 Case Report
Case Report
Thalamic Brain Abscess by Fusobacterium Nucleatum
Marcel Sincari* and Francisco José Oliveira Cabrita
Marcel Sincari* and Francisco José Oliveira Cabrita
Marcel Sincari, Department of Neurosurgery, Centro Hospitalar Tondela-Viseu, Portugal.
Received Date: July 24, 2023; Published Date: August 21, 2023
Abstract
Fusobacterium nucleatum (FN) is an opportunistic, gram-negative bacillus that can rarely cause a brain abscess. Thalamic localization of brain abscesses is much rarer than abscesses in other locations of the brain. We present a case of a left-sided thalamic abscess caused by FN in a 59-yearold male patient who debuted with right side hemiparesis. The patient was successfully treated by repeated navigated aspiration and antibiotherapy.
Abbreviations:BBA-Bacterial Brain Abscess; FN-Fusobacterium Nucleatum
Introduction
Fusobacterium nucleatum is an opportunistic pathogen causing different infectious diseases in the oropharynx and other parts of the oral cavity. FN is an obligate anaerobic gram-negative bacillus, it exists in the human oral cavity, gastrointestinal tract, and other body parts. According to some authors it can cause appendicitis, pericarditis, bacterial brain abscess (BBA), osteomyelitis, and chorioamnionitis, is associated with oral and extra-oral malignancies, including colorectal cancer, breast cancer, esophageal squamous cell carcinoma, and gastric cancer [1]. Periodontally healthy individuals and patients with chronic periodontitis commonly experience FN infection and is more abundant in patients with chronic periodontitis [2].
A study reviewed 122 patients with culture-proven BBA over a period of 20 years and identified that Fusobacterium accounted for 6% of the implicated pathogens of monomicrobial BBA [3].
Brain abscess has a rare incidence of 2% of all space occupying lesions and the deep-seated thalamus as a location is reported in 1.3% to 6% of all brain abscesses [4]. Thalamic abscess mortality rate is about 9%-14% when rupture into the ventricles does not happen [4,5], and the mortality approaches 80% if the rupture does happen [6]. The most common reported causative microbes are anaerobes and Streptococci, although 28% of thalamic abscess cases reported are culture-negative [7].
Odontogenic sources are increasingly being reported as the origin of brain abscesses and three criteria were proposed that must be satisfied to establish the diagnosis of a brain abscess with odontogenic origin:
1. an alternative source of bacteremia has not been found.
2. microbiological findings are consistent with oral microflora.
3. there must be clinical or radiographic evidence of dental pathology [8].
Thalamic BBA is described in literature through sporadic cases, the following case reports articles having been found [9-11].
Case Report
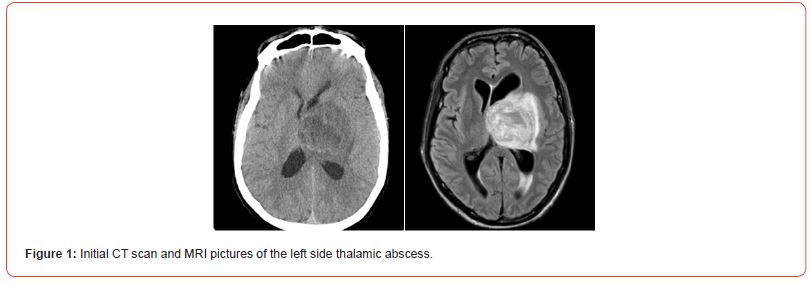
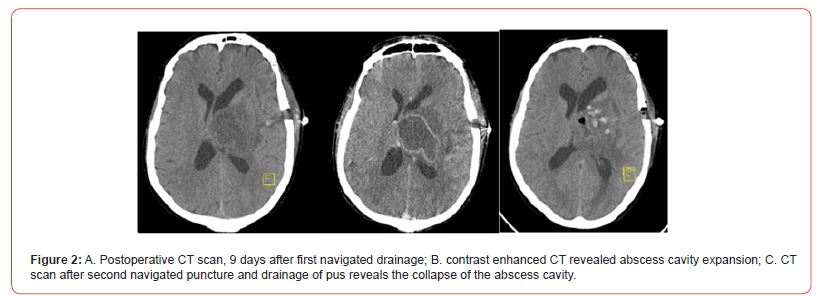
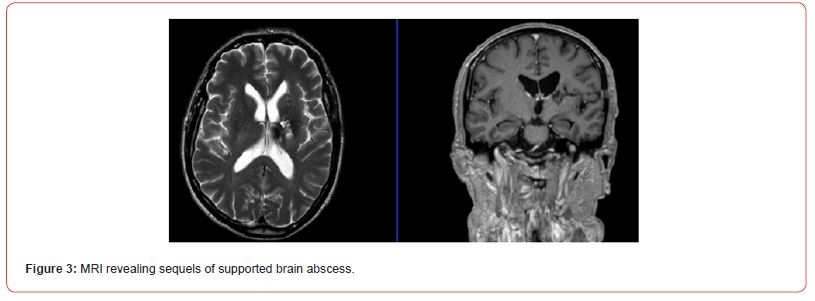
A 59-year-old man was admitted to our department with rightside hemiparesis with several days of evolution. Previously healthy, with no history of oral cavity pathology. MRI revealed left thalamus mass pointing on infection etiology (Figure 1). He was selected for navigated puncture and drainage. During the surgery, about 20cc of yellow, dense, with strong unpleasant smell pus was drained. Laboratory analysis found FN. After 9 days of antibiotic treatment with vancomycin, CT scan (Figure 2A) and contrast enhanced CT scan (Figure 2B) were performed and showed abscess cavity expansion. Second navigated drainage was done with subsequent CT scan that confirmed abscess cavity collapse (Figure 2C). The patient completed 6 weeks of antibiotic therapy with good recovery of hemiparesis. We followed the patient for 4 years, last MRI detects only small sequels of supported abscess (Figure 3).
