Research Article
Research Article
Layered Morphological Perspective of The Temporal Region and Its Relevance in Temporal Contouring Procedures
Gladys Velazco Viloira1*, Nancy Diaz de Villabona2, Said Rodea Hernandez3, Victor Mercado4 and Marta Amin Merino4
1Latin American Center for Medical Training and Research (CLEMI), Bogotá, Colombia
2Universidad de Los Andes, facultad de Odontologia, merida Venezuela
3EPILOG, Clinics Merida, Yucatan, Mexico
4Icron Medical Instituto region metropolitana Santiago de Chile, Chile
Gladys Velazco Viloria, Latin American Center for Medical Training and Research (CLEMI), Bogotá, Colombia
Received Date:April 11, 2025; Published Date:April 21, 2025
Abstract
Changes in the contour of the temporal region represent one of the most significant challenges within minimally invasive facial harmonization approaches, aiming to respond harmoniously and effectively to the demands of patients seeking to prevent or slow down this hallmark of aging. Clinically, the temporal region is a critical anatomical area that directly influences the structural shape and proportions of the face, evidently modifying facial appearance. Therefore, in-depth knowledge of this area is fundamental. In this study, 30 hemifaces were dissected, exposing the temporal area from the cranial to the ocular regions to verify the positioning and distribution of the anatomical layers, assessing each of the spaces and layers involved. The identification of three distinct temporal fat compartments — one located beneath the skin, another beneath the Superficial Musculoaponeurotic System (SMAS), and the deepest overlying the temporal muscle aponeurosis — demonstrates that fat distribution within the temporal fossa differs from that observed in other facial anatomical units. This anatomical study provides a comprehensive description of the temporal region’s anatomy, including the bony insertions of the temporal muscle, the fascial layers that define a clear stratigraphy, the characteristics of dermal and adipose tissues, and the neurovascular structures present in the area. The findings demonstrate that the deep fat tissue in the temporal region is unique among facial areas, being located not beneath the muscle, but rather over its aponeurosis.
Keywords:Fascia; temporal fossa; temporal adipose tissue; temporal stratigraphy
Introduction
Changes in the contour of the temporal region represent one of the most significant challenges within minimally invasive facial harmonization approaches, aiming to respond harmoniously and effectively to the demands of patients seeking to prevent or slow down this hallmark of aging. Clinically, the temporal region constitutes a critical anatomo-clinical area that directly influences the structural shape and proportions of the face, significantly modifying facial appearance. Differentiating between the various functional facial regions by considering their anatomical characteristics as a multi-layered structure interconnected by a system of facial retaining ligaments, which together form a threedimensional, laminar framework, greatly assists specialists in refining their techniques. These interconnected elements continue either toward the dermis or toward muscular or bony tissues, as recent literature reports. Each anatomical layer of the face undergoes changes over time according to its own biomechanics, and individuals from different age groups present unique needs. Among these is the loss of temporal volume, recognized as an early sign of aging, although it can also occur in young adults with a low body fat percentage [1].
The temporal region, located lateral to the facial massif and the front-occipital region, is a transitional area prone to anatomical changes. Clinically, it exhibits features that facilitate the understanding of facial support loss and the inferior migration and separation of superficial fat compartments, contributing to the visible changes associated with aging. The area is characterized by a complex tissue stratigraphy determined by its anatomical components. Notably, prominent zygomatic bones and the zygomatic arch can exacerbate the hollowed appearance of the temples, giving rise to a more emaciated and aged look [2]. Studies such as that of [3] have noted that the layers of the temporal region are continuous with those of the scalp, and that a change in nomenclature occurs below the hairline. Anatomically, the region is medially delimited by the temporal crests (marking the boundary between the forehead and the temple) and inferiorly by the zygomatic arch. Consequently, there is an increasing need to minimize the risk of unintended complications and to maximize safety, making it imperative to deepen the understanding of the anatomy and clinically relevant variations.
Practitioners must maintain an updated morphological map of potential danger zones that may be encountered during facial surgical and minimally invasive procedures. The temporal region is sensitive and hosts vital neurovascular structures from a pathophysiological perspective, including the superficial temporal artery and, nearby, the temporofacial branch of the facial nerve (cranial nerve VII). In addition, the temporal fossae can become naturally depressed either as a sign of aging or as a result of intense physical activity, affecting eyebrow position and the overall facial contour. Topographically, the temporal region is based on the temporal fossa, formed by the parietal, frontal, sphenoid, and temporal bones. It is located lateral to the front-occipital zone, posterior to the orbital region, and superior to the parotidmasseteric area. According to several authors [3,4], the temporal fossae are bilateral, shallow depressions of the skullcap, bounded by the superior temporal line, the lateral orbital wall, the zygomatic arch inferiorly, and posteriorly by the hairline, where the skin is thicker and more vascularized.
