Research Article
Research Article
Measurements In Diagnosed and Undiagnosed Asthma Exacerbations in Children and Review of Literature.
Melpomeni Bizhga*
Department of Service of Pediatric Pneumology, Mother Teresa Hospital, Tirana
Melpomeni Bizhga, Department of Service of Pediatric Pneumology, Mother Teresa Hospital, Tirana
Received Date:October 28, 2024; Published Date:November 11, 2024
Abstract
Children with asthma crises were evaluated for subjective dyspnea scale perception and objective measurements as PEFR, oxygen saturation, heart rate, and respiratory rate.
The study involved a cohort of 38 children, categorized into 17 newly diagnosed (NDA) and 21 previously diagnosed asthma (DA) patients. It examined factors such as dyspnea, PEFR, oxygen saturation, heart rate, and respiratory rate to understand the differences in symptom perception and disease manifestation between the two groups.
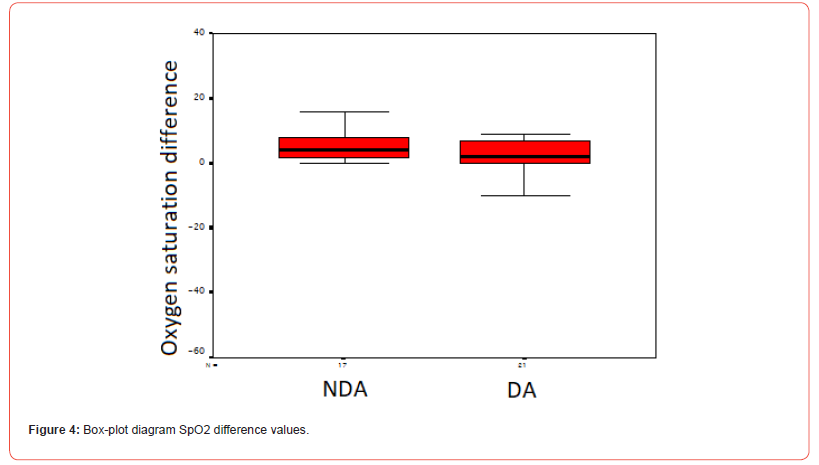
The study found that PEFR variation was more significant in NDA cases than in DA cases, and the middle value was higher. This study found no significant difference in heart rate or oxygen saturation values between non-dependent asthma (NDA) and dependent asthma (DA) patients. However, the subjects with NDA manifested a more significant decrease in respiratory frequency than those with DA, though this result was at the limits of statistical significance (p=0.07).
One of the study’s key findings is the lack of statistically significant differences in heart rate and oxygen saturation between the NDA and DA groups. These physiological parameters may not be the best asthma severity or type indicators.
In contrast, respiratory frequency appears to be a more sensitive marker of clinical improvement in asthma.
Material and Method
Study and population: children presented to emergency department in UHC Nene Tereza, Tirana, with asthma crises during fall 2023 were divided in two groups: previously diagnosed with asthma (DA) and never diagnosed with asthma (NDA). They were evaluated for dyspnea, respiratory frequency, cardiac frequency, oxygen saturation, and ability to generate PEFR.
The data were analyzed by SPSS 16.0.
This study employs a cross-sectional observational design
to explore the subjective perception of dyspnea (shortness of
breath) and objective measurements of respiratory distress in
children experiencing an asthma crisis. The study initially included
44 children who had either ceased or not initiated prophylactic
asthma treatment and presented to the pediatric emergency
department. The study established clear exclusion criteria to ensure
a homogeneous participant pool for meaningful data analysis and
comparison:
Age Restriction: The study was restricted to children aged
five years and above. This criterion ensured that participants could
reliably communicate their dyspnea perceptions and physically
comply with the study’s procedural requirements.
Response to Salbutamol: Children who showed complete
alleviation of symptoms immediately following the initial salbutamol
aerosol treatment were excluded. This selection mechanism was
vital to concentrate the study’s scope on children exhibiting more
persistent asthma symptoms, aligning with the investigation’s
primary interest in dyspnea perception and respiratory distress.
For the remaining participants, the effectiveness of salbutamol inhalation was a critical criterion for study inclusion. This effectiveness was defined quantitatively as an increase in Forced Expiratory Volume in 1 second (FEV1) of at least 12% from the baseline measurement at the end of the first hour after salbutamol administration, accompanied by clinical signs indicative of asthma. This objective criterion was employed to confirm the diagnosis of bronchial asthma in previously undiagnosed cases and gauge the airways’ responsiveness to bronchodilator treatment.