Conclusions
An abscess localized in the thalamic regions of the brain is a diagnostic and therapeutic challenge even to the most experienced doctors. There is limited experience in this field because of the rarity of such cases and this is another reason for the medical challenge and difficult treatment of thalamic brain abscesses. Navigated or stereotactic drainage is an efficient option for the minimally invasive approach to deep-seated abscesses. Repeated evacuation is needed in order to provide the best possible treatment for the patient. Studies about BBA follow up state that under the appropriate antibacterial treatment, BBA volume decrease by 10%-15% per week, assessed by MRI, during the first 3 months [12]. This emphasizes the importance of MRI follow up as a sign of good medical practice.
Transparency Declaration
All authors have stated that there are no conflicts of interest. No external funding was received for this work.
Statement Of Ethics
The authors have no ethical conflicts to disclose.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Yuanxin Chen, Zhijie Huang, Zhengming Tang, Yisheng Huang, Mingshu Huang et al. (2022) More Than Just a Periodontal Pathogen-the Research Progress on Fusobacterium nucleatum. Frontiers in Cellular and Infection Microbiology 12.
- He J, Huang W, Pan Z, Cui H, Qi G, et al. (2012) Quantitative Analysis of Microbiota in Saliva, Supragingival, and Subgingival Plaque of Chinese Adults with Chronic Periodontitis. Clin Oral Investig 16(6): 1579-1588.
- Mei Jen Hsieh, Wen Neng Chang, Chun Chung Lui, Chi Ren Huang, Yao Chung Chuang, et al. (2007) Clinical Characteristics of Fusobacterial Brain Abscess, Jpn J Infect Dis 60(1): 40-44.
- Lutz TW, Landott H, Wasner M (1994) Diagnosis and management of abscess in the basal ganglia and thalamus: a survey. Acta Neurochir (Wien) 127(1-2): 91-98.
- M Yamamoto, S Hagiwara, Y Umebara, N Tanaka, M Ide, et al. (1993) Solitary pyogenic thalamic abscess -two case reports. Neurologia Medico-Chirurgica 33(9): 630-633.
- GM Callovini, A Bolognini, V Gammone, G Petrella (2009) First-line stereotactic treatment of thalamic abscesses: report of three cases and review of the literature. Central European Neurosurgery 70(3): 143-148.
- K Göbels, D Teichmann, M Grobusch, E Halle, N Suttorp, et al. (2002) A case of multiple brain abscesses due to Streptococcus constellatus. European Journal of Clinical Microbiology and Infectious Diseases 21(2): 156-157.
- Ewald C, Kuhn S, Kalff R (2006) Pyogenic infections of the central nervous system secondary to dental affections-a report of six cases. Neurosurg Rev 29(2): 163-166.
- Shadi Basyuni, Valmiki Sharma, Vijay Santhanam, Ashley Ferro (2015) Fatal thalamic abscess secondary to dental infection. BMJ Case Rep.
- Omer Kilic, Ali Kafadar, Yildiz Camcioglu, Necla Akcakaya, Haluk Cokugras, et al. (2012) Primary Intracranial Abscess localized in the Basal Ganglia: A Case Report. Journal of Tropical Pediatrics 58(1): 71-73.
- Özgür Şenol, Hikmet Turan Süslü, Necati Tatarli, Mehmet Tiryaki, Bülent Güçlü, et al. (2016) Thalamic abscess caused by a rare pathogen:streptococcus constellatus. Pan African Medical Journal 24: 256.
- Carsin A, Revest M, Le Reste PJ, Piau C, Gauvrit JY, et al. (2016) Follow-up of brain abscess volume by magnetic resonance imaging: a pilot study. Abstract 1190. ID Week, New Orleans, USA.
-
Marcel Sincari* and Francisco José Oliveira Cabrita. Thalamic Brain Abscess by Fusobacterium Nucleatum. Arch Neurol & Neurosci. 15(4): 2023. ANN.MS.ID.000870.
-
Brain Disorders. Nerves, Psychology, Spinal Cord, Neuropathies, Anorexia Nervosa, vertigo, Hyperactivity Disorder, Seizure, Mental Health, Nervous System, Cortex, Dementia, Multiple , sclerosis, Cognitive neuroscience, Schizophrenia, Concussion, Alzheimer’s, Dementia, Depression, Motor , neurone Disease, Parkinson’s, Stroke, Addiction, Neurodegenerative Diseases, Consciousness, Dyslexia, Brain Disorders, Traumatic Stress Disorder, Migraine, Epilepsy, Hypertension, Anxiety, Sleep Disorders Autism, Aneurysm.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