This bony surface is covered by the periosteum, a membrane containing a varied number of vessels that form a rich anastomotic network of small arteries. Above the periosteum lie various soft tissue layers, including the temporal neurovascular tissues. Moreover, the stratigraphic constitution of the temporal region is highly complex, and recent studies confirm the intricacy of this morphological reality, which is increasingly essential to understand and consider during diagnosis and subsequent clinical procedures.
Proper identification of injection planes—subfascial, within the superficial temporal fat pad, or submuscular—is crucial to achieving safe and effective outcomes. A thorough understanding of the complex anatomy of the temporal area, including structures such as the superficial temporal artery, the temporal branch of the facial nerve, and the sentinel vein, helps minimize procedural risks and enhances treatment precision [5]. Referring to the work of [6], six distinct structural layers were identified in the anatomy of the temporal fossa, extending from the surface to its deeper regions:
Layer 1: Skin
The skin of the temporal region is thin, contains a large amount of dense connective tissue, and features the visible linear projection of the superficial temporal artery and vein [7].
Layer 2: Subcutaneous Tissue
Overlying the superficial fascial layer are the superior and inferior temporal fat compartments, as described by Velazco [8]. According to this study, the superior temporal compartment is located between the superior and inferior temporal septa and does not contain relevant neurovascular structures. In contrast, the inferior temporal compartment, situated between the inferior temporal septum and the adhesions of the zygomatic arch, contains the frontal branches of the facial nerve (motor), the zygomaticotemporal branches (sensory), and the temporal portion of the sentinel vein, as described in other investigations [9,10].
Layer 3: Superficial Fascia, also known as the Temporoparietal Fascia
The temporoparietal fascia, or superficial temporal fascia, is a connective tissue layer approximately 2 to 4 mm thick [11]. It lies directly beneath the subcutaneous fat of the temporal region, enveloping the superficial temporal vessels. It represents the cranial extension of the Superficial Musculoaponeurotic System (SMAS) [12], originating above the zygomatic arch and continuing along the cranial aponeurosis of the forehead and scalp. The investigation conducted by [13] provided a coherent description of the facial planes of the temple and midface. They dissected ten fresh hemifaces layer by layer to reveal the detailed facial anatomy of the midface and temporal regions.
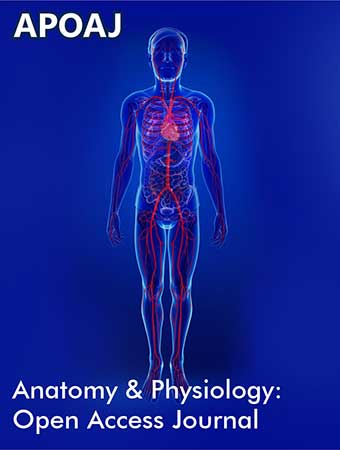
Their findings demonstrated that the temporoparietal fascia is an aponeurotic layer; beneath it lies the “loose connective tissue” or innominate fascia, which histologically retains its multilayered “loose areolar” structure, similar to that observed in the scalp. They also noted that this entity is highly vascularized, challenging previous suggestions that it constitutes an avascular subfascial space. An important study [14] further demonstrated that the superficial temporal fascia exhibits anisotropic properties. Researchers dissected the fascia of the deep temporal muscle (TMF). After removing the skin and subcutaneous fat, they reflected the TMF onto the internal surface of the fascia, revealing a striated pattern with zones formed by collagen fibrils extending longitudinally over greater distances. This indicated mechanical anisotropy of the tissue, characterized by regions with distinct collagen fibril alignment (Figure 1).
Layer 4: Loose Areolar Tissue
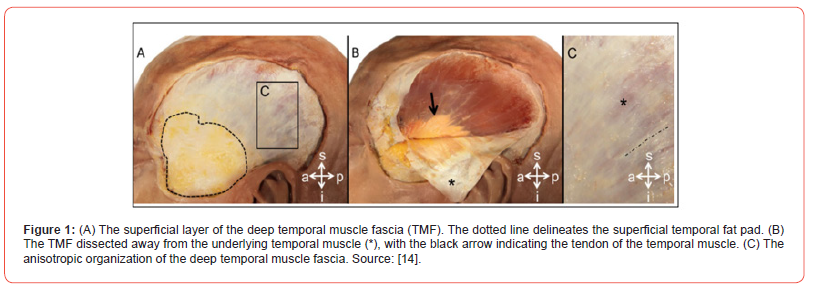
In reference to this layer, it can be generally stated that it is the most abundant of the non-specialized connective tissues. Its main characteristic is the absence of a structured organization, consisting of scattered cells embedded within an abundant extracellular matrix (Figure 2). The majority of the cellular population is represented by fibroblasts immersed in a rich extracellular matrix composed predominantly of collagen and elastin fibers, along with some reticular fibers. In addition, this layer contains blood vessels, nerve extensions, and the secretory components of exocrine glands, which play a fundamental role in tissue nutrition, as described by Megías et al. [15]. In the study conducted by Huang et al. [10], it was demonstrated that the layer of loose areolar tissue located between the superficial and deep temporal fasciae contained a sentinel vein and several perforating vessels but was otherwise predominantly avascular.