Upon meeting the inclusion criteria, children were stratified
into two principal groups based on their asthma diagnosis history,
creating a structured comparison to illuminate differences in
subjective dyspnea perception and objective respiratory distress
indicators:
Undiagnosed Asthma Group (NDA): This cohort included
17 children without a prior asthma diagnosis. This group’s
inclusion offered a unique lens to examine dyspnea perception
and respiratory distress in children whose asthma had not been
previously recognized by medical professionals.
Diagnosed Asthma Group (DA): This group consisted of 21
children with a history of diagnosed asthma who had not adhered
to prophylactic treatment. The objective of this group was to
investigate the influence of asthma diagnosis awareness on the
perception of dyspnea and the manifestation of respiratory distress
during an asthma attack.
Results
Patients were asked to answer the simple question at the beginning of the evaluation and after 6 hours. The answer was categorical (Yes/No).
For the NDA cohort, out of 17 cases, one person reported no dyspnea before and after treatment. At the same time, 15 individuals transitioned from experiencing dyspnea initially to not experiencing it after the treatment, and 1 reported dyspnea at both times. Meanwhile, among the DA cases, with a total of 21 individuals, 5 reported no dyspnea at both time points, 2 reported dyspnea initially, which was not present post-treatment, and 14 individuals noted a transition from having dyspnea to not having it after treatment. No individuals in the diagnosed group reported dyspnea persisting after the treatment. This data, reflecting the categorical shift in the perception of dyspnea, formed the basis for calculating the McNemar test, which confirmed a statistically significant change within both groups.
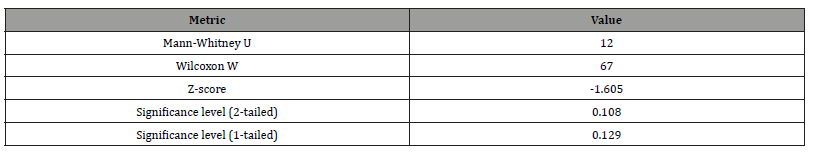
Table 1:Comparison of dyspnea before and after treatment (NDA/DA) – McNemar test results.
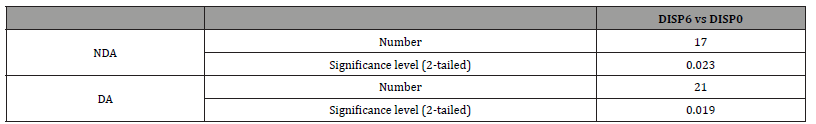
The interpretation of the McNemar test results demonstrates the influence of disease awareness on the perception of symptoms among individuals with asthma. In the context of this study, the statistical analysis points to a significant reduction in the perception of dyspnea in NDA and DA groups after 6 hours.
For the NDA group, most individuals (15 out of 17) reported no dyspnea after 6 hours, having initially reported it. This significant change, with an exact significance level of 0.023, suggests a newly realized perception of symptom relief. It may reflect an increased awareness of their respiratory symptoms after experiencing and recognizing the sensation of dyspnea followed by its absence.
In the DA group, all individuals who initially reported dyspnea (14 out of 21) no longer perceived it after 6 hours, signifying a disappearance of symptoms with a significance level of 0.019. This group’s experience suggests that having a diagnosis and a likely pre-existing awareness of their condition enables a more nuanced perception of symptom changes. These individuals may be more finely attuned to the ebb and flow of their symptoms, capable of discerning the onset of an asthma-related discomfort and the subsequent relief that follows an intervention or the natural progression of the condition.
Impact of the crisis on PEFR
Table 2:Variation of PEFR after the first 6 hours of medication.
