 Research Article
Research Article
Sleep Quality and its Lifestyle Associated Factors among Secondary School Students in an Egyptian City
Dalia G Mahran1*, Dalia M Ismail1, Ali H Zarzour1 and Ghaydaa Shehata2
1Department of Public Health and Community Medicine, Faculty of Medicine, Assiut University, Egypt
2Department of Neurology and Psychiatry, Faculty of Medicine, Assiut University Hospital, Egypt
Dalia G Mahran, Professor, Department of Public Health and Community Medicine, Faculty of Medicine, Assiut University, Egypt.
Received Date: October 21, 2021; Published Date: November 12, 2021
Abstract
Introduction: sleep is critically important to human being as it can properly maintain mental and physical health.
Study objectives: to determine the predictors of poor sleep quality among secondary school students in Egyptian city.
Material and Methods: a cross sectional study was conducted among secondary school students in Assiut. students were selected randomly by multistage stratified random sampling technique Data was collected using a self-administered questionnaire that included demographic data, Pittsburgh Sleep Quality Index (PSQI), lifestyle factors associated with poor sleep quality.
Results: The prevalence of poor sleep among participants was 72.5%. poor sleep quality was more prevalent among females, public school students, urban residents and male students who use illicit drugs. Significant Correlates of poor sleep quality by multivariate analysis were urban residence, using illicit drugs, using internet and mobile phones, irregular breakfast and dinner taking, regular eating carbohydrate and snacks, drinking caffeinated drinks and daytime napping.
Conclusions: poor sleep quality was critically important problem among secondary school student with many lifestyle factors as using illicit drugs, using internet and mobile phones for long time, irregular breakfast and. Dinner time, caffeinated drinks after 6pm and day time napping. Increasing the awareness about healthy sleep is an essential priority especially by focusing programs on adolescents with lifestyle risk factors.
Keywords: Sleep quality; Lifestyle correlates; Secondary schools
Abbreviations: PSQI: Pittsburgh Sleep Quality Index
Introduction
Sleep is a critically important to human being as it can properly
maintain mental and physical health. Good quality of sleep helps
in cognitive restitution, learning, decision making, memory
consolidation and processing of an individual [1,2]. Previous
studies have found that poor sleep has associated with weight gain,
obesity, daytime sleepiness, exhaustion, impaired glucose tolerance
and diabetes, depression and anxiety, impaired memory, and higher
risk of motor vehicle accidents [3-8].
Adolescents’ aged between 10-19 years old suffering poor
sleep quality is a major worldwide concern [9]. The recommended
sleep duration for adolescents is between eight to ten hours of
sleep per night in order they could to function well [10]. The
transition from childhood to adolescents mostly happens during
their schooling environment. During this transition period several
biological, physical and psychological aspects of changes will
occur to the adolescent. During this period the adolescents suffer
from increasing pressures from family, school, social and even
the environmental that indirectly contribute towards the delay in
sleep timing together with a biological sleep phase delay causing
poor sleep quality [11]. Adolescents experience rigid early school
start times, elevated social and academic demands, and increased exposure to electronic media, all of which contribute to poor sleep
quality [12]. Reduction in sleep quality and sleep duration across
populations was found to be linked to increased social and work
demands, changes in lifestyle, smoking, alcohol, increasing use
of technology, current sexual activity, dietary factors, caffeine
intake and level of physical activity [13-20]. This study aimed to
determine the predictors of poor sleep quality among secondary
school students in Assuit, Egypt. The findings from this study
will add new knowledge in the respective field and will provide
useful information for the government or policymakers in terms
of planning an intervention or a campaign targeting the secondary
school students by focusing on the significant predictors of poor
sleep quality of this study. Hence, it will give a wake-up call for
better health and wellbeing for the future generation.
Materials And Methods
A cross sectional study was conducted among 829 secondary school students selected in their second year.
Sample size
Sample size was calculated using Epi- Info, version 7 for descriptive study design. according to the student affairs administration in education high authority, the total number of registered students in the second year of secondary school was. 7,686 students. Based on the least prevalence of poor sleep quality in adolescents from other studies. The calculated number was 375 students. In this study, a multistage stratified random sampling technique was used to select the study sample to correct for the difference in design the sample size was multiplied by the design effect (2); the result equaled 750. An increase in the sample by 10% is used to account for incomplete questionnaires and non responders; the final calculated sample was 825 students.
Sample design
The target students were selected randomly by multistage stratified random sampling technique. Firstly, the schools were stratified into public, private, and technical secondary schools, with further stratification into boys’ and girls’ schools. From every stratum one school was randomly selected, thereby giving a total of four boys’ schools and four girls’ schools. Out of public schools’ strata two schools were selected to include different city regions. Secondly, according to the number of students in the second year in every secondary school, the total sample size was divided proportionately. Lastly, by using simple random sampling the classes were selected. In every class, all students All students were included. Those students who refused to participate were few in number.
Data collection tool and technique
A self-administered questionnaire was used in data collection. The data included the following: (a) demographic data of the students; (b) sleep quality, using the Pittsburgh Sleep Quality Index (PSQI); (c) lifestyle factors associated with poor sleep quality.