Layer 5: Deep Temporal Fascia
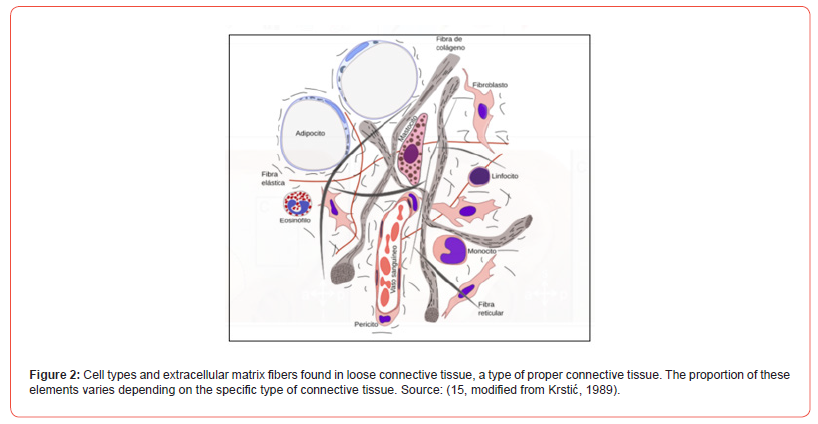
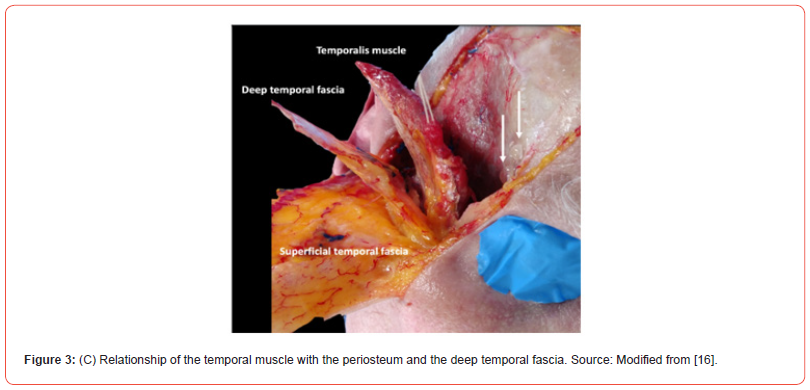
Several studies [7,8] have defined this fascial plane as a continuation of the cranial periosteum. It divides into two strongly adherent laminae on either side of the zygomatic arch. The superficial temporal fat pad occupies the space between these two laminae and contains the middle temporal vein [12]. In (Figure 3) the deep layer of the deep temporal fascia can be observed covering the deep temporal fat pad (the temporal extension of the buccal fat pad) and the temporal muscle [17], findings that have been corroborated by other studies [18].
Layer 6: Temporal Muscle
The temporal muscle is a masticatory muscle capable of generating significant contractile force. It has a fan-shaped structure and is located on the lateral surface of the skull within the temporal fossa. Its proximal attachment, or origin, is the inferior temporal line of the temporal fossa. From there, its tendinous portion passes beneath the zygomatic arch and inserts distally into the coronoid process of the mandible and the anterior margin of the mandibular ramus. Authors such as Cotofana et al. [19] also report that this muscle has additional insertions into the inferior portion of the deep temporal fascia and the posterior surface of the zygomatic process of the frontal bone. This muscle has its terminal insertion at the coronoid process of the mandible and maintains an important anatomical relationship with the anterior deep temporal artery and, at its midportion, with the posterior deep temporal artery. Given its extension, the muscle fibers are divided into three groups: anterior, middle, and posterior [20], each fulfilling a specific function.
The anterior fibers are involved in mandibular protrusion, the middle fibers serve an occlusive function, and the posterior fibers are responsible for mandibular retrusion (Figure 4). As a masticatory muscle, it is innervated by the anterior trunk of the mandibular nerve through its deep temporal branches. Its blood supply comes from the deep temporal branches of the maxillary artery and from the middle temporal branches of the superficial temporal artery.
