 Research Article
Research Article
Dynamics and Epidemiological Characteristics of COVID-19 Epidemic Waves in the Republic of Congo, March 2020 to October 2022
Gilbert NDZIESSI*, Ange Clauvel NIAMA, Jys Ryschel NGOYOMI-ALIST and Jethro MASSALA
Faculty of Health Sciences, Public Health Program, Marien Ngouabi University, Brazzaville, Republic of Congo
Gilbert Ndziessi, Faculty of Health Sciences, Public Health Program, Marien Ngouabi University, Brazzaville, Republic of Congo
Received Date:September 01, 2025; Published Date:September 09, 2025
Abstract
Background: The COVID-19 pandemic presented a significant challenge to public health systems worldwide, particularly in low- and middleincome
countries like the Republic of Congo. This study analyzes the temporal dynamics and epidemiological characteristics of COVID-19 epidemic
waves in Congo from March 2020 to October 2022.
Methods: Data were sourced from the national CIRCOV database, covering all confirmed COVID-19 cases, testing, and vaccination records.
Descriptive and temporal analyses were conducted to characterize epidemic waves, case distribution by age, sex, and location, and to assess mortality
patterns.
Results: A total of 24,775 confirmed COVID-19 cases were reported from 446,034 tests (positivity rate: 5.5%). Four distinct epidemic waves
were identified, varying in duration and intensity, with an average interval of 8.75 weeks between waves. The majority of cases occurred among
individuals aged 20–59, with men representing two-thirds of cases. The overall recovery rate was 96.9%, while the case fatality rate was 1.6%, higher
among older adults and males. Brazzaville and Pointe-Noire accounted for most cases nationally.
Conclusion: The study highlights the recurrent and variable nature of epidemic waves in Congo, influenced by viral transmission dynamics
and public health interventions. Strengthening surveillance systems, decentralizing healthcare services, and improving epidemic preparedness are
essential for responding to future health crises..
Keywords:SARS-CoV-2 transmission dynamics; Epidemic wave characterization; Case fatality rate stratification; Public health surveillance systems
Introduction
The occurrence of epidemics or pandemics rarely adheres to a predictable scientific framework. Outbreaks may arise suddenly, marked by a rapid increase in cases of a known pathogen such as measles or an emergent infectious agent, exemplified by the COVID-19 pandemic. Established infectious diseases benefit from comprehensive epidemiological data and validated response protocols. However, emerging pathogens introduce significant uncertainties related to transmission dynamics, pathogenicity, and the effectiveness of control measures, which pose substantial challenges to public health infrastructures [1,2].
Epidemiological patterns of infectious diseases often manifest as waves or discrete outbreaks, characterized by sharp rises in incidence over short periods. Such fluctuations are influenced by multiple factors, including adherence to non-pharmaceutical interventions, population density, mobility patterns, and viral evolution especially the emergence of variants with altered transmissibility or immune escape capabilities [3-5]. Seroprevalence studies conducted in Central Africa from 2020 to 2024 reveal SARSCoV- 2 circulation levels substantially exceeding those suggested by official case detection, highlighting underdiagnosis linked to healthcare access disparities and testing limitations [6,7].
Prior to the introduction of COVID-19, the Republic of Congo’s healthcare system exhibited structural vulnerabilities common to many low- and middle-income countries. These included insufficient healthcare infrastructure, particularly in rural zones; limited human resources; and a health financing model heavily reliant on external aid [8]. Laboratory diagnostic capacities and epidemiological surveillance were predominantly centralized in urban centers such as Brazzaville and Pointe-Noire, limiting realtime outbreak detection and response in decentralized regions. The absence of a robust, integrated health information system further constrained effective epidemic management and datadriven decision-making. The COVID-19 pandemic has exposed and exacerbated these systemic weaknesses, emphasizing the critical need for strengthening surveillance mechanisms, expanding laboratory network capacities, enhancing data integration platforms, and decentralizing healthcare delivery [9,10].
This study aims to evaluate the temporal and spatial dynamics of COVID-19 within the Republic of Congo, alongside an assessment of public health response strategies including testing, contact tracing, and vaccination campaigns. By characterizing the epidemic waves, analyzing sociodemographic profiles of cases and fatalities, and identifying gaps in surveillance and control measures, this research intends to provide evidence-based recommendations to improve preparedness and inform future epidemic management efforts in the country [11].
