 Case Report
Case Report
Oral Findings in Liver Transplanted Children with a History of a Congenital Liver Disease: A Report of Two Cases
Ezzina Khouloud, Elelmi Yamina*, Cherni Souha, Ghedira Hichem and Ben Khelifa Mohamed
Department of Pediatric Dentistry, Faculty of Dental medicine, Monastir, Tunisia
Elelmi Yamina, Department of Pediatric Dentistry, Faculty of Dental medicine, Monastir, Tunisia.
Received Date:February 08, 2021; Published Date: March 09, 2021
Abstract
Medical progress leads us to take care of new types of patients, including those who have been liver transplanted. In fact, the number of these patients is constantly increasing, hence the probability of meeting them in the dental office is increasing. These patients require specific, personalized and rigorous dental management, due to the infectious risk and therapeutic risk associated with immunosuppressive medication, along with specific side effects of immunosuppressants. Other oral manifestations associated with the previous liver disease, have been reported. The aim of this paper was to describe the oral findings in liver transplanted children through two cases.
Keywords: Enamel hypoplasia; Liver disease; Liver transplantation; Tooth discoloration
Introduction
Liver transplantation is the treatment of choice for acute liver failure, chronic liver failure, metabolic liver disease and malignancy [1]. Earlier diagnosis, improved patient selection and operative techniques, and successful development of immunosuppressive agents, had led to an increase number of liver transplanted patients. To overcome the shortage of child donors, reduction hepatectomies is usually indicated. It is a procedure in which part of a living adult liver is cut down to fit a child [1,2]. Children with liver transplant require careful dental management due to the infectious risk and therapeutic risk associated with immunosuppressive medication, along with specific side effects of immunosuppressants [3,4]. So far, research has largely been confined to the effects of immunosuppressive medication on oral mucosa and gingival tissues. Other possible oral manifestations associated with the previous liver disease have not been largely investigated. The aim of this paper was to report on delayed eruption of teeth, enamel hypoplasia and greenish intrinsic staining of teeth, in two children with the same medical history, who received orthotopic liver transplants.
Cases presentation
First case
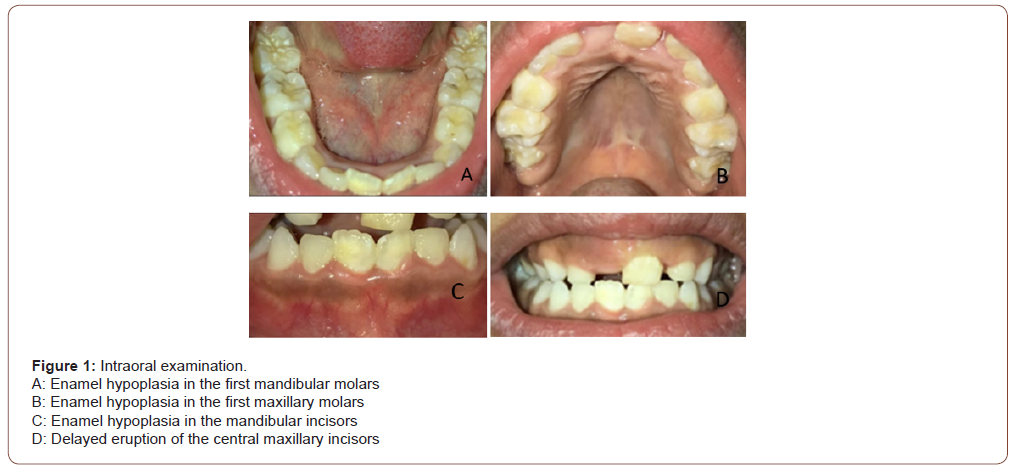
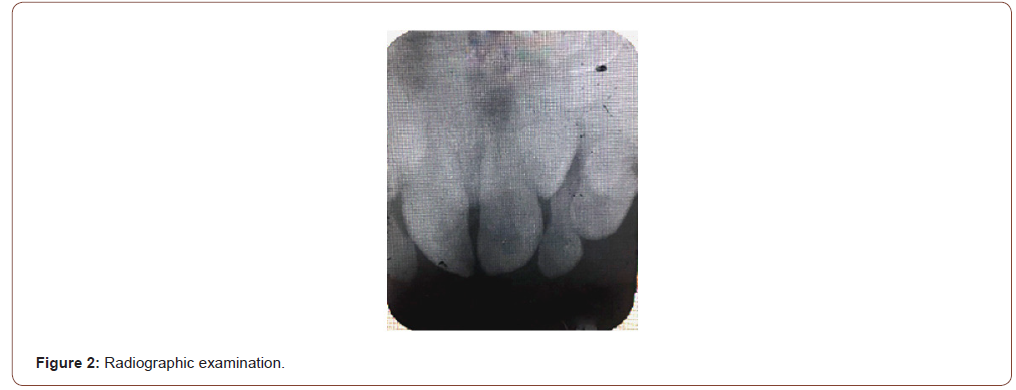
nine-year-old female patient was referred to the Dental Department of Fattouma Bourguiba Hospital of Monastir, Tunisia for a dental check-up. She had a history of progressive familial intrahepatic cholestasis diagnosed at the age of three years. She underwent an orthotopic liver transplant of a hemi-liver, taken from her mother, six months before the dental check-up. The patient is taking Tacrolimus as immunosuppressive medication. Clinical examination of the oral mucosa and the teeth showed a delay of the eruption of the central maxillary incisors (Figure 1D) and enamel hypoplasia in the mandibular incisors and first molars (Figures 1 A, B, C). Radiographic examination (intraoral periapical radiograph) showed the presence of the central maxillary incisors. The periapical radiograph also showed that 2/3 of the roots of 11 and 21 were formed, and the absence of an obstacle preventing the spontaneous eruption of the teeth (Figure 2).