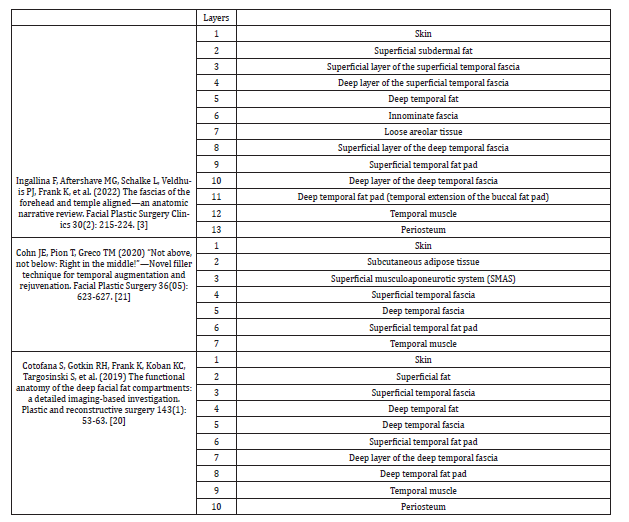
The different stratigraphic distributions of the temporal region are described in (Table 1), where it can be observed that authors such as Ingallina et al. [3], Cotofana et al. [16], and Cohn et al. [21] provide a more detailed integration of these tissue structures into a unified model. In the temporal region, the fat compartments play a crucial role in both facial aesthetics and in aesthetic medicine and maxillofacial surgery procedures. These compartments are key to maintaining the volume, shape, and support of the upper third of the face.
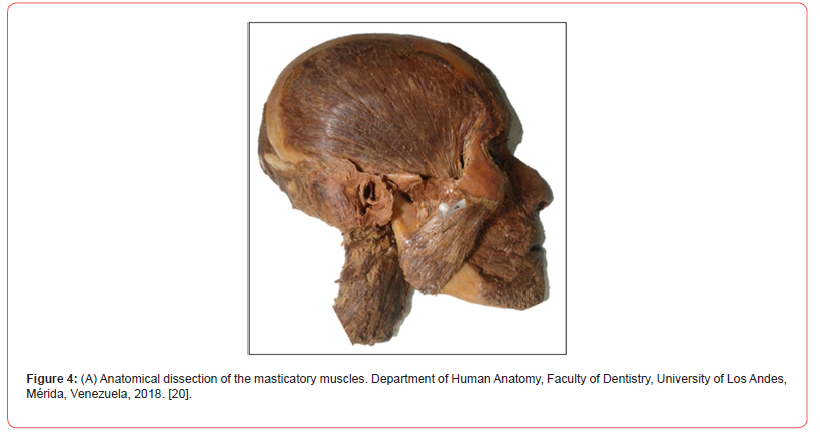
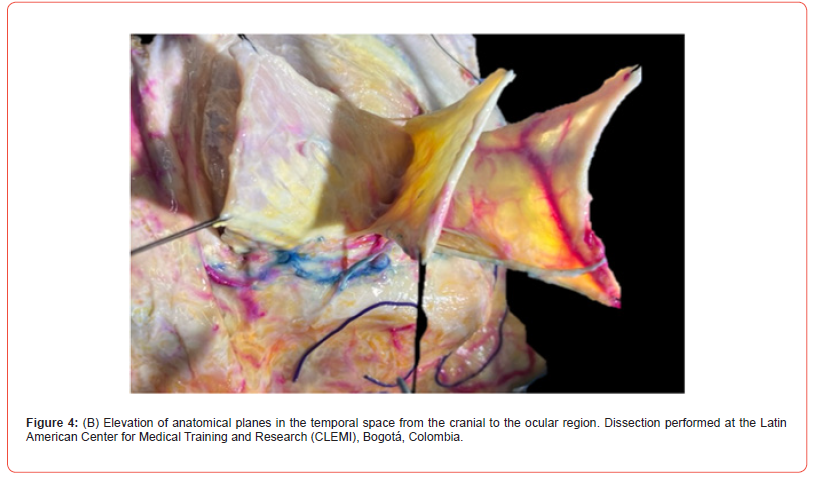
Table 1:Distribution of Tissue Layers in the Temporal Region as Described by Different Investigators.
Regarding the superficial temporal fat, it is located between the superficial temporal fascia and the superficial layer of the deep temporal fascia. Its function is to shape the transition between the regions interacting with the temporal area and to provide volume. It has a close anatomical relationship with the temporal branches of the facial nerve and the superficial temporal artery. Therefore, detailed knowledge of the anatomy of this area, as well as the correct clinical approach technique, is essential to avoid complications such as vascular embolism or nerve injury. Over time, this fat compartment tends to atrophy, leading to temporal hollowing, which represents a hallmark of aging, thus highlighting its aesthetic relevance. Authors such as Huang et al. [10] report that within the subcutaneous tissue layer, the inferior temporal septum divides the subcutaneous fat into two dynamic compartments: the Lateral Temporal Cheek Fat Compartment (LTFC) and the Lateral Orbital Fat Compartment (LOFC).
