 Review Article
Review Article
Weight and Body Mass Index in Children and Adolescents with Type 1 Diabetes Mellitus in a Population from the North of Mexico
Ricardo Marín Rocha*, Leonor Hinojosa Amaya, Elisa Lizbeth Dávila Sotelo, Vincenzo Arenas Fabbri, Ana Gabriela Galvez López and Laura Paola Escamilla Luna
Department of Pediatrics, School of Medicine and University Hospital “Dr. José Eleuterio Gonzalez”, México
Ricardo Marín-Rocha, Department of Pediatrics, School of Medicine and University Hospital “Dr. José Eleuterio González”, Universidad Autónoma de Nuevo León (U.A.N.L.), Av. Francisco I. Madero, s/n, Col. Mitras Centro, C.P. 66460, Monterrey, Nuevo Léon, Mexico.
Received Date: September 07, 2020; Published Date: October 08, 2020
Introduction: Type 1 diabetes mellitus is the most common form of diabetes known among young people and the incidence of this disease in children has increased over time. The increased risk of T1DM autoimmunity associated with body mass index at 2 years indicates a potential role for adiposity, possibly by increasing insulin resistance and ß-cell load.
Materials and methods: An observational, retrospective study where records of 55 patients diagnosed with type Diabetes Mellitus were retrospectively analyzed and used, according to the guidelines of the American Diabetes Association and the American Pediatric Society.
Results: The study consisted of 55 participants where 31 (56%) of them were female, while 24 (44%) belonged to the male sex. The average age that was reported in total for all participants was 14.18 ± 2.72 years. 33 (60%) were of normal weight, while 8 (14%) were overweight, as well as 14 (26%) suffered from obesity.
Conclusion: The Mexican population studied showed an increase in reported cases where people with type 1 Diabetes Mellitus had an increase in body weight compared to what was expected, with people with type 1 DM being overweight as well as obesity.
Keywords: Childhood; Mexican population; Obesity; Overweight; Type 1 diabetes mellitus
Introduction
Type 1 diabetes mellitus (T1DM) is characterized by the progressive autoimmune destruction of insulin-producing pancreatic β cells that forces the use of exogenous insulin [1]. T1DM is one of the most common chronic diseases of childhood [2,3]. The incidence of T1DM in children has increased over time [4]. The increased risk of T1DM autoimmunity associated with body mass index (BMI) at 2 years indicates a potential role for adiposity, possibly by increasing insulin resistance and ß-cell load [4]. T1DM represents more than 90% of the cases of childhood and adolescent diabetes. It is estimated that, of the total world population of 1.8 billion young people under the age of 14, around 440,000 have T1DM. The global incidence of childhood-onset T1DM is increasing worldwide, at an annual rate of about 3%, particularly in children <5 years [3]. There has been a rapid increase in the prevalence of obesity in general populations since the 1980s, and this conspicuous epidemic has spread globally [5]. Although T1DM patients have traditionally been thought to have a lower BMI, current research has shown otherwise [6]. The prevalence of overweight and obesity is also increasing in patients with type 1 diabetes, at an even faster rate than in the general population [5,6]. In type 1 diabetes, the relationship between BMI and mortality is less clear than in the general population [5]. Currently, about 50% of patients with type 1 diabetes are overweight or obese. They also have higher waist and hip circumferences compared to healthy controls [6]. During the first decade of diabetes, mortality is mainly related to acute complications, such as ketoacidosis or hypoglycemic coma, during the second decade renal complications become dominant and are of particular importance due to their influence on the prognosis of patients with diabetes [1]. The microvascular complications of diabetes include nephropathy, retinopathy, and neuropathy and are related to damage to small vessels of the kidney, retina, and nerves [3]. Recent studies suggest that insulin resistance in overweight or obese individuals with type 1 diabetes may be associated with an increased risk of vascular complications [7].
Nordwall et al recently discovered that glycemic control remains the most crucial factor in preventing the development of vascular complications in childhood-onset T1DM [9]. In the Pittsburgh Epidemiology of Diabetes Complications Study, which followed adult patients with type 1 diabetes for an average of 18 years, the prevalence of overweight increased from 29% to 42% and the prevalence of obesity increased seven times from 3 23% [10]. The intensity of insulin treatment influences weight gain as shown in the Diabetes Control and Complications Trial, where patients on intensive insulin therapy gained an average of 4.6 kg in 5 years, which is significantly more than patients in the conventional study arm [11]. The hypothesis proposed was that the existence of overweight and obesity in patients with an established diagnosis of type 1 DM increases the appearance of complications associated with this disease and has an unfavorable impact on the patient’s evolution. The objective was to determine the weight and body mass index of children and adolescents diagnosed with type 1 diabetes mellitus.