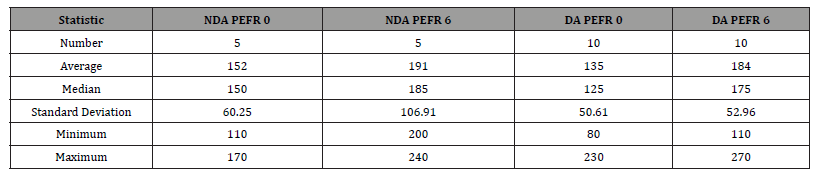
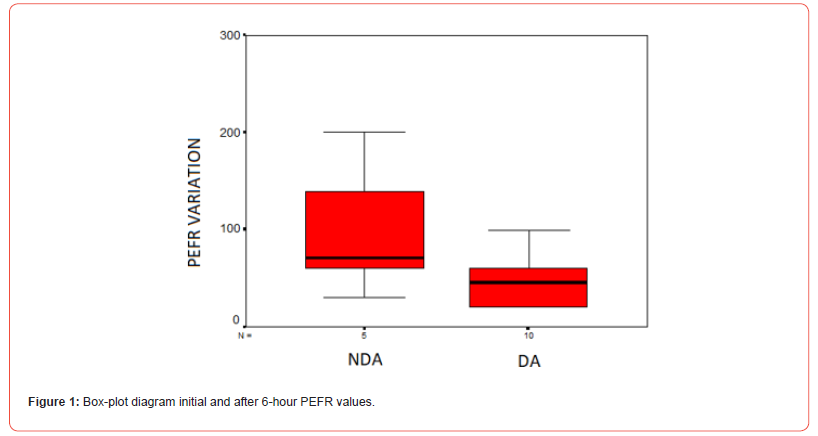
The initial examination of PEFR data in illustrates distinct trends within NDA and DA groups, observed over a 6-hour interval. In the NDA cohort, the recorded PEFR values indicate an increase and a notable expansion in the variability of these measurements. Such an increase in variability suggests that individuals within the NDA group exhibit a wide range of responses, potentially reflecting differences in the condition’s natural history or the individual’s physiological response to their asthma status.
In contrast, the DA group demonstrates a smaller range of PEFR variability. This relative homogeneity might imply a more stable response amongst these patients. This could be attributed to regular monitoring and management of their diagnosed condition, leading to a potentially more controlled asthma status. The response pattern in the DA group also points to the benefit of having an established asthma management plan that modulates the variability of the condition’s impact on lung function.
When interpreting the results of the Mann-Whitney test, demonstrated in the differences between the NDA and DA groups regarding median PEFR improvement do not reach statistical significance. This outcome implies that while numerical differences in PEFR improvements are observable, they do not establish a clear statistical distinction between the groups.
Table 3:Variation of PEFR after the first 6 hours of medication.
Given the results from the Mann-Whitney test that do not demonstrate statistical significance, it suggests a need for additional research involving larger sample sizes to determine any potential differences conclusively. Such findings could be essential in understanding the influence of a formal asthma diagnosis on the variability of PEFR readings. The observed broader range of variability in the PEFR amongst the NDA group could point to a less consistent response to their condition, hinting at the potential benefits of timely diagnosis and management in achieving a more stable condition, as seen in the DA group. This variability and the study’s current findings invite further exploration better to interpret the relationship between diagnosis awareness and respiratory function.
Impact of the crisis on HR, RR, SpO2
Table 4:Comparison of mean differences in heart rate, respiratory rate and O2 saturation by type of medication (oral vs. intravenous).
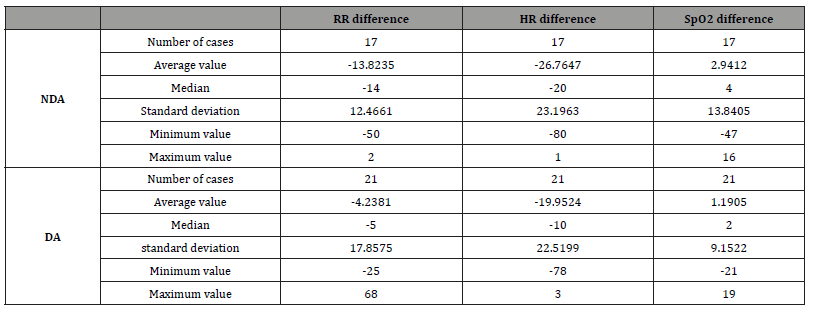
The NDA group significantly decreased HR and RR following the intervention. The substantial average reductions in RR (-13.8235) and HR (-26.7647) for the NDA group suggest a pronounced response to the asthma crisis management, effectively mitigating the acute symptoms manifested through elevated physiological stress.
In contrast, the DA group demonstrated a less pronounced decrease in HR and RR. The average change in HR (-19.9524) was somewhat closer to that of the NDA group, but the average change in RR (-4.2381) was notably more minor. This disparity could imply that patients with diagnosed asthma, possibly due to their ongoing management plans, initially present with less severe deviations from their baseline physiological states during an asthma crisis or respond differently to the intervention.