Their study aimed to investigate the temporal fat compartments and the relative neurovascular structures in cadavers. This research allowed the development of a safe and effective fat grafting technique for the augmentation of temporal hollowing. Eight cadavers (16 temporal regions) were dissected to analyse the tissue stratigraphy of the temporal area, including fat compartments, ligaments, and neurovascular structures. The results revealed the presence of two separate fat compartments in the subcutaneous layer: the lateral temporal-cheek fat compartment and the lateral orbital fat compartment. Additionally, two distinct compartments were identified in the loose areolar tissue layer: the superior temporal compartment and the inferior temporal compartment, separated by the inferior temporal septum. The presence of a sentinel vein and between one to six perforating vessels traversing the subcutaneous tissue and draining into the middle temporal vein was also observed.
This study concluded that there are four distinct fat compartments in the temporal region that are ideal for fat grafting and highlighted the importance of identifying a precautionary zone in the anterior half of the inferior temporal compartment. On the other hand, the deep temporal fat, located between the deep temporal fascia and the temporal muscle, is less accessible than the superficial fat. However, it facilitates gliding movements and provides cushioning to the temporal muscle during mandibular motions. Additionally, it contributes to the volume of the temporal region under study, and its loss can also lead to temporal hollowing. Authors such as Surek [22] have contributed research related to the anatomy of the intermediate temporal fat pad (ITFP) in connection with filler injection procedures. Using ultrasound technology for clinical localization in 20 fresh hemifacial cadavers, Surek demonstrated that anatomical terminology in the temporal region remains highly variable across the current body of literature.
His findings described the arrangement of three distinct
temporal fat pads: deep, intermediate, and superficial. The deep
temporal fat pad represents the temporal extension of the buccal
fat pad, while the intermediate temporal fat pad (ITFP) is located
between the superficial layer of the deep temporal fascia (S-DTF)
and the deep layer of the deep temporal fascia (D-DTF). The
temporal region is also a point of convergence for the sutures of the
frontal, sphenoid, parietal, and temporal bones. Therefore, areas
of bony instability exist where intracranial penetration may occur
[21]. In the application of facial aesthetic procedures, the temporal
region is crucial. Therefore, considering its innervation and
vascularization is of vital importance due to its clinical relevance.
This anatomical zone receives both sensory and motor innervation
[23] (verbal communication with Dr. Nancy Díaz de Villabona, Full
Professor of Human Anatomy, Faculty of Dentistry, University of Los
Andes, Mérida, Venezuela):
a) Sensory Innervation: It is provided by the fifth cranial
nerve, or trigeminal nerve, through the following branches:
b) Supraorbital nerve: Arising from the ophthalmic branch,
providing sensory innervation to the superior areas of the
temporal region.
c) Zygomaticotemporal nerve: A collateral sensory branch of
the maxillary nerve.
d) Auriculotemporal nerve: A branch of the posterior division
of the mandibular nerve, distributing sensory fibers to the
auricular skin, scalp, parotid gland, and the temporomandibular
joint complex.
Motor Innervation:
On one hand, the temporal branches of the facial nerve (seventh
cranial nerve) innervate the facial mimic muscles in the anterior
temporal region, including the lateral portion of the frontalis
muscle and the distal insertion of the orbicularis oculi muscle. On
the other hand, being a masticatory muscle, the three portions of
the temporal muscle receive innervation from the mandibular
nerve, the third branch of the trigeminal nerve, specifically from its
anterior division:
a) The posterior deep temporal nerve branches from the
temporomasseteric trunk.
b) The middle deep temporal nerve arises directly from the
anterior trunk.
c) The anterior deep temporal nerve branches from the
temporobuccal trunk along with the buccal nerve, this one
being sensory.
This innervation is highly relevant in botulinum toxin treatments aimed at controlling temporal hypertrophy associated with temporomandibular joint dysfunction (TMJ disorders) or bruxism, as well as for the treatment of dynamic rhytids in the frontotemporal region.
Vascularization of the Temporal Region:
The superficial temporal artery (a terminal branch of the external carotid artery) is the main arterial supply to the temporal region. It provides blood to the skin, muscles, and superficial tissues. Understanding its course is critical during procedures such as filler injections to avoid vascular complications such as embolism or necrosis. The middle and posterior deep temporal arteries, branches of the maxillary artery, supply the deep muscles such as the temporal muscle. The anterior deep temporal artery arises from the superficial temporal artery. Regarding venous drainage, the superficial temporal vein, which accompanies the superficial temporal artery, drains into the retromandibular vein. Based on the above, the primary objective of this study was to conduct a structural anatomical analysis of the temporal region, investigating the distribution of the various anatomical layers composing this area. The goal is to develop a reliable clinical concept that supports Temporal Contouring and the implementation of intelligent rejuvenation techniques, preserving the anatomo-clinical integrity of the temporal region.