Materials and Methods
Observational, retrospective study. It was carried out in the Department of Pediatrics of the University Hospital ‘’ Dr. José Eleuterio González ‘’ where records of 55 patients diagnosed with type Diabetes Mellitus were retrospectively analyzed and used, according to the guidelines of the American Diabetes Association and the American Pediatric Society, who attended a diabetes mellitus camp in July 2018. During the period from April 25, 2020 to May 25, 2020, the data captured in the database carried out in a previous study entitled “Physical condition measured with the Harvard exam in schoolchildren” was analyzed with password Registration before the Ethics Committee and Research Committee of the UANL Faculty of Medicine: PE20-00015.
The inclusion criteria that were integrated to carry out this study were: Patients between 4 and 18 years of age, as well as patients with a diagnosis of type 1 diabetes mellitus. The exclusion criteria that were taken into account were: Comorbidities with poor control (Graves’ diseases, Hashimoto’s thyroiditis, celiac disease, as well as patients with type 2 diabetes mellitus). On the other hand, the elimination criteria used were: incomplete data in the collection sheet and those patients who refused to participate in the study. The description of the design of this study consisted, starting with an analysis of the variables obtained, such as age, sex, weight, height, and body mass index. Weight-for-age above the 95 percentile, 85- 94 percentile overweight, and morbid obesity above 99 percentile were classified as obesity according to the corresponding CDC tables, the specific data from the created database were collected and prevalence was determined in patients with Type 1 Diabetes Mellitus. Records were kept by means of a folio without using the name or registry of the patients for data management and these folios were linked with the name of the patients in a list that was kept by the researcher principal without access for the rest of the research team, in accordance with current data protection laws.
In the analysis of qualitative variables, the Chi-square test or Fisher’s exact test was used in the case of independent groups. For the quantitative variables, they were evaluated with a student’s T of independent samples for parametric distribution and Mann Whitney’s U test for non-parametric distribution. A value of p <0.05 was taken as statistically significant. SPSS version 21 was used to perform the statistical analysis.
Results
The study consisted of 55 participants where 31 (56%) of them were female, while 24 (44%) belonged to the male sex. The average age reported in total of all participants was 14.18 ± 2.72 years, this result being expected, since this disease usually occurs in the young population. The time it took to diagnose the disease in the patients included in this study was on average 6.66 ± 4.13 years. Anthropometric measurements were taken from all patients, where the results obtained according to the sex of the patients were recorded. The registered weight of the female participants obtained an average of 53.91 ± 15.13 kilograms, while the mean weight of the male sex was 58.90 ± 15.91. The mean height obtained for the female sex was 153.47 ± 12.99 centimeters, while for the male it reflected an average result of 163.33 ± 12.56. Based on these results, the average BMI of both sexes was obtained, the female sex showed a mean of 22.37 ± 3.85, while the male sex was 21.77 ± 3.84. After calculating the BMI in children and adolescents, the BMI number was recorded to obtain the percentile category, which the female gender resulted in an average of 73.48 ± 23.14, and the male gender average was 66.46 ± 25.61 (Figure 1).
Based on the data obtained by the percentile of BMI that the patients demonstrated, it can be determined that of the total of the 31 female patients who participated in the study, 16 (51.7%) were of normal weight, while 7 (22.5%) were overweight, as well as 8 (25.8%) suffered from obesity. Of the 24 male patients, 17 (70.8%) were of normal weight, 6 (25%) were overweight, and only 1 (4.2%) suffered from obesity. The patients were measured blood glucose to carry out a control of the disease, where in the last HbA1C carried out elaborated on all patients they released an average value of 6.95 ± 1.36%, thus being within acceptable values.