Second case
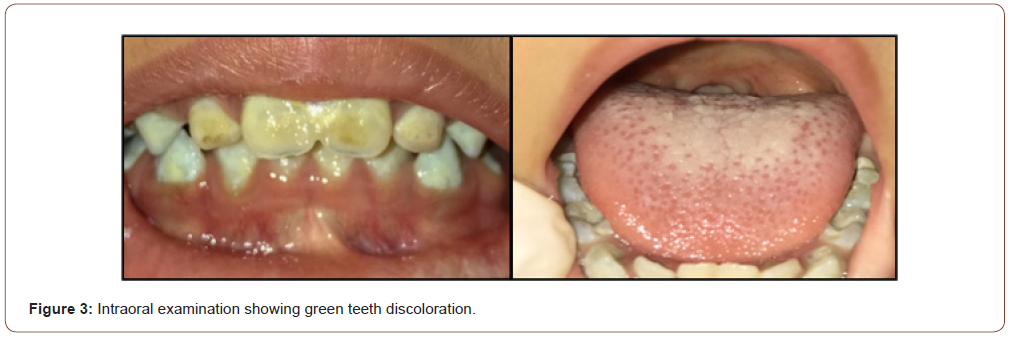
A two-year-old female patient was referred to the Dental Department of Fattouma Bourguiba Hospital for a dental check-up. She had a history of progressive familial intrahepatic cholestasis diagnosed at the age of two months. She underwent an orthotopic liver transplant of a hemi-liver, taken from her father, six months before the dental check-up. The patient is taking Tacrolimus as immunosuppressive medication. The clinical examination showed a green pigmentation of the maxillary incisors and the molars (Figure 3). The patient was non-cooperative. Therefore, retractors couldn’t be used to take pictures.
Discussion
Nutritional deficiencies in vitamin A and vitamin D are among the most frequent systemic causes of delayed eruption of the permanent dentition. Fat-soluble vitamin A is present in food of animal origin as retinol and in plants as carotene. This vitamin is involved in the growth of bones. Its deficiency leads to impaired bone growth, which can lead to delayed eruption of permanent teeth. Vitamin D deficiency leads to poor calcification of the bones. Therefore, the bone loses its rigidity and becomes deformed. This leads to stunted growth and abnormalities in the dentition including hypoplastic enamel and eruption disorders [5]. Since the liver has a role of absorption and storage of vitamin A, and an activating role of vitamin D, [6] liver disease from which the patient was affected before receiving a liver transplant, may be the cause of this delay of central maxillary incisors eruption, in the first case [1,7]. Parents should be reassured that delayed eruption of the primary or permanent dentition may sometimes occur, but these teeth do erupt eventually and often without recourse to surgical intervention.
In addition, it is recommended to monitorize the development of the dentition, and to perform a thorough clinical and radiographic examination, in order to make sure of the absence of an obstacle preventing the spontaneous eruption of teeth.
Enamel hypoplasia is a quantitative defect of enamel, visually and morphologically identified as involving the surface of the enamel and associated with a reduced thickness. It can be hereditary or acquired and can be associated with numerous systemic disorders and low birth weight [8]. Studies have also shown that enamel hypoplasia is more common in children with chronic liver disease compared to healthy children. This is due to the malnutrition often seen in patients with liver problems, since the liver plays a role in storage of mineral, salts and vitamins, participates in digestion and absorption of nutrients and fat-soluble vitamins, and is the seat of protein synthesis [9,10].
A study conducted by Dorota Olczak-Kowalczyk, et al. in 2014, showed frequent dental defects such as opacities and hypoplasia (25.7% of the subjects) in children and adolescents with liver failure [11]. Another study by Hosey et al. reported enamel defects in 6 out of 55 subjects with liver failure [1]. Wondimu et al. reported enamel hypoplasia in 36% and enamel opacities in 76% of pediatric liver recipients [2]. Enamel hypoplasia provides a nest for bacteria. Surface irregularities due to this pathology can promote the retention of dental plaque and decrease the clearance of carbohydrates. Therefore, restoration of teeth with enamel hypoplasia by composite resin protects them against decay [10]. Teeth discoloration is due to the excess of conjugated bilirubin in the blood, due to the cholestatic disease the patient suffered from before the transplant, which causes its accumulation in the tissues [8,11,12,13]. In fact, hyperbilirubinaemia (> 2.5 mg/dl) is associated with a yellowish discoloration of the mucous membrane, skin. Partial bilirubin oxydation in blood may produce a darker tissue discoloration (greenish brown or yellowish brown) [11].