Materials and Methods
A descriptive-analytical anatomical study was conducted at the Latin American Center for Medical Training and Research (CLEMI), Bogotá, Colombia. A total of 30 hemifaces corresponding to 15 fresh cadavers were dissected between November 2024 and December 2024. Magnifying loupes with 30x magnification were used, and a layer-by-layer dissection technique was performed using a medial design, extended from the cranial to the ocular region. The dissection preserved the layers of the lateral canthal ligament and maintained planar integrity throughout the procedure. The anatomical planes were carefully elevated, exposed for observation, and subsequently analyzed and photographed. Black 3-0 silk sutures were used for tissue fixation and marking, as shown in Figure 4. Once the superficial anatomical boundaries were established, and after incising the skin and dissecting the subcutaneous tissue, the superficial musculoaponeurotic system (SMAS) was identified.
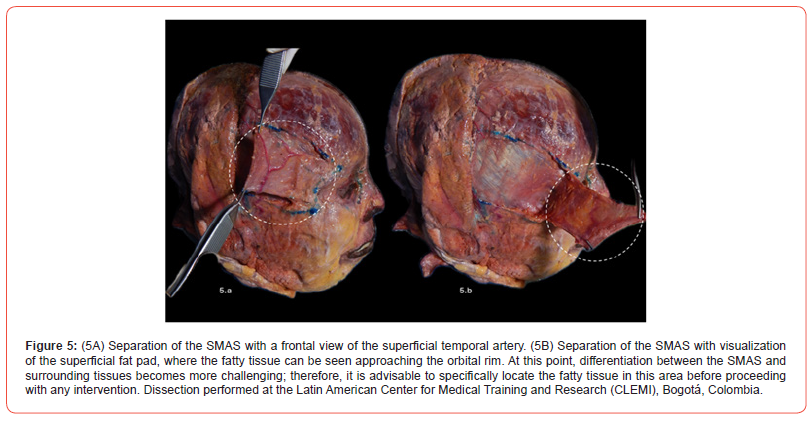
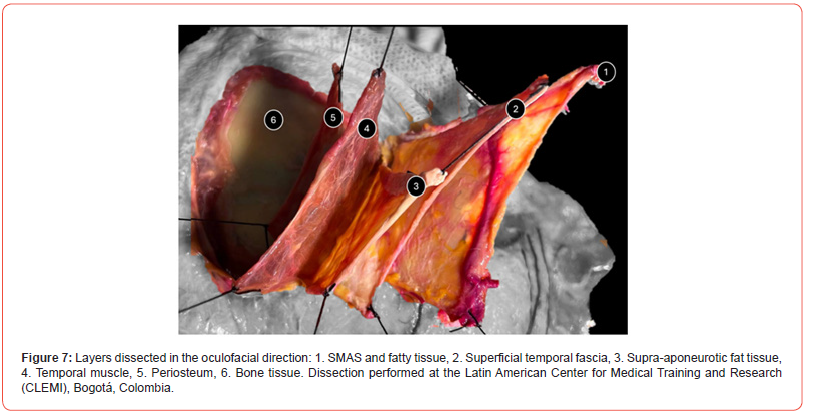
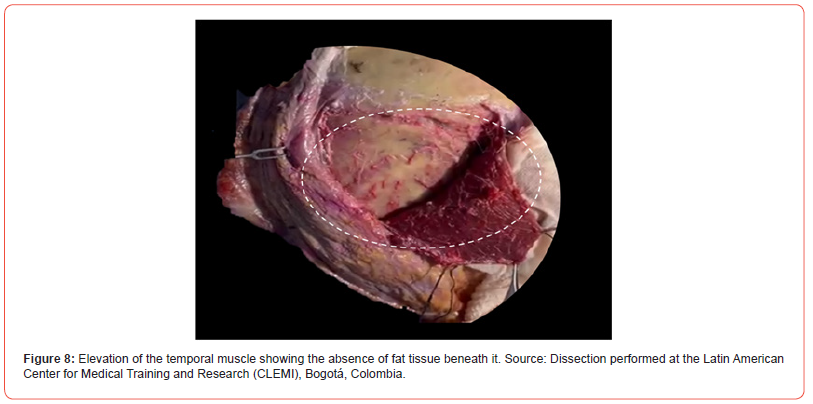
The SMAS is defined as a fibroelastic structure that continues uninterruptedly with the galea aponeurotica superiorly and with the superficial cervical fascia and the platysma muscle inferiorly. It has a superficial relationship with the tissues near the orbital rim, extending anteriorly and superiorly in its course to reach the medial aspect of the frontalis muscle, passing posterior to the lateral orbital rim, as shown in (Figure 5). On (Figure 6) The superior temporal septum is observed, completely surrounded by fatty tissue extending both laterally and centrally relative to the septum. A total of six layers were dissected, confirming that the deep fat pad is not located directly over the bone, but rather over the aponeurosis of the temporal muscle (Figure 7). In all the dissected anatomical specimens, it was evident that the deep fat tissue is not located beneath the muscle, but rather lies in a supraaponeurotic position (Figure 8)..