The demographic variables were categorized as follows: sex (male and female), residence (rural and urban), type of education (public, private, and technical), smoking (nonsmoker, currently smoker, and ex-smoker) and addiction (using illicit drugs and no). The PSQI is a questionnaire that is used to evaluate sleep quality over the last month; it is a validated questionnaire that has been used to evaluate sleep quality of adolescents and young adults. It consists of 19 self-rated questions that are grouped into seven component scores, all of which have equal weight on a 0–3 scale. These components are sleep latency, sleep duration, subjective sleep quality, habitual sleep efficiency, daytime dysfunction, sleep disturbances and use of sleep medication. The seven component scores are summed to give a global PSQI score from 0 to 21; a higher score indicates worse sleep quality. A score more than 5 differentiates between good and bad sleep quality, with a sensitivity of 89.6% and specificity of 86.5%.The internal consistency of the index (Cronbach’s α = 0.83). The index needs 5 to 10 min to complete [21]. Suleiman et al. (2010) [22] translated the questionnaire into Arabic.
Lifestyle factors associated with poor sleep quality were categorized as follows: watching TV and using internet (not regularly, less than one hour per day, one hour per day, two hours per day, 3-4 hours per day and 5 hours or more per day), using mobile phones (calls/text messages) (zero, less than one hour per day, one to > 2 hours per day and ≥2 hours per day), sleeping with lights on, daytime napping and using bed for activities other than sleep (always, usually, sometimes and never), eating breakfast, lunch, dinner, snacks, vegetables and fruits, milk, carbohydrates and caffeinated drinks after 6 pm (regular and irregular). Data collection was done away from the exam times at the middle of the first semester of academic year. The questionnaire was filled in by the students during class. It was explained page by page. In every class, the class teacher and two well-trained data collectors assisted in watching the students and keeping understanding and completeness of data during questionnaire filling in.
Data management and statistical analysis
The study hypothesis was “poor sleep quality would be
associated with many demographic, lifestyle factors and special
habits that could be risk factors for poor sleep quality”.
Descriptive statistics were used in the form of frequencies,
means, and standard deviations [SDs] also tests of significance such
as the chi-square test and Fisher’s Exact test for qualitative variables
and Student’s t test for quantitative variables. For prediction of
factors that could be associated with poor sleep quality binary
logistic regression analysis was used. All significant factors that
were found to be likely associated with poor sleep quality by using
bivariate analysis were used to construct regression models. Only
significant variables included in the final equation. P-value was
considered significant when it was equal to or less than 0.05.
Ethical considerations
Before starting data collection, the proposal was approved by the Faculty Ethical Review Committee in Assiut university. Also, an approval was received from the Central Agency of Public Mobilization and Statistics and administration of secondary education and directors of every school. After explanation of the aim and methods of the study, an informed consent was taken from every student. As the questionnaire items did not include sensitive issues, parents’ consent was not sought, and it was not requested from the higher authorities. It was explained at the class that the collected data will be used for scientific research only and are confidential.
Results
The mean age of the students was 16.66 ± 0.72 SD. About one half (54.9%) were boys, 56.2% attended technical schools, 66.7% were from urban areas, 14.7% of males were currently smokers, 7.7% of males reported using illicit drugs as hashish or bango. The prevalence of poor sleep among participants was 72.5%, using the cut off of PSQI >5. The mean PSQI score was 7.35 (SD = 2.94). Poor sleepers were statistically significantly higher among females (77.0%) than males (68.8%). Urban residents (76.8%) evidenced poorer sleep compared to rural residents (63.6%). The percent of poor sleepers was higher among public school students (81.4%) than private school students (76.9%). The percent of poor sleepers was statistically significantly higher among male students who use illicit drugs (91.4%) than non-users (67.4%) of illicit drugs (Table 1).
Table 1: Relationship between demographic factors & special habits and sleep quality among secondary school students in Assiut city, 2015.