Methods
Data Source
The data used in this study were obtained from the national CIRCOV database (Integrated COVID-19 Response Center), which serves as the official repository for epidemiological surveillance of the COVID-19 pandemic in the Republic of Congo. Established at the onset of the health crisis, this database centralizes, harmonizes, and facilitates the management of COVID-19 related information.
Data are updated daily through an extensive network of
healthcare actors nationwide, including:
a. Accredited medical biology laboratories, responsible for
conducting diagnostic tests (PCR, antigen tests) and reporting
results for both positive and negative cases;
b. Screening centers, which collect samples, monitor suspected
cases, and promptly report test results to the central system;
c. Vaccination centers, tasked with recording vaccination data,
including vaccine type, number of doses administered, and
sociodemographic characteristics of vaccinated individuals.
All records within CIRCOV are anonymized to ensure confidentiality and protect individual privacy. Each entry corresponds to a unique individual and includes key clinical information (presence or absence of symptoms, symptom onset date, disease progression, vaccination status) as well as sociodemographic data (age, sex, place of residence). This detailed data granularity enables in-depth analyses of epidemiological trends, vaccination impact, and affected population profiles.
Centralizing these data within CIRCOV not only facilitates realtime monitoring of the pandemic but also supports coordinated national health responses, production of epidemiological reports, and data-driven decision-making. For this study, all available data from March 14, 2020, the date of the first confirmed COVID-19 case in Congo to October 14, 2022, when the government officially declared the end of the epidemic, were extracted and analysed.
Variables
The variables analysed included:
• Age (in years)
• Sex (male/female)
• Geographic location (department or district)
• Date of case confirmation (date of positive test)
• Symptomatology (presence or absence of clinical signs)
• Vaccination status (vaccinated or unvaccinated)
Statistical analysis
Data from the CIRCOV database underwent rigorous processing
to ensure quality and relevance for epidemiological analysis. The
entire dataset was imported and managed using Microsoft Excel
2010, facilitating data structuring and preparation for statistical
analysis. To optimize temporal trend analysis, pivot tables were
created to aggregate confirmed cases at two main temporal
resolutions:
a. By epidemiological week: This weekly granularity
enabled the detection of short-term fluctuations, such as rapid
outbreak onset or epidemic peaks.
b. By month: Monthly aggregation provided a broader view
of longer-term trends, offering a more stable overview of pandemic
progression.
These temporal aggregations allowed graphical representation of the COVID-19 epidemic evolution at the national level, highlighting periods of case increase or decrease. Such visualizations were essential for identifying epidemic cycles and better understanding the disease dynamics within the country. Moreover, these processed data formed the basis for more advanced statistical analyses aimed at exploring epidemic determinants and assessing the impact of implemented public health interventions.
Identification of epidemic waves
An epidemic wave was defined as a rapid and significant
increase in case numbers over a specific period, deviating from
the previous trend. For each wave, the interval between waves the
time elapsed since the end of the previous wave was calculated.
The average time between two epidemic waves (AT) was estimated
using the following formula:
AT = (Sum of outbreak delays) / (Number of outbreaks)
Results
Overall situation of the COVID-19 epidemic in Congo
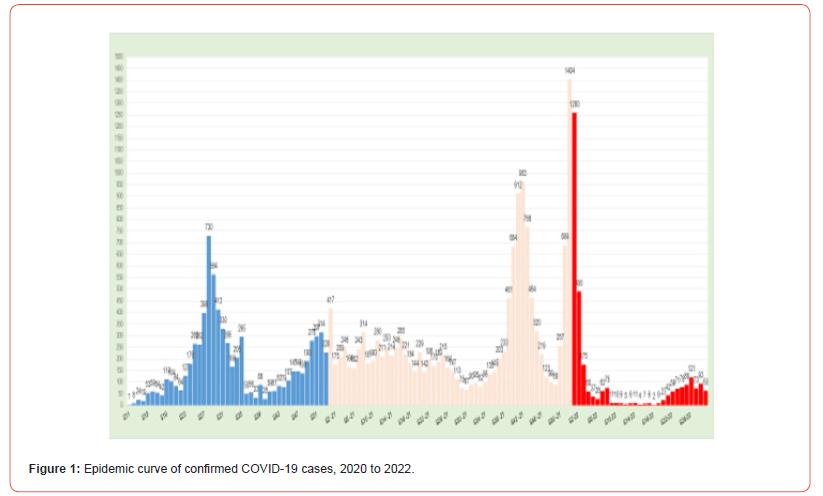
From March 14, 2020, to October 14, 2022, a total of 446,034 RT-PCR and antigen tests were conducted, resulting in 24,775 confirmed COVID-19 cases, corresponding to an overall positivity rate of 5.5%. The epidemic curve of confirmed cases highlights several successive waves during this period. The first wave, shown in blue, peaked sharply between weeks 27 and 31 of 2020, with weekly case numbers exceeding 700. The second wave, depicted in beige, primarily spanned the entirety of 2021, from week 1 to week 52, characterized by a gradual increase culminating around week 42. The third wave, illustrated in red, was the most intense, with an exceptionally high peak of 1,404 confirmed cases in a single week at the beginning of 2022. Following this peak, a marked decline in case numbers was observed. This epidemic progression reflects both the impact of various circulating viral variants and the effects of implemented control measures and successive vaccination campaigns (Figure 1).