Results
In the thirty dissected hemifaces, the presence of three fat compartments was evidenced: one located beneath the skin, one beneath the SMAS, and a deep one situated over the aponeurosis of the temporal muscle. This finding demonstrates that fat tissue distribution within the temporal fossa differs from that observed in other facial regions. Understanding the anatomy of these compartments highlights the importance of accurately locating them, particularly when performing procedures such as facial adipo-structuring, where precise knowledge of fat compartment positioning is absolutely essential.
Discussion
Given the biological and functional complexity of the temporal region, a thorough morpho functional understanding of the different layers that compose it is essential to optimize safety and efficacy in clinical practice. Anatomical dissection remains a key method to confirm the critical importance of this knowledge.
Currently, there is an increasing demand for anatomical studies based on dissection, focused on identifying anatomical entities that rigorously support clinical approaches, with temporal contouring procedures being one such area. The review and bibliographic analysis regarding the morpho-stratigraphy of the temporal region and its application in temporal contouring procedures confirm anatomical findings that are both consistent with and divergent from those obtained in the present study, emphasizing the importance of an evidence-based morpho-stratigraphic approach. From a stratigraphic perspective, the results obtained in the present investigation are consistent with those reported by Cohn et al. [21], who stated that the soft tissues of the temporal region are distributed in parallel stratified layers that vary in thickness depending on age-related influences. This observation is supported by other studies [23], which report that although each anatomical layer undergoes its own aging process, there is also a dependency between superficial and deeper entities.
This suggests that aging is a multifaceted and complex process, where even minimal changes occurring in one layer can often trigger a cascade of changes in adjacent layers. The evidence of three distinct temporal fat compartments, located respectively beneath the skin, beneath the SMAS, and over the aponeurosis of the temporal muscle, demonstrates that fat distribution within the temporal fossa differs from that of other facial anatomical units [24]. In particular, the deepest compartment identified in the dissections performed in this study coincides with descriptions by Ingallina et al. [3], Cotofana et al. [16], Contreras [18], and Kyu-Ho Yi et al. [25]. These authors describe a deep temporal fat pad representing the temporal extension of the buccal fat compartment. It is clear that the deep fat compartments are situated between the two layers of the deep temporal fascia, covering the temporal muscle. Moreover, this deep fat extension contributes to the stabilization of the underlying skeletal and muscular structures, preserving overall facial balance [25].
Conclusion
The anatomical study conducted in this investigation provides a comprehensive description of the anatomy of the temporal region, including the bony relationships regarding the insertion of the temporal muscle, the fascial layers that define a clear stratigraphy, the fat and dermal tissue entities, and the neurovascular elements present in the area. The findings demonstrate that the temporal region is one of the few facial areas where deep fat is not located beneath the musculature, as is commonly reported, but rather over the aponeurosis of the temporal muscle. This significantly impacts the precise placement of biomaterials in this area.
These findings provide a solid explanation of the morphological characteristics that must be considered when performing anatomoclinical approaches, emphasizing the importance of identifying risk zones and establishing the anatomical foundation for the development of future techniques aimed at rejuvenating the studied area. As is well known, age-related changes lead to a loss of volume in this region, resulting in a concavity of the temporal fossa—a stigmatizing sign of subcutaneous tissue aging—that causes the face to appear tired and aged. This has a profound impact on overall facial harmony, a key goal of clinical disciplines that seek to restore balanced proportions and achieve natural facial rejuvenation.
- Buckingham ED, Glasgold R, Kontis T, Smith SP Jr, Dolev Y, et al. (2015) Volume rejuvenation of the facial upper third. Facial Plast Surg 31(1): 43-54.
- Breithaupt AD, Jones DH, Braz A, Narins R, Weinkle S (2015) Anatomical basis for safe and effective volumization of the temple. Dermatol Surg 41(Suppl 1): S278-S283.
- Ingallina F, Alfertshofer MG, Schalke L, Veldhuis PJ, Frank K, et al. (2022) The fascias of the forehead and temple aligned—an anatomic narrative review. Facial Plast Surg Clin North Am 30(2): 215-224.
- De Almeida AR, de Araújo Sampaio GÂ, Queiroz NP (2017) Hyaluronic acid in the rejuvenation of the upper third of the face: review and update. Part 2: temporal and supraorbital regions. Surgical Cosmetic Dermatology 9(2): 113-121.