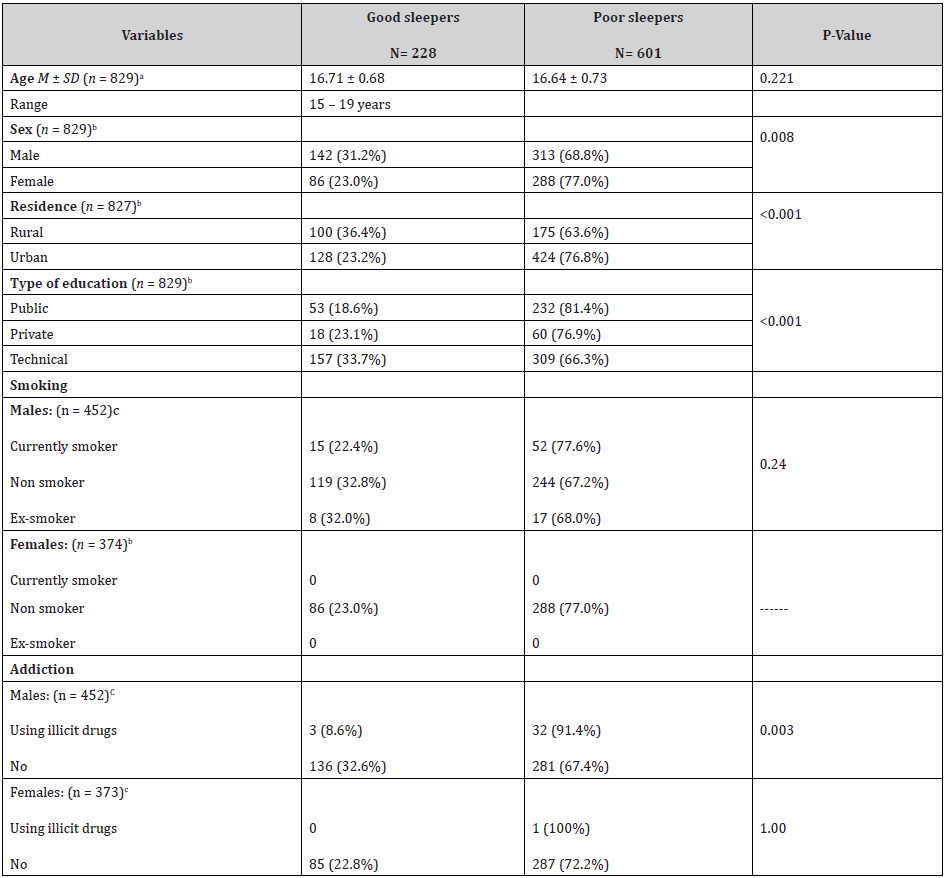
aStudent’s t test was used. bChi-square test was used. c Fisher’s Exact test was used.
The percent of poor sleepers was the highest among students who were usually taking sleep naps (79.8%), and the lowest among students who were never taking sleep naps (53.5%). In addition, the percent of poor sleepers was highest among students who were always using bed for activities other than sleep (79.3%), and the lowest among students who were never using bed for activities other than sleep (60.0%). The percent of poor sleepers was the highest among students who reported using internet 5 hours or more per day (82.9%), and the lowest among students who reported using internet one hour per day (66.7%), the association was statistically significant (p=0.001). Also, the percent of poor sleepers was the highest among students who reported using mobile phones 2 hours or more per day (80.7%), and the lowest among students who reported no using mobile phones (62.6%), the association was statistically significant (p=0.003). On the other hand, there was no statistical significant association between sleep quality and watching TV, using computer or video games.
Regarding the percent of poor sleepers was higher among students who eat breakfast, lunch and dinner irregularly (less than 5 days per week) 76.4%, 79.1% and 81.6% respectively compared to 67.4%, 70.6% and 66.1% among students who eat breakfast, lunch and dinner regularly, the associations were significant (p<0.05). Also, the percent of poor sleepers was higher among students who eat snacks and carbohydrates regularly (less than once every day) 80.9% and 75.0% respectively compared to 68.7% and 68.3% among students who eat snacks and carbohydrates irregularly, the associations were significant (p<0.05). The percent of poor sleepers was higher among students who reported always drinking caffeinated drinks after 6 pm (77.1%) compared to (65.1%) among students who reported never drinking caffeine containing drinks after 6 pm (p < 0.05; Table 2)
Table 2: Relationship between lifestyle factors and sleep quality among secondary school students in Assiut city, 2015.