Evolution of the positivity rate in Congo
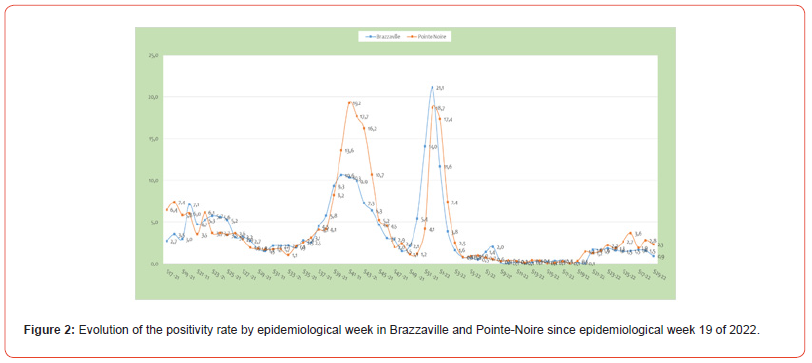
Figure 2 below illustrates the weekly progression of the overall positivity rate since epidemiological week 13 of 2020. The positivity rate has remained relatively stable over several epidemiological weeks at the national level, albeit with slight fluctuations.
Evolution of the positivity rate in Brazzaville and Pointe- Noire
Figure 2 highlights the weekly variations in the positivity rate within the departments of Brazzaville and Pointe-Noire. Since epidemiological week 19 of 2022, there has been a noticeable resurgence in the positivity rate, characterized by a fluctuating, sawtooth pattern.
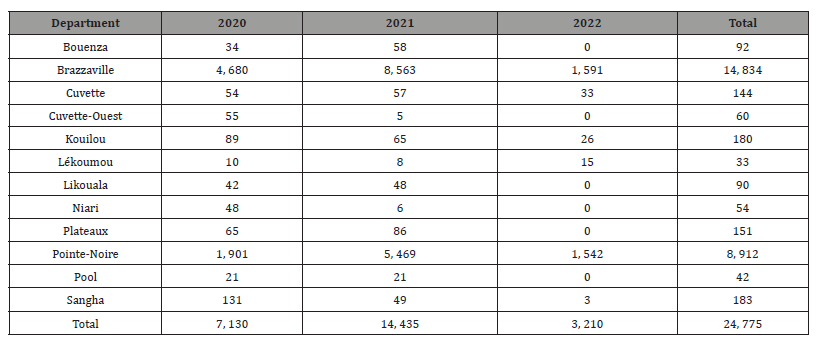
Monthly evolution of the epidemic by department
As shown in Table 1, between 2020 and 2022, a total of 24,775 COVID-19 cases were reported across the departments of the Republic of Congo. Brazzaville recorded the highest number of cases with 14,834, followed by Pointe-Noire with 8,912 cases. Other departments reported significantly fewer cases, notably Kouilou and Sangha with 180 and 183 cases, respectively. Several departments such as Bouenza, Cuvette, Likouala, and Plateaux recorded between 90 and 151 cases, while Lékoumou, Niari, and Pool reported fewer than 50 cases during this period. Table 1 below shows the monthly distribution of confirmed COVID-19 cases by department from March 14, 2020, to July 24, 2022.
Table 1:Annual Evolution of the Number of Confirmed COVID-19 Cases by Department.
