and medicine [19]. Based on their consideration while choosing a place of treatment, they considered the quality of health care services and facility more important, followed by the cost of care rendered.
Other factors such as proximity and recommendation from relatives were not indicated as factors for both the pharmacy and medical students. On whom to contact for advice if side effect is seen while taking some medication, majority of the pharmacy and medical students said they do contact physicians. However, there was a significant difference `between the two groups, and none of the medical students check the internet for such information. All the medical and pharmacy students usually provided the detailed information about their illness and also gave details of their past medical history to the physicians. On the basis on which they could choose their medicine, majority of them said it was based on previously used medicines while other said their choices were based on brands used. There was no significant difference on their basis for the choice of medicine. Although most of them frequently interacted with their physicians regarding their underlying illnesses, a few of the pharmacy students frequently prefer second opinion, that is, they prefer to visit another physician, medical specialist or healthcare professional to ask for their opinion. More than half of the medical students do same. The reason for their second opinion preference was due to side/adverse effects. Majority of the students were of the opinion that readily available healthcare information among pharmacy and medical students will improve prescription adherence compared to increase in the frequency of self-medication.
The reasons given for self-medication among the students varied. More than a half of the pharmacy students said they do not want to burden their physicians because they felt their problems were not very serious and a few of the medical students also agreed to that. This is similar to a study in Brazil, China and Rwanda where the medical and pharmacy students had self-medication when they considered their conditions to be minor or transient [20, 21]. However, a few of them said no, while a half 50 of both pharmacy and medical students opined that they were involved actively in taking care of their health. Majority of the pharmacy students indicated that they handle their health issues based on factors like social media speculation and friend’s advice, as well as 37.07% of medical students. Another factor for self-medication was long time of waiting at the hospital which affected a half of the pharmacy students. Other factors that encouraged their self-medication was that they do not trust their physicians for advice and other health related issues. Most of pharmacy students do not visit their physician because previous treatment did not work, this was also the case of one-third of the medical students. This outcome is in line with that reported by a study in Bayelsa State Nigeria, where the major determinant of self-medication among the students includes self-decision, friends and family recommendations [22].
Summary
The prevalence of self-medication among the pharmacy and medical students was relatively high. The study suggested that the students’ practice of self-medication was frequent and long waiting time at hospitals was a contri buting factor. Another predictor of self-medication among the students includes self-decision, friends and family recommendations. There was evidence that the level of knowledge about medicine in general may have influenced the students’ attitude and perception about medicines for particular illnesses. Thus, the impact of irrational use of medicine among the students is still worrisome and thus, calls for a concern in the public health sectors. There is thus a need for sensitization of medical and pharmacy students on the advantages and disadvantages of selfmedication in order to ensure rational medicine use. Policies to control the use of over- the- counter drugs will be essential in view of the enormous adverse effects of self-medications. Healthcare workers should increase the consciousness of rational use of medicines among undergraduate students especially in developing countries where medicines can be sourced without prescription.
Conflict of Interest
The authors have none to declare.
Funding
No funding was received for this study.
Acknowledgement
The authors do sincerely acknowledge the Dean, Provost and management of the Faculty of Pharmaceutical Sciences and the College of Medicine, Nnamdi Azikiwe University for a conducive the conducive atmosphere to carry out the study.
References
- WHO (2017) Introduction to Drug Utilization Research: Chapter 4: Economic aspects of drug use (pharmacoeconomy): 4.3 Cost-effectiveness analysis.
- Anteneh Assefa Desalegn (2013) Assessment of drug use pattern using WHO prescribing indicators at Hawassa University teaching and referral hospital , south Ethiopia : a cross-sectional study. BMC Health Serv Res 13: 170.
- Bennadi D (2014) Self-medication: A current challenge. Journal of Basic and Clinical Pharmacy 5(1): 19-23.
- OA Babatunde, JO Fadare, OJ Ojo, KA Durowade, OA Atoyebi, et al. (2016) Self-medication among health workers in a tertiary institution in South-West Nigeria. In Pan African Medical Journal 24: 312.
- Fernando ADA, Bandara LMH, Bandara HMST, Pilapitiya S, De Silva A, et al. (2017) A descriptive study of self-medication practices among Sri Lankan national level athletes. BMC Research Notes 10(1): 1-12.