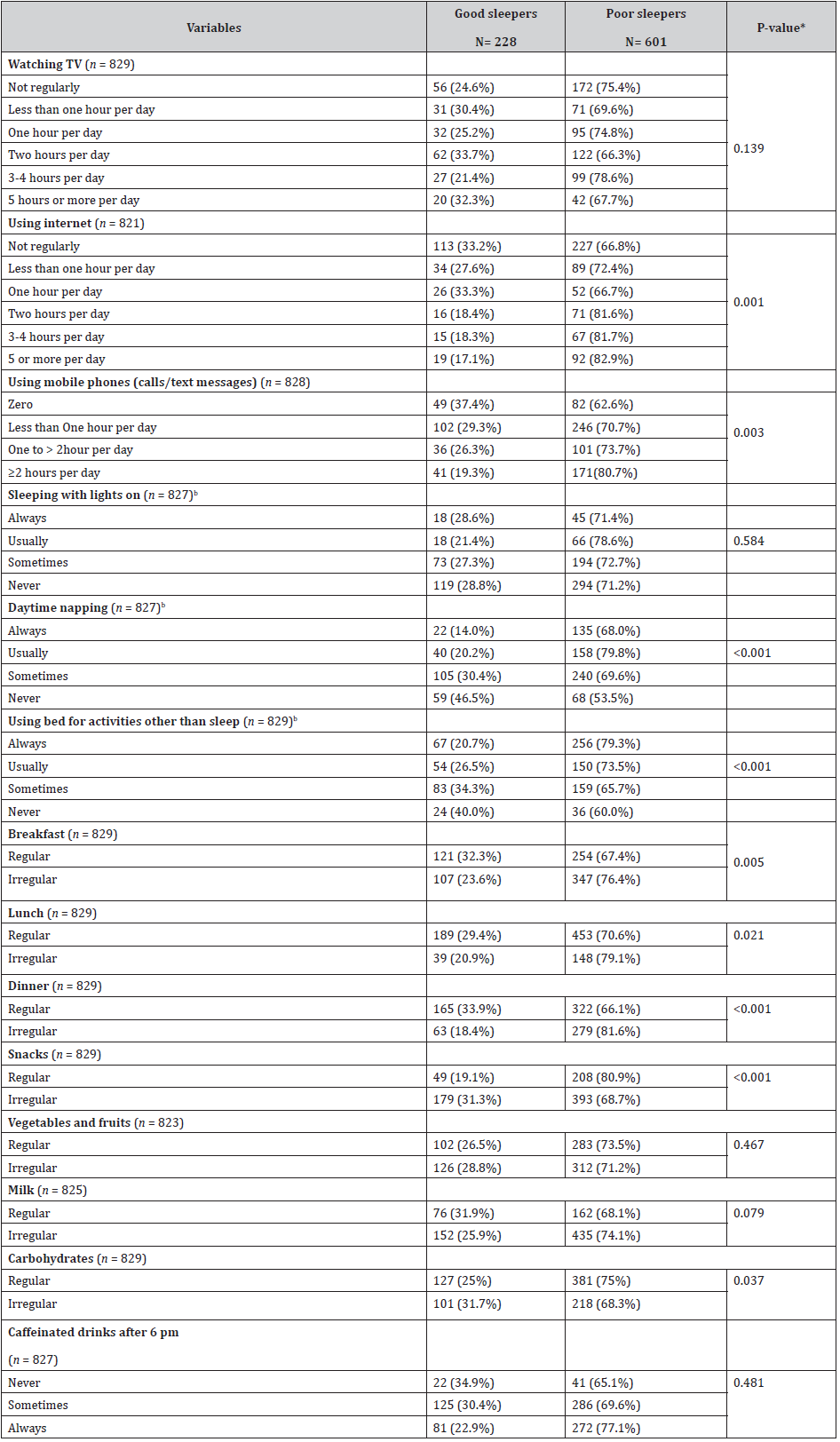
*Chi-square test was used
Table (3) presents multivariate logistic regression, the significant predictors of poor sleep were: the chance of poor sleep increased 1.5 times among urban residents compared to rural residence [odds ratio (OR) 1.5, 95% confidence interval (CI) (1.0 - 2.2) P=0.047]. Using illicit drugs regular or sometimes has shown significant increase in the chance of poor sleep quality 6.6 times compared to not using it [OR 6.6, CI (1.9-23.0) p=0.003]. The chance of poor sleep increased 1.9 times with using internet three hours or more per day compared to using internet less than one hour per day [OR 1.9, CI (1.2-3.2) p=0.009]. Also, using mobile phones two hours or more per day has shown significantly increasing the chance of poor sleep quality two times compared to not using mobile phones [OR 2.0, CI (1.1-3.5) p=0.015]. Also, irregular breakfast taking (less than five days per week) has shown significantly increasing the chance of poor sleep quality 1.6 times compared to regular breakfast taking [OR 1.6, CI (1.1-2.3) p=0.012]. Also, irregular dinner taking (less than five days per week) has shown significant increase in the chance of poor sleep quality 1.7 times compared to regular dinner taking [OR 1.7, CI (1.2-2.5) p=0.006]. Also, regular eating carbohydrate (once or more per day) has shown significant increase in the chance of poor sleep quality 1.5 times compared to irregular eating carbohydrate with [OR 1.5, CI (1.0-2.1) p=0.041]. Also, regular eating snacks (once or more per day) has shown significant increase in the chance of poor sleep quality 1.9 times compared to irregular eating snacks with [OR 1.9, CI (1.3-2.9) p=0.002]. Also, always drinking caffeinated drinks after 6p.m has shown significant increase in the chance of poor sleep quality 1.9 times compared to never drinking caffeine containing drinks after 6p.m [OR 1.9, CI (1.0-3.7) p=0.045]. Also, always daytime napping has shown significant increase in the chance of poor sleep quality 4.8 times compared to never daytime napping [OR 4.8, CI (2.6-9.0) p>0.0001].