Vital Status of confirmed COVID-19 cases
As of July 24, 2022, the distribution of confirmed COVID-19 cases in the Republic of Congo showed that the vast majority of patients approximately 97% had recovered. Active cases accounted for a small proportion, around 1.45%. The case fatality rate remained relatively low, at about 1.56%. Additionally, only a very small fraction of patients (0.09%) had been transferred to other care facilities. These figures reflect a situation in which most patients recovered, with a relatively low mortality rate at that point in time.
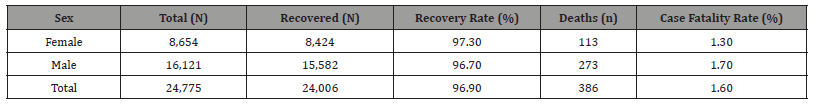
Distribution of confirmed COVID-19 cases by sex
An analysis of confirmed COVID-19 cases in the Republic of Congo by sex shows that the majority of patients were male, accounting for approximately two-thirds of all cases (Table 2). The recovery rate was slightly higher among women (97.3%) compared to men (96.7%). Conversely, the mortality rate was somewhat higher among men, reaching 1.7%, versus 1.3% in women. These findings align with trends observed in various contexts, where men appear to be more susceptible to severe forms of the disease.
Table 2:Distribution of COVID-19 Cases by Vital Status and Sex.
Distribution of confirmed COVID-19 cases by age group
As shown in Table 3, the distribution of confirmed COVID-19
cases in the Republic of Congo by age group shows a predominance
among young and middle-aged adults. The most affected age groups
were:
• 30–39 years: 27.2%
• 40–49 years: 25.6%
• 20–29 years: 15.1%
• 50–59 years: 15.3%
Table 3:Distribution of COVID-19 Patients by Age Group.
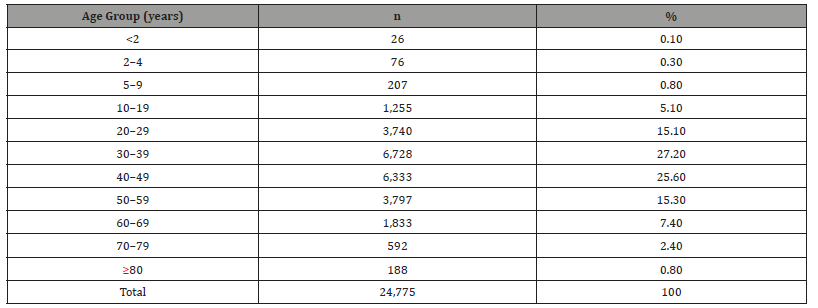
Children and adolescents accounted for a small proportion of cases, with less than 6% among individuals under 20 years old. Older adults aged 60 and over represented approximately 10.4% of cases, indicating a lower incidence in this age group despite their higher vulnerability to severe outcomes.
COVID 19 case fatality overview
From March 14, 2020, to July 24, 2022, a total of 418 dignified and safe burials (DSBs) were conducted in the Republic of Congo. Among these, 386 (92.3%) were for individuals confirmed to have died from COVID-19 via RT-PCR testing, while 32 involved suspected cases. As reported in Table 4, the distribution of recoveries and deaths by age group shows that most confirmed cases occurred among adults aged 20 to 59, with high recovery rates across all categories. However, mortality increased significantly starting in the 50–59 age group, which accounted for more than a quarter of all deaths, followed by those aged 60–69. Individuals aged 70 and older also represented a substantial share of deaths, despite having fewer total cases. In contrast, deaths among children and adolescents remained extremely rare.
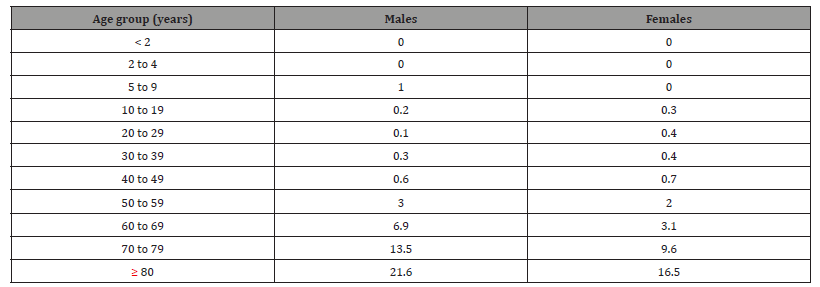
Case fatality rate by age and sex
The COVID-19 case fatality rate varies significantly by age and sex (Table 5). It is nearly zero among children and young people up to 19 years old, then gradually increases with age. In men, mortality begins to rise starting from the 50-59 age group, with a marked increase in older age groups, peaking among those aged 80 and above. Women exhibit a similar pattern, but with consistently lower fatality rates than men across all age groups, particularly among the elderly. This difference highlights an increased vulnerability of men to COVID-19, especially in the senior population.