Although relatively small, the positive average changes in SpO2 for both groups post- treatment, +2.9412 for NDA and +1.1905 for DA, indicate improved oxygenation. This improvement, particularly more noticeable in the NDA group, underscores the effectiveness of the intervention in enhancing respiratory function and oxygen delivery.
The wide range in the minimum and maximum values across both groups, especially notable in the drastic differences in RR and HR, underscores the heterogeneity in patient responses to treatment. The more significant variability observed within the NDA group could suggest a more diverse range of asthma crisis severity at presentation or varied treatment efficacy, which the absence of a formal asthma management plan might influence.
The observed differences in response between the NDA and DA groups could also reflect the influence of prior asthma management on the acute response to standardized emergency treatments. While the DA group, potentially benefiting from ongoing asthma management strategies, might exhibit a more moderated physiological response to the crisis and treatment, the NDA group’s broader range of physiological responses may highlight the critical role of early diagnosis and consistent management in moderating the impacts of asthma crises.
The standardization of the data about the differences in heart rate, respiratory rate, and oxygen saturation-before and after the intervention across the NDA and DA groups - was further analyzed using the Mann-Whitney test. This statistical approach assessed the significance of the observed differences between the two patient groups, providing a more robust understanding of the treatment impact within a standardized statistical framework. This subsequent analysis is crucial for corroborating the initial observations and offering a statistically validated perspective on the effectiveness of asthma crisis management in children, considering the variability of physiological responses highlighted in the previous assessment.
Table 5:Comparison of mean differences in heart rate, respiratory rate and O2 saturation by type of medication – Mann-Whitney test results.
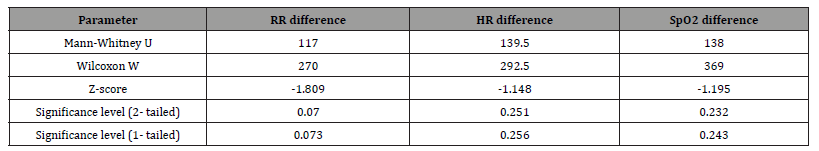
The key findings from the analysis indicate no statistically significant difference between the mean heart rate and oxygen saturation differences between the NDA and DA groups. This is evidenced by the significance levels for HR differences (0.251 for 2-tailed and 0.256 for 1-tailed) and SpO2 differences (0.232 for 2-tailed and 0.243 for 1-tailed), which are well above the conventional threshold for statistical significance (usually p < 0.05). This outcome suggests that the treatment’s impact on heart rate and oxygen saturation is consistent across both groups, indicating uniform effectiveness in addressing these specific parameters of the asthma crisis, regardless of the prior diagnosis status.
However, a more nuanced observation emerges from analyzing respiratory rate differences. The significance level for RR difference stands at 0.07 (2-tailed), which, while not conventionally significant, is at the cusp of statistical significance and indicates a trend. This suggests that subjects in the NDA group experienced a more pronounced decrease in respiratory rate than those in the DA group.