- Hong GW, Wan J, Choi W, Yi KH (2025) An expert guide to anatomy-based filler injection for the temple: techniques and clinical insights. Life (Basel) 15(2): 266.
- Sykes JM, Riedler KL, Cotofana S, Palhazi P. (2020) Superficial and deep facial anatomy and its implications for rhytidectomy. Facial Plast Surg Clin North Am 28(3): 243-251.
- Tamura BM (2010) Facial anatomy and the application of fillers and botulinum toxin- Part II. Surgical Cosmetic Dermatology 2(3): 195-204.
- Velazco G (2020) Adipoestructuración facial. Acta Bioclínica 10(20): 25-46.
- Moss CJ, Mendelson BC, Taylor GI (2000) Surgical anatomy of the ligamentous attachments in the temple and periorbital regions. Plast Reconstr Surg 105(4): 1475-1490.
- Huang RL, Xie Y, Wang W, Herrler T, Zhou J, et al. (2017) Anatomical study of temporal fat compartments and its clinical application for temporal fat grafting. Aesthet Surg J 37(8): 855-862.
- Demirdover C, Sahin B, Vayvada H, Oztan HY (2011) The versatile use of temporoparietal fascial flap. Int J Med Sci 8(5): 362-368.
- Bae JH, Park SY, Yi KH (2024) Consideration of the diameter of superficial temporal arteries related to filler injections in the temporal region. Skin Res Technol 30(4): e13674.
- De Vasconcellos JA, Britto JA, Henin D, Vacher C (2003) The fascial planes of the temple and face: an en-bloc anatomical study and a plea for consistency. Br J Plast Surg 56(7): 623-629.
- Zwirner J, Ondruschka B, Scholze M, Schulze-Tanzil G, Hammer N (2021) Biomechanical characterization of human temporal muscle fascia in uniaxial tensile tests for graft purposes in duraplasty. Scientific Reports 11(1): 2127.
- Megías M, Molist P, Pombal MA. Atlas de histología vegetal y animal.
- Cotofana S, Gaete A, Hernandez CA, Casabona G, Bay S, et al. (2020) The six different injection techniques for the temple relevant for soft tissue filler augmentation procedures – Clinical anatomy and danger zones. J Cosmet Dermatol 19(7): 1570-1579.
- Watanabe K, Shoja MM, Loukas M, Tubbs RS (2016) Soft tissue of the scalp and temporal regions. In: Anatomy for Plastic Surgery of the Face, Head, and Neck.
- Contreras Alvarado EA, Theriot Giron MDC, Quiroga Garcia MA, Hernandez Juarez J (2018) Estudio cadavérico de la región temporal. Rev Mex Estomatol 5(1): 3-8.
- Cotofana S, Gotkin RH, Frank K, Koban KC, Targosinski S, et al. (2019) The functional anatomy of the deep facial fat compartments: a detailed imaging-based investigation. Plast Reconstr Surg 143(1): 53-63.
- (2018) Anatomical dissection. Department of Human Anatomy, Faculty of Dentistry, University of Los Andes, Mérida, Venezuela.
- Cohn JE, Pion T, Greco TM (2020) “Not Above, Not Below: Right in the Middle!”-Novel filler technique for temporal augmentation and rejuvenation. Facial Plast Surg 36(5): 623-627.
- Surek CC (2021) A new target for temple volumization? An anatomical and ultrasound-guided study of the intermediate temporal fat pad. Aesthetic Surg J 41(12): 1339-1343.
- Verbal communication with Dr. Nancy Díaz de Villabona, Full Professor of Human Anatomy, Faculty of Dentistry, University of Los Andes, Mérida, Venezuela.
- Swift A, Liew S, Weinkle S, Garcia JK, Silberberg MB (2021) The facial aging process from the “inside out”. Aesthet Surg J 41(10): 1107-1119.
- Yi KH, Wan J, Kim SB, Kim HJ (2025) Temporal fat pad filler injection for lifting purposes: shifting of the superficial layer of deep temporal fascia. J Cosmet Dermatol 24(3): e70023.
-
Gladys Velazco Viloira*, Nancy Diaz de Villabona, Said Rodea Hernandez, Victor Mercado and Marta Amin Merino. Layered Morphological Perspective of The Temporal Region and Its Relevance in Temporal Contouring Procedures. Anat & Physiol Open Access J. 1(5): 2025. APOAJ.MS.ID.000525.
- Fascia; temporal fossa; temporal adipose tissue; temporal stratigraphy; iris publishers; iris publisher’s groupFrontal, Sinuses, Agenesis, Pneumatization, Prevalence, Cadavers, Embryology, Surgery, Symptoms, Sinusitis
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.