Table 4:Distribution of COVID-19 recoveries and deaths by age group.
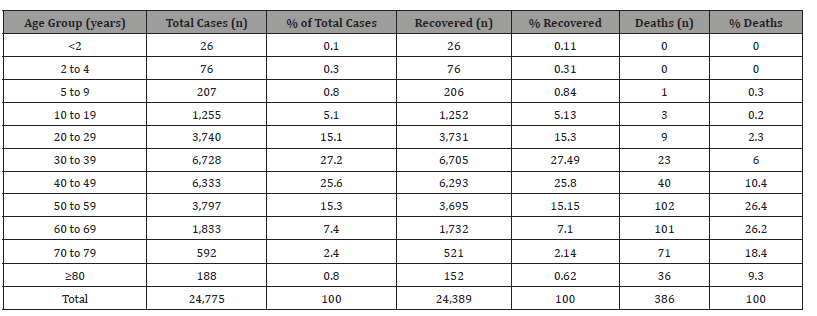
Table 5:Case Fatality Rate by Age and Sex.
Evolution of COVID-19 deaths by epidemiological week
The weekly evolution of COVID-19-related deaths in the Republic of Congo, from March 2020 to July 2022, reveals three distinct phases (Figure 3). The first phase (in blue) corresponds to a low number of weekly deaths during the initial wave. The second phase (in red) highlights a significant peak in mortality occurring between epidemiological weeks 38 and 47 of 2021, with a maximum of 31 deaths in a single week, reflecting the severity of the second wave. Finally, the third phase (in green) shows a marked decline in weekly deaths starting at the end of 2021, with very low figures through July 2022, suggesting either relative epidemic control or the impact of public health interventions.
Characteristics of epidemic waves
Between March 14, 2020, and July 17, 2022, the COVID-19 pandemic in the Republic of Congo unfolded in four successive waves, each marked by a sharp rise and gradual decline in confirmed cases. These peaks reflect the virus’s transmission dynamics and the public health measures taken. Table 6 summarizes the main characteristics of each wave, offering key insights into their intensity, duration, and implications for future outbreak management.
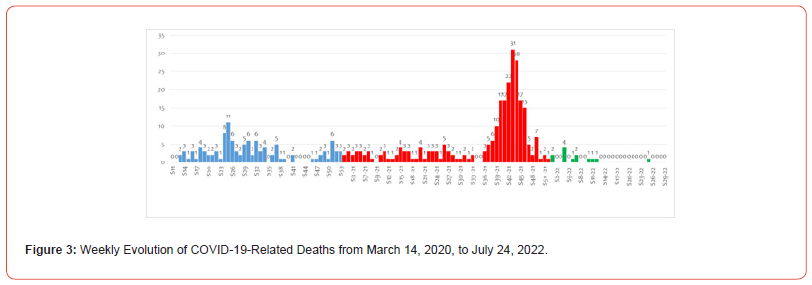
Table 6:Summary of COVID-19 Epidemic Waves in the Republic of Congo.
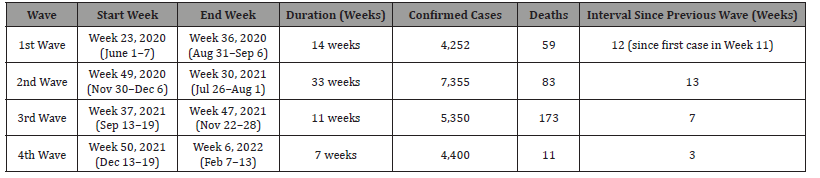
The First Epidemic Wave
Following the confirmation of the first COVID-19 case during epidemiological week 11 of 2020 (March 9–15), the first epidemic wave was observed starting in week 23 (June 1–7, 2020), i.e., 12 weeks after the initial detection of the virus. This wave extended until epidemiological week 36 (August 31–September 6, 2020). During this period, a total of 4,252 confirmed cases and 59 deaths were reported. The 12-week delay between the first case and the onset of the wave marked the period required for significant community transmission to take hold.