- Sirak Tesfamariam, Indermeet Singh Anand, Ghide Kaleab, Samson Berhane, Biruck Woldai, et al. (2019) Self-medication with over the counter drugs, prevalence of risky practice and its associated factors in pharmacy outlets of Asmara, Eritrea. BMC Public Health 19(1): 159.
- Gutema GB, Gadisa DA, Kidanemariam ZA, Berhe DF, Berhe AH, et al. (2011) Self-medication practices among health sciences students: The case of mekelle university. Journal of Applied Pharmaceutical Science 1(10): 183-189.
- Idoko CA, Omotowo BI, Ekwueme OE, Chidolue I, Ezeoke U, et al. (2018) Prevalence and Pattern of Self-medication among Medical Students in a Nigerian University 23(1): 189-193.
- Mgbahurike AA, Nenwi GF (2020) Prevalence, Knowledge, Practice and Perception of Self Medication among Pharmacy Students in a Nigerian tertiary Institution. Journal of Medical Biomedical and Applied Sciences 8(8): 494-503.
- A Auta, SB Banwat, CN Sariem, D Shalkur, B Nasara, et al. (2012) Medicines in pharmacy students’ residence and self-medication practices. Journal of Young Pharmacists 4(2): 119-123.
- Gelayee DA (2017) Self-Medication Pattern among Social Science University Students in Northwest Ethiopia. Journal of Pharmaceutics: 8680714.
- Tuyishimire J, Okoya F, Adebayo AY, Humura F, Lucero-Prisno Iii DE, et al. (2019) Assessment of self-medication practices with antibiotics among undergraduate university students Pan Afr Med J 33: 307.
- James H, Handu SS, Al Khaja KA, Otoom S, Sequeira RP (2006) Evaluation of the knowledge, attitude, and practice of self-medication among first-year medical students Med Princ Pract 15(4): 270-275.
- Kumar N, Kanchan T, Unnikrishnan B, Rekha T, Mithra P, et al. (2013) Perceptions and practices of self-medication among medical students in coastal South India. PLoS One 8(8): e72247.
- N F A El Ezz, H S Ez-Elarab (2011) Knowledge, attitude and practice of medical students towards self-medication at Ain Shams University, Egypt J Prev Med Hyg 52(4): 196-200.
- Sawalha AF (2008) A descriptive study of self-medication practices among Palestinian medical and nonmedical university students Res Soc Adm Pharm 4(2): 164-72.
- Klemenc-Ketis Z, Hladnik Z, Kersnik J (2010) Self-medication among healthcare and non-healthcare students at University of Ljubljana, Slovenia Med Princ Pract 19(5): 395-401.
- Lukovic JA, Miletic V, Pekmezovic T, Trajkovic G, Ratkovic N, et al. (2014) Self-medication practices and risk factors for self-medication among medical students in Belgrade, Serbia PLoS One 9(12): e114644.
- WA Sholabi, AT Ajamu, R Adisa (2021) Prevalence, knowledge and perception of self-medication practice among undergraduate healthcare students Journal of Pharmaceutical Policy and Practice 14(1): 49.
- Gama ASM, Secoli SR (2017) Self-medication among nursing students in the state of Amazonas - Brazil. Rev Gaucha Enferm. 38(1): e65111.
- Lei X, Jiang H, Liu C, Ferrier A, Mugavin J, et al. (2018) Self-medication practice and associated factors among residents in Wuhan, China Int J Environ Res Public Health 15(1): 68.
- Owonaro PA, Okorafor GC, Eniojokun J (2015) Attitudes And Patterns Of Self- Medication Among Undergraduate Students OfNiger Delta University In Wilberforce Island. Journal of Pub Health 1(2): 1-12.
-
Ogbonna Brian O*, Achuagu Vera O, Eze Uchenna IH, Onwuchuluba Ebele E and Omuta Michael C. Evaluation Of Medicine Use Pattern and Practices Among Pharmacy and Medicine Students of a Nigerian Federal University. Arch Phar & Pharmacol Res. 3(2): 2022. APPR.MS.ID.000557.
-
Drug, Antibiotics, Exacerbation, Over the Counter (OTC), Anatomical Therapeutic Chemical (ATC), Enormous adverse effects, Illnesses.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