Table 3: Predictors of Poor Sleep Quality Among Secondary School Students in Assiut, 2015 Identified by Multivariate Logistic Regression Analysis
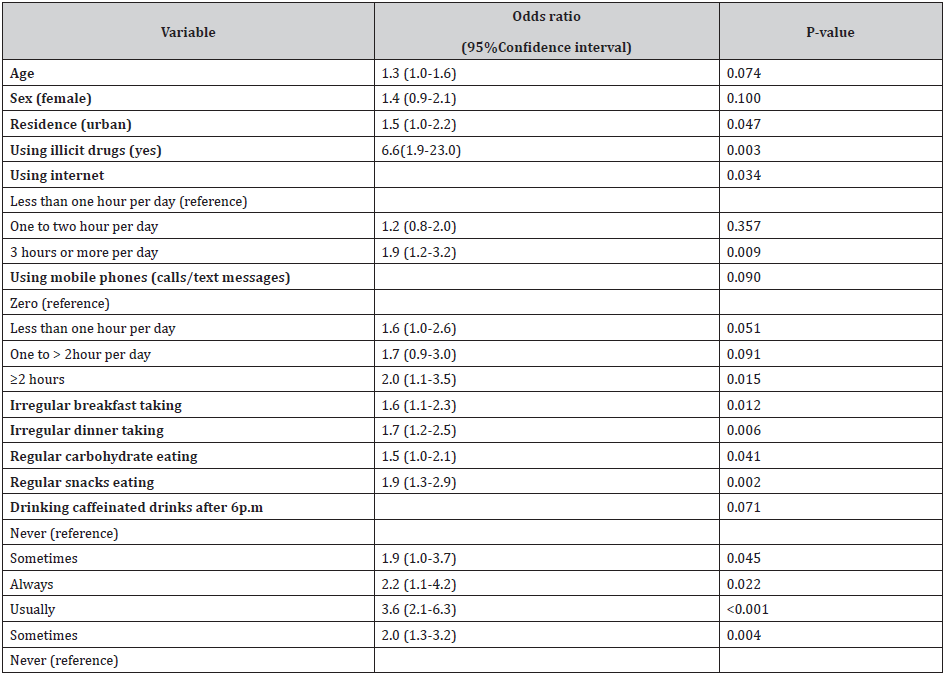
N = 808. Nagelkerke R Square = 0.21. Odds ratio is adjusted for all variables in the table.
Discussion
This study was a cross-sectional study. It was conducted to identify the associated factors which may lead to poor sleep quality. In the current study, age was significant predictor of poor sleep quality [OR 1.4, p=0.014]. This is consistent with the results of meta-analysis of 41 surveys worldwide conducted by Gradisar et al. [23]. Age is important factor affecting sleep pattern in adolescents as it leads to delay of sleep time and restrict school night sleep [23]. The effect of age (especially adolescence) on sleep is attributed to developmental changes in the circadian alerting system, so the preferred times for falling asleep and waking are typically delayed in adolescents [24]. The delayed sleep time during adolescence, early school start time and increased academic and social demands lead to poor sleep.
In the current study, poor sleep quality was associated with female gender. The prevalence of poor sleep quality was higher among females than males with statistical significant difference (p=0.008). This difference may be attributed to that females are more subjected to anxiety, depression and long periods of thinking [25]. This is consistent with the results of many studies. Merdad et al., 2014 in the Saudi study in Jeddah among 947 high school students aged 14–23 years found that females has significantly higher PSQI than males [12]. Similar results were found among 1,629 Hong Kong Chinese adolescents aged 12 to 19 years [9]. In Japanese study among 94,777 adolescents, it was also reported that female adolescents had more short sleep duration than males and more female adolescents rated their sleep quality as poor or very poor [26].
In the current study, the prevalence of poor sleep quality was higher among residents of urban area with statistical significant difference (p>0.0001). Using logistic regression, the chance of poor sleep increased two times among urban residents compared to rural residence [OR 2.0, p=0.002]. This finding may be due to calm green environment, early closure of services in rural areas and more access of the adolescents to internet and new technology in urban areas that allows better sleep quality. This result is comparable with the results of study made by Liu et al., 2008 among 1056 high school students in China who found that urban students go to bed later than rural students [27]. This is also consistent with the findings of Haseli-Mashhadi et al., 2009 that rural residents were more likely to report good levels of sleep quality compared to urban residents in middle-aged and elderly Chinese [28].
In the current study, we found that technical school students
were less liable to poor sleep than public and private school
students with a highly statistical significant difference (p>0.0001).
In multiple analysis, the chance of poor sleep increased 1.8 times
among public education students compared to technical education
students [OR 1.8, p=0.023]. This finding may be related to the lower
socioeconomic level of technical school students, less access to new
technology, more physical activity and less napping due to more
afternoon jobs. All these factors lead to better night sleep. This
finding could be explained also by the fact that majority of technical
schools students are residents of rural areas.
This study found that the percent of poor sleepers was higher
among smoker males than non-smoker males (77.6% versus 67.2%
respectively), but the association was not statistically significant.
The previous studies showed different results about association
between sleep and smoking. Cheng et al., 2012 found no statistical
significant difference between good and poor sleepers (PSQI
score≥6) as regarding smoking among 4,318 incoming university
students in Taiwan [29]. The same results were found among 1,515
African Americans, aged 30-65 years, [30] and 2,803middle aged
Chinese [31]. On the other hand, a study among 12,154 high school
students in USA [16] and other study among 2,432 Norwegian
adolescents, aged 15-17 years [32], revealed that being a current
smoker increased the odds of sleeping < 8hours. Additionally
smoking was found as a risk factor for sleep problems in Japanese
[33] and Hong Kong studies [9]. Although the results of the studies
differs between significant and non-significant association between
different sleep measures and smoking but being a current smoker a
bad habit was related to poor sleep measures in most studies. The
effect of smoking on sleep is attributed to nicotine stimulation of
nicotinic acetylcholine receptors in the brain that results in release
of a variety of neuro-transmitters in the brain, most importantly
dopamine. Based on these effects nicotine could interact with sleep
regulating mechanisms and may affect sleep quality or Rapid Eye
Movement sleep [34].