The Second Epidemic Wave
The second wave emerged during epidemiological week 49 (November 30–December 6, 2020), 13 weeks after the end of the first wave. It was the most substantial wave in terms of magnitude and lasted until week 30 of 2021 (July 26–August 1). During this period, 7,355 confirmed cases and 83 deaths were recorded. The 13-week interval between the waves reflects a notable resurgence in virus transmission.
The Third Epidemic Wave
Following a period of relative stability, a third wave began in week 37 of 2021 (September 13–19), just 7 weeks after the end of the second wave. This wave was particularly deadly, prompting health authorities to launch an emergency containment campaign. It ended in week 47 of 2021 (November 22–28). Over this 11-week period, 5,350 confirmed cases and 173 deaths were reported. The short 7-week interval highlights the rapid re-emergence of transmission.
The Fourth Epidemic Wave
After a brief lull beginning in week 47 of 2021, a fourth wave emerged in week 50 (December 13–19, 2021), just three weeks (21 days) after the end of the third wave. This wave lasted until week 6 of 2022 (February 7–13), spanning approximately 7 weeks (49 days). A total of 4,400 confirmed cases and 11 deaths were recorded during this period.
Average Onset Interval Between Epidemic Waves
The average interval between successive COVID-19 epidemic waves in the Republic of Congo, calculated based on the observed data for each wave, was approximately 8.75 weeks, or about 9 weeks. The shortest interval recorded was 3 weeks, and the longest interval was 13 weeks. This variability reflects both the dynamics of virus transmission and the timing of public health interventions.
Discussion
Evolution of the COVID-19 pandemic in the Republic of Congo
The trajectory of the COVID-19 pandemic in the Republic of Congo, similar to many African countries, has been characterized by a complex and unpredictable dynamic. This study reconstructs the epidemiological progression, delineates successive epidemic waves, and analyzes the sociodemographic profiles of confirmed cases and fatalities from March 2020 to October 2022.
Underestimation of viral circulation
The total number of confirmed cases (24,775) appears comparatively low relative to the national population, corresponding to a cumulative incidence of approximately 435 cases per 100,000 inhabitants. This incidence is markedly lower than that reported in many other countries, including across the African continent [12]. Several factors contribute to this underestimation. Initially, diagnostic capacity was limited in both accessibility and availability of testing, with screening infrastructure predominantly concentrated in major urban centers such as Brazzaville and Pointe- Noire [13]. Additionally, social distrust and stigma associated with COVID-19 may have impeded test uptake, particularly in rural areas [14]. Seroprevalence studies conducted in several Central African countries and in Republic of Congo have demonstrated a significant disparity between PCR-confirmed cases and true infection prevalence, with exposure rates frequently exceeding 50–60%, indicating far more extensive viral circulation than official statistics suggest [15-17]. The under-detection of asymptomatic and paucisymptomatic infections, coupled with the absence of an integrated surveillance system, hampers comprehensive understanding of community transmission dynamics and the development of herd immunity [18].
Sociodemographic characteristics of cases
Analysis confirms a predominance of males among confirmed infections, accounting for approximately two-thirds of cases, consistent with data reported both regionally and globally [5– 8]. This male predominance may be attributed to differences in occupational exposure, social behaviors, and biological and immunological factors, including a more robust immune response in females mediated by sex hormones and genetic factors [19]. Clinically, females exhibited a marginally higher recovery rate (97.3% versus 96.7%), whereas mortality was elevated among males (1.7% versus 1.3%) [20]. This sex-based disparity underscores the heightened vulnerability of males to severe COVID-19 manifestations, highlighting the necessity for sex-specific considerations in prevention and clinical management strategies [21].
Urban concentration of cases
The majority of confirmed cases were reported in Brazzaville and Pointe-Noire, representing 59.8% and 36.0% of cases respectively [12]. This urban concentration is attributable to high population density, increased mobility, the cities’ significant economic roles, and their status as international entry points facilitating viral dissemination [22]. Conversely, rural regions were less affected, although this may partly reflect underreporting due to limited access to testing and healthcare services [23]. These geographic disparities illustrate inequities in exposure risk and healthcare accessibility, underscoring the need for context-specific surveillance and intervention measures [24].