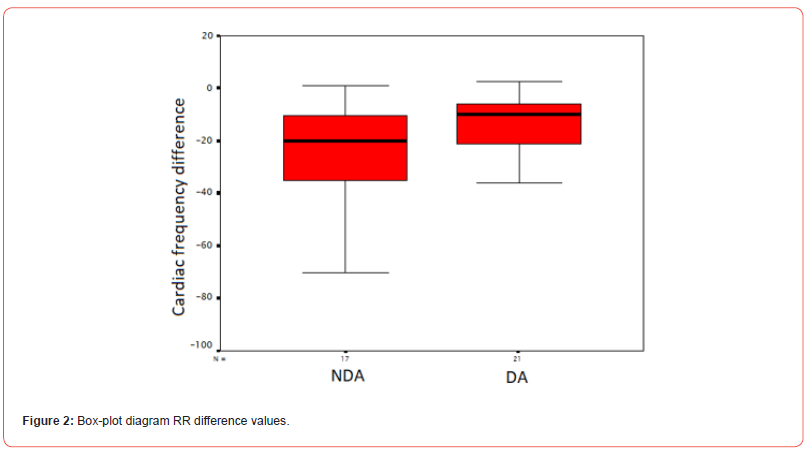
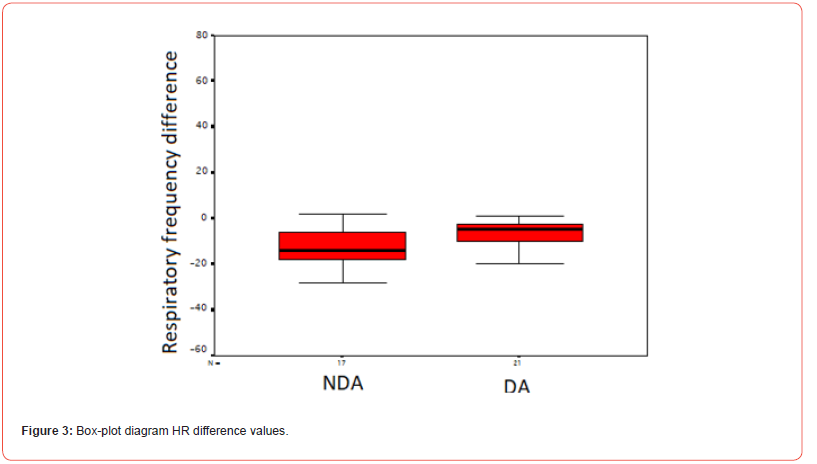
This finding, being on the threshold of statistical significance, points to a potential differential impact of the treatment of respiratory rate based on diagnosis status. It hints at the possibility that individuals without a prior diagnosis of asthma may exhibit a more significant response regarding respiratory rate reduction following the standardized treatment protocol.
Discussion of asthma crisis and measurement parameters
Asthma stands as a critical non-communicable disease with profound public health consequences worldwide, affecting both the pediatric and adult populations. This condition is notably linked with high rates of morbidity and, in extreme cases, mortality. Currently, asthma is identified as the 16th leading cause of reduced life expectancy due to disability and ranks 28th in terms of global disease burden, as measured by disability-adjusted life years [1]. It is estimated that approximately 300 million individuals globally have asthma, with projections suggesting that this number could rise by another 100 million by 2025 [2].
Significant variations are observed in asthma’s incidence, severity, and mortality rates across different regions. While high-income nations report higher instances of asthma, a disproportionate number of asthma-related fatalities occur in lowto middle-income countries [3]. Despite decades of advancements in therapeutic options for asthma, substantial improvements are still needed in the area of patient education, particularly concerning the understanding of dyspnea, a common and distressing symptom of the disease.
Elevating the focus on primary healthcare is essential for mitigating the risk of exacerbations and complications associated with asthma and for diminishing the rates of hospital admissions and fatalities due to this condition [4]. While severe asthma in children is relatively uncommon, it is nonetheless a serious health issue that can lead to significant morbidity and occasionally mortality, presenting substantial challenges in treatment. Various definitions of severe asthma share a core characteristic: the inability to achieve control despite the administration of high doses of inhaled corticosteroids. Depending on the specific definition applied, the incidence of severe asthma in children who have asthma can reach up to 5% of the affected population [5].
This study found no significant difference in heart rate or oxygen saturation values between non-dependent asthma (NDA) and dependent asthma (DA) patients. However, the subjects with NDA manifested a more significant decrease in respiratory frequency than those with DA, though this result was at the limits of statistical significance (p=0.07).
One of the study’s key findings is the lack of statistically significant differences in heart rate and oxygen saturation between the NDA and DA groups. These physiological parameters may not be the best asthma severity or type indicators.
In contrast, respiratory frequency appears to be a more sensitive marker of clinical improvement in asthma. In a mild asthma crisis, the respiratory frequency does not change or increase to 35% above average. In a moderate asthma crisis, the respiratory frequency increases from 35% to 50% above average; in a severe asthma crisis, the frequency increases by over 50%.
The decrease in respiratory frequency observed in the NDA group is a clear indicator of clinical improvement and normalization of breathing. This is because an increase in respiratory frequency often occurs as a compensatory mechanism when the lungs fail to perform their function adequately, requiring increased work to maintain adequate gas exchange.
Oxygen saturation is typically above 95% in a mild asthma crisis. In a moderate asthma crisis, it is between 90-95%, and in a severe asthma crisis, it is below 90%.