This study found that the percent of poor sleepers was higher
among male students who used illicit drugs regularly or sometimes
compared to non-users of illicit drugs with statistical significant
difference (p=0.003). By using logistic regression, using illicit
drugs regular or sometimes has shown significant increase in the
chance of poor sleep quality 6.6 times compared to non users [OR
6.6, p=0.003]. Despite the presence of such significant relation, this
point could not be analyzed as only 35 students reported using
illicit drugs and many students who use illicit drugs would deny
addiction, so this relation would be studied with other study means
as e-mail or phone. This result is consistent with other studies in
USA (16) and Norway [32].
In this study, it was found that using internet was a significant
risky behavior associated with poor sleep quality (p=0.001), by
using multiple regression, using internet three hours or more per
day was a significant predictor of poor sleep [OR 1.9, p=0.009].
This relation is mostly due to increase the alertness and level of
activity of the nervous system. Also exposure to the bright light
of the viewing screen before sleep may affect the sleep/wake
cycle through suppression of the nocturnal salivary secretion
of melatonin. In addition, the content of television programs
and computer game playing may be excessively violent and/or
stimulating, which may inhibit relaxation and result in anxiety and
difficulty in falling asleep [19, 35]. This finding is in agreement
with many studies, as that was conducted among 1,956 Turkish
high school students aged between 14 and 18 years which found
that the students with internet addiction (using Internet Addiction
Test) were more likely to have difficulty in falling asleep and night
awakenings, problematic internet users and internet addicts were
found to sleep significantly less than average internet users [36].
Another Taiwanese study found that poor sleep quality (PSQI score
≥6) was significantly associated with a higher tendency toward
internet addition [29]. In a study, among 2,546 Belgium secondary
school children, adolescents who spent more time using the
internet went to bed significantly later during the week and during
the weekend, got up later on weekend days and spent less time in
bed during the week [18].
In the current study, there was significant inverse relation
between sleep quality and hours of using mobile phones (p=0.003).
By multiple analysis, using mobile phones two hours or more
per day was significant predictor of poor sleep quality [OR 2.0,
p=0.015]. This relation is consistent with a study; done in UK
among 738 adolescents aged 11–13 years, that found that frequent
use of mobile phones was associated with difficulty in falling asleep,
frequent early awakening and inversely associated with weekday
sleep duration [37]. Also the study, conducted by Yang et al., 2010
among 11,111 Taiwanese adolescents aged 12-18 years, found
that problematic cell phone use was associated with insomnia in
adolescents [38]. While the study, conducted by White et al., 2011
among 350 college students with average age 20 years in USA,
found that mobile phone use was related to sleep quality, but not
sleep length [39].
On the other hand, the current study found that there was
no statistical significant association between sleep quality and
frequency of watching TV or using computer or video games. These
findings are consistent with the study of Lund HG et al., 2010 who
found that daily hours of television and video game exposure were
not significant predictors of the PSQI score [40]. Also consistent
with Chen et al., 2006 study findings that hours of watching TV/
using computer during weekdays and were not significantly
correlated with adequate sleep [41]. But other studies in Saudi
Arabia, Spain, Norway and USA found that short sleep duration was
associated with more TV watching [16,32,42-44].
In this study, it was found that there was no statistical significant
association between sleep quality and sleeping with lights on. This
finding is consistent with the study of Gellis and Lichstein, 2009
among 220 middle aged adults (mean age 42±12.8 SD) in USA [45].
This study found that there was inverse relation between
daytime napping and sleep quality (p>0.0001). Also using logistic
regression, always daytime napping was significant predictor
of poor sleep quality [OR 4.8, p>0.0001]. This relation could be
attributed to that long and late naps interfere with night sleep. This
finding is consistent with the study of Gellis and Lichstein, 2009
in USA that found significant differences between good and poor
sleepers in relation to daytime napping that poor sleepers were
more likely to nap during the day (PSQI >5) [45]. The same result was obtained by Jefferson et al., 2005 among 516 individuals aged
18 to 65 years in a population based study [46].
In this study, we found association between poor sleep quality
and using bed for activities other than sleep (e.g. reading, watching
TV, mobile phone using or thinking about important matters), the
association was statistically significant (p>0.0001). Several factors
may lead to poor sleep in adolescents who used bed for activities
other than sleep, including that these activities may replace the
time for sleep and it may increase arousal due to the media or
book contents or due to alerting features of the screens including
brightness and the specific wave-length of the screens [35]. This
finding is consistent with the study of Gellis and Lichstein, 2009 in
USA that found that bed activities other than sleep especially more
likely to worry, plan, or think about important matters at bedtime
were greater among poor sleepers (PSQI >5) [45]. In another study
conducted by Lemola et al., 2015 among 362 adolescents aged 12–
17 years in northwestern Switzerland, found that electronic media
use in bed before sleep especially being online (Facebook, Chat
etc.) in bed and having the mobile phone switched on at night was
related to shorter sleep on weekday nights and only being online in
bed before sleep was related with sleep difficulties [35].