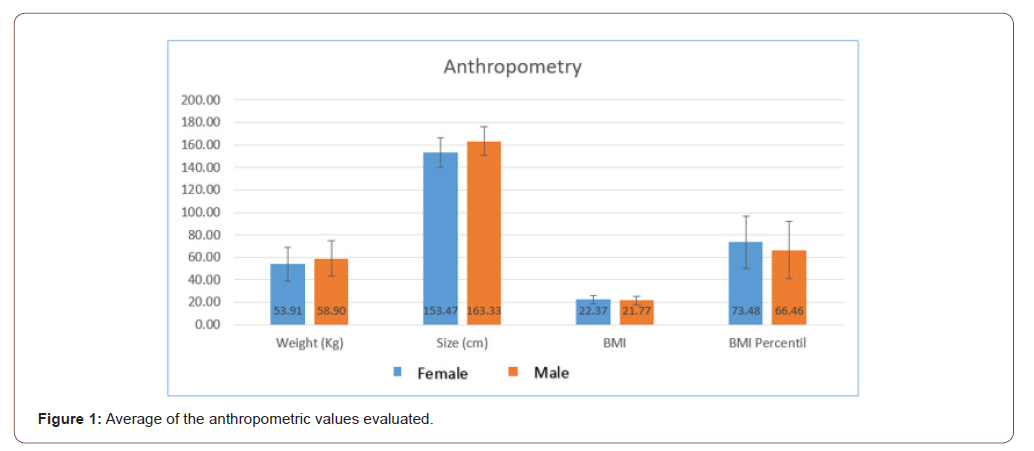
Table 1:Insulins managed by study participants.
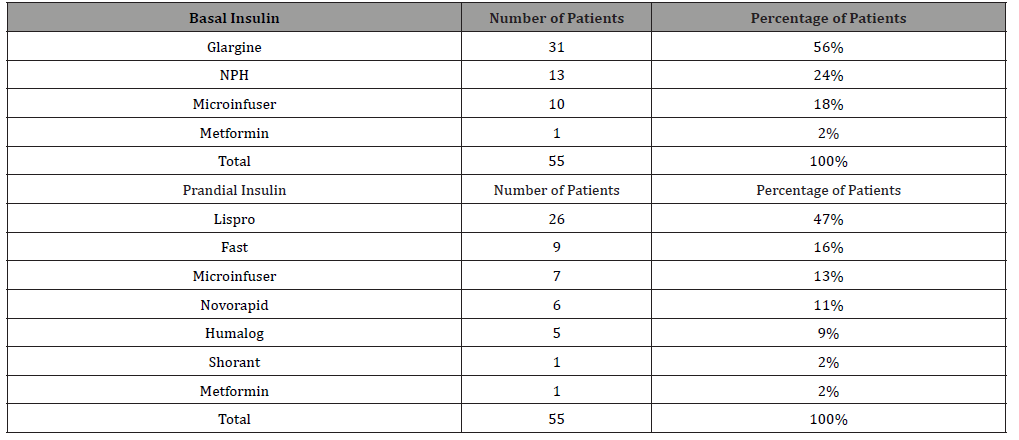
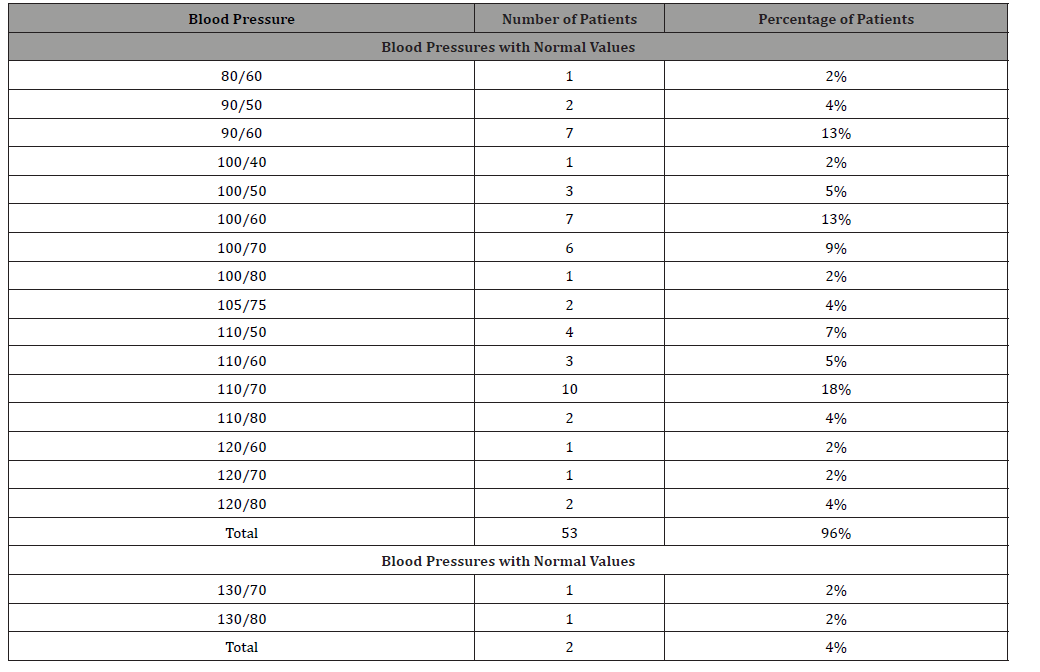
Table 2:Reported blood pressures.