Since evaluating arterial blood gases and capillary acid-base balance can be challenging to obtain and is relatively expensive for assessing acute respiratory insufficiency type 2, oxygen saturation measurement is a simple, non-invasive, and cost-effective alternative. However, arterial blood gas analysis is necessary in lifethreatening crises, where a PaO2 value of less than 60 mmHg would be a concerning finding.
The study by S. Koripadu et al. [6] detailed PEFR in asthmatic children and observed its response to bronchodilator therapy. The researchers reported a mean pre-bronchodilator PEFR of 120 L/ min and a mean post-bronchodilator PEFR of 149 L/min, indicating a mean improvement of approximately 23%. This significant response highlights the substantial bronchial reactivity among the asthmatic children studied compared to the control group, who’s median PEFR was considerably higher at 200 L/min.
The present research also explored PEFR in asthmatic patients, focusing on differentiating between NDA and DA cases. The baseline PEFR measurements varied more significantly between the groups in the present study, with the NDA group starting at an average PEFR of 224 L/min. In comparison, the DA group had a lower baseline of 135 L/min. Regarding the post-treatment PEFR values, the author’s study reported an average increase of 149 L/min, reflecting a 23% improvement. In contrast, the present research observed a much higher post-treatment PEFR in the NDA group, with an average of 324 L/min, while the DA group’s average was 184 L/min. This indicates a more substantial percentage increase in PEFR, particularly for the NDA group, than the findings of the researcher’s study. There could be multiple reasons for the variations in the observed PEFR responses between the two studies. Firstly, the study populations and settings may have varied, as the author’s study concentrated on children with bronchial asthma in a controlled clinical environment. At the same time, the present research may have involved a broader demographic with varying asthma severities and baseline characteristics, such as age and general health conditions [7].
In their work, K. Ushakiran et al. [8] studied the response of PEFR to bronchodilator therapy in children aged 5 to 12 who were diagnosed with bronchial asthma. Their results, obtained from a controlled group of 50 children with asthma, revealed a mean pre-bronchodilator PEFR of 120.8 liters per minute (L/min) and a post-bronchodilator PEFR of 146.6 L/min, reflecting an average percentage improvement of 21.3% across all participants. This study emphasized the utility of PEFR measurements in monitoring the response to asthma treatment.
Some notable differences emerge when comparing the findings of the K. Ushakiran et al. study with the current research. In the pre-bronchodilator PEFR measurements, the colleague’s study reported a mean value of 120.8 L/min, while the present research found higher initial PEFR in both groups. Regarding the post-bronchodilator PEFR, the researcher’s study observed an average of 146.6 L/min. In contrast, the present research reported significantly higher post- treatment PEFR values.
The percentage improvement in PEFR also differed between the studies. The study by K. Ushakiran et al. reported an average improvement of 21.3% after administering bronchodilators. However, in the present research, the percentage improvement is approximately 44.6% for the NDA group and 36.3% for the DA group, indicating a more substantial response to the treatment. The differences in the PEFR responses between the two studies may be attributed to various factors, such as the specific characteristics of the study populations, the severity of asthma, the treatment protocols, and the medications used. The present research’s focus on differentiating between NDA and DA cases may have also contributed to the observed variations in the PEFR responses.
In their work, U. C. Onubogu et al. [9] studied the correlation and predictive value of oxygen saturation and the percentage of predicted peak expiratory flow rate (% predicted PEFR) in identifying children with mild symptoms of asthma exacerbation. They found a moderate correlation (r = 0.44) between these parameters in children with uncontrolled asthma experiencing mild symptom exacerbations. The study established that children with SpO2 between 92% and 95% were significantly more likely to exhibit mild symptoms of asthma exacerbation.
Some notable differences emerge when comparing the findings of colleagues’ studies with the present research. Regarding PEFR values, researchers study reported that the % predicted PEFR ranged notably, with mean values for participants with no symptoms and mild symptoms of asthma exacerbation being 77.8% and 64.1%, respectively. In contrast, the present research found higher initial PEFR readings, with the NDA group starting at 224 litres per minute (L/min) and the DA group at 135 L/min.
Regarding the change in PEFR post-treatment, U. C. Onubogu et al. study observed a mean increase in %predicted PEFR after bronchodilator therapy, indicating a moderate predictive value of PEFR in monitoring exacerbation severity. This finding aligns with the present research, demonstrating a substantial increase in PEFR after treatment, especially in the NDA group, reflecting significant responsiveness to bronchodilator therapy.