The significant association between sleep quality and regularity
of meals pattern (breakfast, lunch and dinner) (p= 0.005, 0.021,
>0.0001 respectively). Adequate sleep time could be attributed
to waking up early and having their breakfast before going to
school. Having regular meals pattern may reflect more stable
family structures with the parents and children having their meals
together, and help adequate sleep [43]. This finding is consistent
with the results of many studies as the study of Cheng et al., 2012
who found that students who skipped breakfast were more likely
to be poor sleepers (PSQI score ≥6) [29]. Also Al Hazzaa et al., 2014
found that having low intake of breakfast decreased the odd of
having adequate sleep duration [43]. On the other hand, irregular
breakfast taking (less than five times per week) [OR 1.6, p=0.012]
and irregular dinner taking (less than five times per week) [OR 1.7,
p=0.006] were significant predictors of poor sleep quality. Also,
Stea et al., 2014 found that having an irregular meal pattern were
associated with short sleep duration [32], the same result was
reported by Chen et al., 2006 that adopting healthy diet (eating
breakfast daily, eating three meals a day, drinking at least 1,500cc
of water daily, choosing foods with little oil, etc.) was negatively
associated with inadequate sleep [41].
Regular carbohydrate eating (once or more per day) and
regular snacks eating (once or more per day) were significant
predictor of poor sleep quality [OR 1.5, p=0.041] and [OR 1.9, CI
p=0.002] respectively. These findings are consistent with the
results of the study of Al-Disi et al., 2010 among 126 Saudi girls
aged 14-18 years, who found that subjects sleeping < five hours/
day showed a significantly higher percent of carbohydrate intake
from their total daily energy intake than those sleeping > seven
hours/day [47]. In other study, among eleven healthy volunteers
aged 34-49 years completed in random order two 14-day stays in
a sleep laboratory with access to palatable food and 5.5-h or 8.5-h
bedtimes. Nedeltcheva et al., 2009 found that sleep restriction was
accompanied by increased consumption of calories from snacks,
with higher carbohydrate content [48]. Proposed mechanisms by
which insufficient sleep may increase caloric consumption from
carbohydrates and snacks include: more time and opportunities for
eating, psychological distress, uninhibited eating (low leptin and
high ghrelin secretion), more energy needed to sustain extended
wakefulness, and changes in appetite hormones [49].
As found in the study results, there were no statistical significant
associations between sleep quality and having milk or its products
or eating vegetables and fruits. This is consistent with the results
of the study of Al-Hazzaa et al., 2014 among Saudi adolescents
who found that the frequency of consumption of vegetables, fruits
and milk/dairy products intake per week were not significantly
associated with sleep duration [43]. Although milk drinking is
thought to promote sleep, this relation was not found in the current
study may be due to the sleep promoting effect limited to drinking
milk at night. This is contradicted with the results of HELENA study
among European adolescents that found that the proportion of
adolescents who eat adequate amounts of fruits and vegetables
was lower in shorter sleepers than in adolescents who slept ≥ eight
hours per day [50]. This difference may be due to different cultural
and social habits of eating behaviors between Arab and European
adolescents.
The current study shows that there was statistical significant
association between drinking caffeinated drinks after 6 pm
and poor sleep quality [OR 1.9, p=0.045]. While there were no
statistical significant association between sleep quality and
regularity of drinking caffeinated drinks per week. These results
may be attributed to short term effect of caffeine on sleep and
those who drink caffeinated drinks early in the day cannot nap
so can have sleep with good quality at night, this is consistent
with Lund et al., 2010 who found that the number of caffeinated
drinks per day did not significantly differ between PSQI groups
[40]. The same result was found by Merdad et al., 2014 that there
was no statistical significant difference of PSQI scores between
different amounts of caffeine intake per day [12]. While Cheng et
al., 2012 found statistical significant association between higher
frequency of tea-drinking (≥3 times / week) and poor sleep quality,
and non-statistical significant association between frequency
of coffee-drinking and sleep quality [29]. While Mindell and his
colleges, in their study among 1473 parents/caregivers of children
ages newborn to 10 years in America, found that regular caffeine
consumption was associated with shorter total sleep time [51]. The
same association was detected by Drescher et al., 2011 among 319
American adolescents between 10-17 years [51].
The results of the current study could be generalized because
different schools from different regions in Assiut city were included.
The current study was limited by being a cross-sectional study;
we could not judge the causal relation between the outcome and
predictors, that the temporal sequence was not clear. to avoid more
elongation of the questionnaire, which could affect the accuracy
of data, the study did not include other factors related to sleep as
academic performance, sleep habits during exam times, weekends,
and holidays. These factors could be studied in other studies.
Conclusion
Poor quality of sleep should be considered a critically important medical problem, especially in adolescents. It’s associated with many life style factors as using illicit drugs, using internet and mobile phones for long time, irregular breakfast and. Dinner time, caffeinated drinks after 6pm and day time napping. A behavioral intervention program should be developed and implemented by the Ministry of Education in secondary schools. Parents should also monitor their sleep timing and behaviors. Mass media should conduct special programs to increase the awareness about sleep needs, healthy sleep patterns, risk factors and consequences of poor sleep to be avoided.