In children, since enamel is not mineralized yet, the discoloration may appear on the teeth, giving them a shade ranging from yellowish to greenish. This pigmentation can also affect temporary teeth in children with congenital cholestatic disease [11,12]. These stains in the teeth are not seen in adults who develop liver disease after tooth enamel has already been calcified [11]. Wondimu et al. reported greenish discoloration of the teeth in 50% of pediatric liver recipients with a medical history of hyperbilirubinaemia biliary atresia [2]. Unlike pigmentations on the skin and mucous membranes which disappear after the treatment of the liver disease, the teeth pigmentations do not disappear, because the dental tissues lose their metabolic activities and their ability to lose the pigment, once the tooth development is completed [11]. The purpose of the treatment of these green colorations is purely aesthetic. It will allow the patient to regain self-confidence. It important to know that teeth whitening is not effective when the pigmentation is confined to the dentin [8]. Therefore, the treatment of choice for the aesthetic rehabilitation of permanent teeth is the fixed prosthesis: veneers or full recovery crowns. For children, temporizing using composite restorations is advised to camouflage the green stains. For temporary teeth, composite resin can also be used to hide the green pigmentation [8,12].
Parents of liver transplanted children should be forewarned earlier of the likelihood of a delayed teeth eruption, enamel hypoplasia and intrinsic green staining of teeth due to liver disease, in order to allay their concerns. They should also be reassured that there are techniques available to improve their dental health and their smile. Recipients of liver transplants are constantly increasing and are becoming younger. Therefore, dentists will increasingly be needed to treat these patients.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- MT Hosey, G Gordon, DA Kelly, L Shaw (1995) Oral findings in children with liver transplants. Int J Paediatr Dent 5(1): 29-34.
- Wondimu B, Németh A, Modéer T (2001) Oral health in liver transplant children administered cyclosporin A or tacrolimus. Int J Paediatr Dent 11(6): 424-429.
- Lins L, Bastos J (2014) Oral health protocol for liver transplant patients. Transpl Technol 2(2):1-8.
- Byron RJ, Osborne PD (2005) Dental management of liver transplant patients. Gen Dent 53(1): 66-69.
- Castaneda B, Choukroune C (2016) Alterations of the eruption of permanent molars. Rev Odont Stomat 45:180-206.
- (2014) College of Universities in Hepato Gastro Enterology (CDUHGE) Liver-biliary tract. In: Collegiate University of Hepatogastroenterology (CDU-HGE), (edn.), The fundamentals of digestive pathology. Paris: Elsevier Masson, pp. 1-39.
- Hala Abu Botain, Rita Khounganian (2013) Dental management of a patient with progressive familial intrahepatic cholestasis. King Saud University Journal of dental sciences 4: 37-45.
- Kelly, Deirdre A (2017) Dental Care of Children with Liver Disease. Diseases of the Liver and Biliary System in Children 405-412.
- Masterson EE, Fitzpatrick AL, Enquobahrie DA, Mancl LA, Conde E, et al. (2017) Malnutrition-related early childhood exposures and enamel defects in the permanent dentition: A longitudinal study from the Bolivian Amazon. Am J Phys Anthropol 164(2): 416-423.
- Baygin O, Cakir M, Ucuncu N (2017) Oral and dental health in children with chronic liver disease in the Turkey Northeast. Niger J Clin Pract 20(9): 1182-1188.
- Olczak Kowalczyk D, Kowalczyk W, Krasuska Sławińska E, Dądalski M, Kostewicz K, et al. (2014) Oral health and liver function in children and adolescents with cirrhosis of the liver. Prz Gastroenterol 9(1): 24-31.
- Guimarães LP, Silva TA (2003) Green teeth associated with cholestasis caused by sepsis: a case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 95(4): 446-451.
- Barbério GS, Zingra ACG, Santos PSS, Machado MA (2018) Green Teeth Related to Bilirubin Levels. Acta Stomatol Croat 52(1): 61-64.
-
Ezzina Khouloud, Elelmi Yamina*, Cherni Souha, Ghedira Hichem, Ben Khelifa Mohamed. Oral Findings in Liver Transplanted Children with a History of a Congenital Liver Disease: A Report of Two Cases. Annal of Pub Health & Epidemiol. 1(3): 2021. APHE.MS.ID.000513.
-
Enamel hypoplasia, Liver disease, Liver transplantation, Tooth discoloration, Acute liver failure, Eruption disorders, Immunosuppressive agents.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