A wide variety of insulins were used for the treatment of the patients, within the basal insulins used it was recorded that in 31 (56%) patients Glargine was used, while in 13 (24%) of the patients NPH insulin was used, in 10 (18%) of the patients received insulin through a pump, and on the other hand, only 1 (2%) of the patients opted for treatment with metformin. Among the prandial insulins that were used in this study, Lispro was used in 26 (47%), rapid insulin was used in 9 (16%) patients, 7 (13%) patients received micro-infusion treatment, 6 (11 %) patients received Novorapid, another 5 (9%) received Humalog, while 1 (2%) of the patients received insulin treatment (Table 1).
Only some of the patients had concomitant diseases at the time of the study, 43 (77%) did not have any disease, 6 (11%) of the patients had hypothyroidism, 1 (2%) patient had atopic dermatitis, 1 (2%) patient had atrophic Hashimoto’s thyroiditis, 1 (2%) patient had arterial hypertension, 1 (2%) patient was reported with depression, as well as 1 (2%) patient was reported with Hashimoto’s thyroiditis / Vitiligo.
At the time of baseline blood pressure measurement, the vast majority of patients registered blood pressure within normal levels, 53 (96%) reported pressures at acceptable values while 2 (4%) of the patients reported blood pressure with values elevated (Table 2).
Another of the vital signs assessed in this study was the heart rate, which obtained an average value of 95.22 ± 16.68 beats per minute. The cardiorespiratory fitness of the patients was reported as: Good, average, below average and poor. In most cases, patients reported below average cardiorespiratory fitness, 20 (36%) of patients were included in this group, 17 (31%) patients reported poor cardiorespiratory fitness, 11 (30%) patients were included in the average group, and thus only 7 (13%) had good cardiorespiratory fitness.
Discussion
Obesity, once rare in type 1 diabetes, is now an increasingly common problem. The accumulation of evidence on the prevalence and consequences of obesity in type 1 DM shows very clearly that this comorbidity is underestimated and little understood. Obesity is likely due to changes in the environment affecting the population as a whole and an unintended consequence of modern and more intensive approaches to the treatment of hyperglycemia (2). Although generally considered thin or sometimes underweight, recent studies have shown that approximately half of all T1DM patients are currently overweight or obese (1). The Pittsburgh Epidemiology of Diabetes Complications Study, which followed adult patients with type 1 diabetes for an average of 18 years, found that the prevalence of overweight increased from 29% to 42% and the prevalence of obesity increased seven times from 3 to 23% [10]. In the study that we carried out, we observed according to the BMI percentile obtained from the total number of patients studied, 40% of the people with type 1 DM were classified within a state above what is considered normal, either overweight or obesity, thus coinciding with studies carried out previously where they reported that a little less than half of the population with type 1 DM reported these same conditions in their body weight.
Previous studies have reported that insulin treatment influences weight gain, as shown in the Diabetes Control and Complications Trial where patients in intensive insulin therapy gained an average of 4.6 kg in 5 years, which is significantly more than patients in the conventional study arm [11]. Weight gain can also be modified by the level of insulin. Two clinical trials comparing insulin glargine U300 with insulin glargine U100 in patients with type 1 diabetes reported less weight gain over 6 months with insulin glargine U300, although insulin requirements increased [12]. During the development of our study, all patients received treatment with insulins, the most used were: Glargine (basal insulin) and Lispro (prandial insulin), being able to find a relationship with weight gain during their application of these two insulins, thus as they have written in previous studies with the use of insulins in general. Nordwall et al recently discovered that glycemic control remains the most crucial factor in preventing the development of vascular complications in childhood-onset T1DM [9]. In contrast, in the study by Amin et al, although glycosylated hemoglobin (HbA1c) levels improved over time, there was no concomitant reduction in microalbuminuria in patients with it, suggesting the role of other factors in non-glycemic genetic and environmental risk [13]. All the patients in our study underwent measurement of HBG where an average of 6.95% was reported, being found as an acceptable value within the parameters.