In terms of correlation analysis, colleagues’ study found a significant but moderate correlation between % predicted PEFR and SpO2 in uncontrolled asthma cases with mild symptoms, suggesting that these measures can help identify exacerbation risks. In contrast, the present research found no correlation between these parameters.
The differences in the findings between the two studies may be attributable to several factors. Colleagues’ study focused on a cohort with uncontrolled asthma and mild exacerbations, potentially capturing a different severity spectrum than the present study, including individuals with varied treatment responses (NDA vs DA). Additionally, researchers’ use of %predicted PEFR, a normalized measure accounting for age, sex, and height, may have provided a more comparative assessment across different patient groups, which could explain the observed correlations with SpO2. Furthermore, geographical and demographic differences, such as the specific regional asthma characteristics and genetic backgrounds in Nigeria, where colleagues’ study was conducted, could influence PEFR norms and SpO2 levels, differing from the present research settings.
Overall, both studies highlight the critical role of PEFR in monitoring asthma treatment responses, especially postbronchodilator changes. The researcher’s additional focus on SpO2 correlations offers an expanded diagnostic toolset that could enhance early intervention strategies in asthma management. Combining these measures could provide a more comprehensive assessment of asthma exacerbation severity and control.
During their work, D. A. Kaminsky et al. [10] studied the fluctuations of peak expiratory flow (PEF) and its implications for asthma treatment failure. The study focused on temporal variability and self-similarity (denoted as α) in PEF measurements from asthma patients participating in the LOCCS trial. They found that increased variability in PEF quantified as the coefficient of variation (CVPEF) and higher values of α were predictive of treatment failure. Specifically, patients with higher CVPEF and α during the treatment phase were likelier to experience treatment failures.
In summary, the higher PEFR and FR values observed in the present study highlight the importance of considering sample characteristics and the context of measurements in interpreting asthma research findings. Combining multiple objective measures and employing sophisticated analytical techniques can enhance our understanding of asthma control and improve clinical practice.
Acknowledgement
None.
Conflict of Interest
None.
- Asher MI, García-Marcos L, Pearce NE, Strachan DP (2020) Trends in worldwide asthma prevalence. European Respiratory Journal 56(6): 2002094.
- Dharmage SC, Perret JL, Custovic A (2019) Epidemiology of asthma in children and adults. Frontiers in pediatrics 7: 246.
- Mattiuzzi C, Lippi G (2020) Worldwide asthma epidemiology: insights from the Global Health Data Exchange database. In International forum of allergy & rhinology 10(1): 75-80.
- Serebrisky D, Wiznia A (2019) Pediatric asthma: a global epidemic. Annals of global Health 85(1): 6
- Ahmed H, Turner S (2019) Severe asthma in children-a review of definitions, epidemiology, and treatment options in 2019. Pediatric pulmonology 54(6): 778-787.
- Koripadu S, Yanamandala HV, Yarlagadda S (2017) A CLINICAL STUDY OF BRONCHIAL ASTHMA IN CHILDREN AGED 5 TO 15 YEARS. Population 4(66): 3963-3968.
- Srinivasa K, Ushakiran CB, Rudrappa S (2015) Clinical study of bronchial asthma in children aged 5 to 12 years with special reference to peak expiratory flow rate. Int J Contemp Pediatr 2(4): 297-302.
- Onubogu UC, Ayuk A (2022) Pulse oximetry and peak expiratory flow rate correlations in acute asthma exacerbation in children. Nigerian Journal of Clinical Practice 25(11): 1896-1903.
- Kaminsky DA, Wang LL, Bates JH, Thamrin C, Shade DM, etal. (2017) Fluctuation analysis of peak expiratory flow and its association with treatment failure in asthma. American journal of respiratory and critical care medicine 195(8): 993-999.
- Ohwada A, Sato K (2019) Heterogeneity of perception of symptoms in patients with asthma. Journal of Thoracic Disease 11(12): 5218.
-
Melpomeni Bizhga*. Measurements In Diagnosed and Undiagnosed Asthma Exacerbations in Children and Review of Literature. Anat & Physiol Open Access J. 1(5): 2024. APOAJ.MS.ID.000524.
-
Newly Diagnosed; Diagnosed Asthma; Physiological Stress; Forced Expiratory Undiagnosed Asthma; Non-Dependent Asthma; Dependent Asthma
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.