Case fatality and risk factors
The overall case fatality rate of 1.56% aligns with figures observed in multiple African contexts [25]. Advanced age remains the principal risk factor for mortality, with a pronounced increase in fatality rates beginning at age 50, particularly among those over 60 years [26]. The presence of comorbid conditions such as diabetes, hypertension, and cardiovascular disease correlates with greater disease severity, confirming their pivotal role in progression to critical illness [27]. In contrast, children and adolescents exhibited low susceptibility to severe disease, with near-zero mortality, consistent with global observations [28]. The higher mortality rate among males further suggests complex interactions among biological, behavioral, and comorbidity-related factors [29].
Epidemic wave dynamics
Four distinct epidemic waves were identified, with an average inter-wave interval of approximately nine weeks [12]. The third wave, the most severe, coincided with the emergence and spread of the Delta variant, noted for increased transmissibility and virulence, as documented regionally [30]. This fluctuating epidemic pattern emphasizes the critical need for strengthened epidemiological and genomic surveillance to enable early detection of emerging variants and facilitate timely public health responses [31]. Inter-wave periods represent strategic opportunities to intensify vaccination efforts and reinforce non-pharmaceutical interventions [32].
Low vaccination coverage
Vaccination coverage remains suboptimal, with only 11% of the target population vaccinated as of July 2024 [33]. Vaccine hesitancy, driven by misinformation, distrust of health authorities, and concerns over adverse effects, has led to significant dose wastage through expiration and has imposed economic burdens [34]. This low uptake compromises the establishment of herd immunity and impedes sustainable epidemic control [35]. These findings highlight the urgent need to enhance health communication, community engagement, and targeted strategies to improve vaccine acceptance and coverage [36].
Study limitations
This study has several limitations. It is based solely on PCR-confirmed cases, excluding undetected asymptomatic infections, thereby underestimating true infection prevalence [37]. Data centralization in urban centers limits geographic representativeness, with probable underreporting from rural areas [38]. The lack of systematic genomic sequencing restricts insights into variant circulation and their clinical implications [39]. Furthermore, limited data on comorbidities and socioeconomic factors constrains a comprehensive analysis of risk determinants [40].
Conclusion
The COVID-19 pandemic in the Republic of Congo has been characterized by successive epidemic waves with moderate case fatality despite low vaccination coverage. Underreporting driven by limited testing and vaccine hesitancy has impeded effective epidemic control. These findings underscore the necessity to strengthen surveillance systems, improve health communication, and tailor public health interventions to local contexts to better manage the ongoing pandemic and prepare for future health emergencies.
Conflict of Interest
The authors declare no conflicts of interest regarding the publication of this manuscript.
Contributions of the Authors
GN wrote the protocol. JRNA collected data and drafted the manuscript. GN and CAN supervised and validated the various stages of the study. JRNA and JM performed statistical Analysis. All authors contributed to manuscript review and editing and approved the final version of the manuscript prior to submission.
References
- Smith J, Brown L (2020) Emerging infectious diseases: challenges and responses. J Infect Dis 221(3): 345–352.
- Managing epidemics: key facts about major deadly diseases. Geneva: World Health Organization.
- Nguyen T, et al. (2021) Impact of non-pharmaceutical interventions on epidemic curves. Epidemiol Rev 43(1): 12–25.
- Zhao L, et al. (2022) Viral evolution and pandemic dynamics. Virology 565: 24–35.
- Okoro C, et al. (2021) COVID-19 epidemiology in Africa: a review. Afr Health Sci 21(1): 123–134.
- Mbala-Kingebeni P, et al. (2024) SARS-CoV-2 seroprevalence in Central Africa: 2020–2024. Lancet Infect Dis 24(2): 158–165.
- Johnson M, et al. (2023) Underdiagnosis and testing limitations in COVID-19: a Central African perspective. BMC Public Health 23(1): 1024.
- (2019) Republic of Congo Ministry of Health. Health system assessment report. Brazzaville.
- Adeyemi A, et al. (2022) Health infrastructure and epidemic response in low-income countries. Glob Health Action 15(1): 203–210.
- (2020) World Bank. Health information systems in sub-Saharan Africa: challenges and opportunities. Washington DC.
- Mvoula D, et al. (2023) COVID-19 response strategies in Republic of Congo. Int J Infect Dis 125: 201–210.
- (2022) African CDC. COVID-19 incidence in African countries. Addis Ababa.
- Ntumba E, et al. (2023) Diagnostic capacity and access disparities during COVID-19 in Congo. Health Policy Plan 38(4): 374–383.