Conclusion
The Mexican population studied showed an increase in reported cases where people with Type 1 Diabetes Mellitus had an increase in body weight compared to expected, with people with type 1 DM being overweight as well as obesity, this may be taken hand in hand environmental and genetic factors, as well as the use of insulin treatment (being glargine and lispro the most relevant), due to its lipogenic effect already demonstrated previously. There was a little more incidence in cases reported in the female sex, but without having a significant difference. On average, glycosylated hemoglobin was within acceptable limits, responding adequately to insulin treatment in patients including those who were overweight and obese.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Mottalib A, Tomah S, Hafida S, Elseaidy T, Kasetty M, Ashrafzadeh S, et al. (2019) Intensive Multidisciplinary Weight Management in Patients with Type 1 Diabetes and Obesity: a 1-Year Retrospective Matched Cohort Study. Diabetes Obes Metab 21(1): 47-42.
- Corbin KD, Driscoll KA, Pratley RE, Smith SR, Maahs DM, et al. (2018) Obesity in Type 1 Diabetes: Pathophysiology, Clinical Impact, and Mechanism. Endocr Rev 39(5): 629-663.
- Marcovecchio ML, Chiarelli F (2011) Microvascular disease in children and adolescents with type 1 diabetes and obesity. Pediatr Nephrol 26(3): 365-375.
- Ponsonby AL, Pezic A, Cochrane J, Cameron FJ, Pascoe M, et al. (2011) Infant anthropometry, early life infection, and subsequent risk of type 1 diabetes mellitus: a prospective birth cohort study. Pediatr Diabetes 12: 313-321.
- Dahlström EH, Sandholm N, Forsblom CM, Thorn LM, Jansson FJ, Harjutsalo V, et al. (2019) Body Mass Index and Mortality in Individuals with Type 1 Diabetes. J Clin Endocrinol Metab 104(11): 5195-5204.
- Mottalib A, Kasetty M, Mar JY, Elseaidy T, Ashrafzadeh S, Hamdy O (2019) Weight Management in Patients with Type 1 Diabetes and Obesity. Diabetes Obes Metab 21(1): 37-42.
- Edqvist J, Rawshani A, Adiels M, Björck L, Lind M, et al. (2019) BMI, Mortality, and Cardiovascular Outcomes in Type 1 Diabetes: Findings Against an Obesity Paradox. Diabetes Care 42(7): 1297-1304.
- Patterson CC, Dahlquist GG, Gyurus E, Green A, Soltesz G (2009) Incidence trends for childhood type 1 diabetes in Europe during 1989-2003 and predicted new cases 2005-20: a multicentre prospective registration study. Lancet 373: 2027- 2033.
- Nordwall M, Arnqvist HJ, Bojestig M, Ludvigsson J (2009) Good glycemic control remains crucial in prevention of late diabetic complications–the Linkoping Diabetes Complications Study. Pediatr Diabetes 10: 168-176.
- Conway B, Miller RG, Costacou T, Fried L, Kelsey S, et al. (2010) Temporal patterns in overweight and obesity in type 1 diabetes. Diabet Med 27(4): 398-404.
- DCCT Research Group (1995) Effect of intensive diabetes management on macrovascular events and risk factors in the Diabetes Control and Complications Trial. Am J Cardiol 75(14): 894-903.
- Schechter R, Reutrakul S (2015) Management of severe insulin resistance in patients with type 1 diabetes. Current diabetes reports 15(10): 1-12.
- US Renal Data System (2005) US Renal system: annual data report. Available at http://www.usrds.org/adr.htm.
-
Ricardo Marín Rocha, Leonor Hinojosa Amaya, Elisa Lizbeth Dávila Sotelo, Vincenzo Arenas Fabbri, Ana Gabriela Galvez López. Weight and Body Mass Index in Children and Adolescents with Type 1 Diabetes Mellitus in a Population from the North of Mexico. 9(1): 2020. ANN.MS.ID.000702.
-
Smartphones Addiction, Family Affluence Scale; Arabic Version of Smartphones Addiction Scale; Patient Health Questionnaire; Social Networks; depressive symptoms.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