- Loubaki L, et al. (2022) Social stigma and testing uptake during the COVID-19 pandemic in Congo. Soc Sci Med 290: 114470.
- Mbaya JK, et al. (2023) Seroprevalence of SARS-CoV-2 antibodies in Central Africa: a systematic review. Int J Epidemiol 52(1): 143–153.
- Fokou G, et al. (2024) Hidden burden of COVID-19: serological evidence in African rural populations. Clin Infect Dis 78(3): 450–460.
- Ndziessi G, Niama RF, Aloumba AG, Peya JM, Ngatse JA, Ngoyomi RA, et al. (2023) Seroprevalence of SARS-CoV-2 antibodies in Republic of Congo, February 2022. Epidemiol Infect 151(e162): 1‑10.
- Ouedraogo A, et al. (2022) Surveillance system gaps and SARS-CoV-2 transmission dynamics in Africa. Epidemics 38: 100519.
- Tchokothe A, et al. (2023) Sex differences in COVID-19 infections and outcomes. Front Immunol 14: 112456.
- Nkongolo A, et al. (2023) Clinical outcomes of COVID-19 by sex in Central Africa. BMC Infect Dis 23(1): 560.
- Takougang I, et al. (2023) Gender-sensitive approaches to COVID-19 prevention in Africa. Glob Public Health 18(2): 298–307.
- Diop B, et al. (2023) Urban transmission dynamics of COVID-19 in Congolese cities. Urban Health 100(3): 703–711.
- Mbemba G, et al. (2023) Rural healthcare access and COVID-19 case reporting in Congo. Rural Remote Health 23(1): 6722.
- Mbele M, et al. (2023) Health disparities and COVID-19 response adaptation in Central Africa. Health Equity 7(1): 65–72.
- (2023) African CDC. COVID-19 case fatality rates across Africa. Addis Ababa.
- Lissouba P, et al. (2023) Age and COVID-19 mortality in Central African populations. Aging Clin Exp Res 35(5): 845–852.
- Kabasele N, et al. (2023) Comorbidities and severity of COVID-19 in African cohorts. J Med Virol 95(7): e28478.
- Ngoy B, et al. (2023) Pediatric COVID-19 cases and outcomes in Central Africa. Pediatr Infect Dis J 42(6): 544–50.
- Mbemba E, et al. (2023) Gender, behavior, and comorbidity interactions in COVID-19 mortality. J Glob Health 13: 06014.
- Diouf M, et al. (2023) Impact of the Delta variant on the third wave in Central Africa. Virol J 20(1): 45.
- Nkoua B, et al. (2024) Genomic surveillance and variant tracking in Republic of Congo. Front Genet 15: 1102805.
- Mboumba S, et al. (2023) Vaccination strategies during inter-wave periods of COVID-19 in Africa. Vaccine 41(21): 2829–2837.
- (2024) WHO Africa. COVID-19 vaccination coverage report, July 2024. Brazzaville.
- Nzau M, et al. (2024) Vaccine hesitancy and misinformation in Central African contexts. Hum Vaccin Immunother 20(1): 2235390.
- Djeukam R, et al. (2024) Impact of low vaccination rates on COVID-19 control in Congo. PLoS One 19(2): e0281146.
- Mbata P, et al. (2024) Community engagement strategies to improve COVID-19 vaccination. Health Promot Int 39(1): daab180.
- Kimbouala S, et al. (2023) Limitations of PCR-based COVID-19 surveillance in Africa. Front Public Health 11: 1034949.
- Ngouanet F, et al. (2023) Geographic representativeness in COVID-19 data collection in Congo. Int J Health Geogr 22(1): 22.
- Mokeba L, et al. (2024) SARS-CoV-2 variant diversity and clinical impact in Central Africa. Infect Genet Evol 110: 105358.
- Tsala A, et al. (2023) Socioeconomic determinants of COVID-19 risk in African settings. Soc Sci Med 315: 115526.
-
Gilbert NDZIESSI*, Ange Clauvel NIAMA, Jys Ryschel NGOYOMI-ALIST and Jethro MASSALA. Dynamics and Epidemiological Characteristics of COVID-19 Epidemic Waves in the Republic of Congo, March 2020 to October 2022. Annal of Pub Health & Epidemiol. 3(1): 2025. APHE.MS.ID.000552.
-
SARS-CoV-2 transmission dynamics; Epidemic wave characterization; Case fatality rate stratification; Public health surveillance systems
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