Acknowledgment
Great thanks to the competent research field assistants for helping in data collection.
Disclosure
The authors declare that there was no conflict of interest.
References
- Smaldone A, Honig JC, Byrne MW (2007) Sleepless in America: inadequate sleep and relationships to health and well-being of our nation's children. Pediatrics 119(Supplement 1): S29-S37.
- Sadeh A (2007) Consequences of sleep loss or sleep disruption in children. Sleep medicine clinics 2(3): 513-520.
- Altevogt BM, Colten HR (2006) Sleepdisorders and sleep deprivation: an unmet public health problem: National Academies Press.
- Lucassen EA, Zhao X, Rother KI, Mattingly MS, Courville AB, et al. (2013) Evening chronotype is associated with changes in eating behavior, more sleep apnea, and increased stress hormones in short sleeping obese individuals. PloS one 8(3): e56519.
- Chaput JP, Després JP, Bouchard C, Tremblay A (2007) Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec family study. Obesity15(1): 253-261.
- Malhotra S, Kushida CA (2013) Primary hypersomnias of central origin. CONTINUUM: Lifelong Learning in Neurology 19(1, Sleep Disorders): 67-85.
- Moo-Estrella J, Pérez-Benítez H, Solís-Rodríguez F, Arankowsky-Sandoval G (2005) Evaluation of depressive symptoms and sleep alterations in college students. Archives of medical research 36(4): 393-398.
- Hounnaklang N, Lertmaharit S, Lohsoonthorn V, Rattananupong T (2016) Prevalence of poor sleep quality and its correlates among high school students in Bangkok, Thailand. Journal of Health Research 30(2): 91-98.
- Chung K-F, Cheung M-M (2008) Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. Sleep 31(2): 185-194.
- Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, et al. (2015) National Sleep Foundation’s updated sleep duration recommendations. Sleep Health 1(4): 233-243.
- Kesintha A, Rampal L, Sherina M, Kalaiselvam T (2018) Prevalence and predictors of poor sleep quality among secondary school students in Gombak District, Selangor. The Medical journal of Malaysia; 73(1): 31-40.
- Merdad RA, Merdad LA, Nassif RA, El-Derwi D, Wali SO (2014) Sleep habits in adolescents of Saudi Arabia; distinct patterns and extreme sleep schedules. Sleep medicine 15(11): 1370-1378.
- Al-Hazzaa HM, Musaiger AO, Abahussain NA, Al-Sobayel HI, Qahwaji DM (2012) Prevalence of short sleep duration and its association with obesity among adolescents 15-to 19-year olds: A cross-sectional study from three major cities in Saudi Arabia. Annals of thoracic medicine 7(3): 133-139.
- Calamaro CJ, Mason TB, Ratcliffe SJ (2009) Adolescents living the 24/7 lifestyle: effects of caffeine and technology on sleep duration and daytime functioning. Pediatrics 123(6): e1005-e10.
- Chokroverty S (2009) Sleep Disorders Medicine E-Book: Basic Science, Technical Considerations, and Clinical Aspects: Elsevier Health Sciences.
- McKnight-Eily LR, Eaton DK, Lowry R, Croft JB, Presley-Cantrell L, et al. (2011) Relationships between hours of sleep and health-risk behaviors in US adolescent students. Preventive medicine 53(4-5): 271-273.
- Van den Bulck J (2003) Text messaging as a cause of sleep interruption in adolescents, evidence from a cross‐sectional study. Journal of Sleep Researc 12(3): 263.
- Van den Bulck J (2004) Television viewing, computer game playing, and Internet use and self-reported time to bed and time out of bed in secondary-school children. Sleep 27(1): 101-104.
- Zhou HQ, Shi WB, Wang XF, Yao M, Cheng GY, et al. (2012) An epidemiological study of sleep quality in adolescents in South China: a school‐based study. Child: care, health and development 38(4): 581-587.
- Ismail DM, Mahran DG, Zarzour AH, Sheahata GA (2017) Sleep quality and its health correlates among Egyptian secondary school students. Journal of Social, Behavioral, and Health Sciences 11(1):5.2
- Buysse DJ, Reynolds III CF, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry research 28(2): 193-213.
- Suleiman KH, Yates BC, Berger AM, Pozehl B, Meza J (2010) Translating the Pittsburgh sleep quality index into Arabic. Western Journal of Nursing Research 32(2): 250-68.
- Gradisar M, Gardner G, Dohnt H (2011) Recent worldwide sleep patterns and problems during adolescence: a review and meta-analysis of age, region, and sleep. Sleep medicine 12(2):110-8.
- Dijk DJ, Duffy JF, Czeisler CA (2000) Contribution of circadian physiology and sleep homeostasis to age-related changes in human sleep. Chronobiology international 17(3): 285-311.
- Voderholzer U, Al‐Shajlawi A, Weske G, Feige B, Riemann D (2003) Are there gender differences in objective and subjective sleep measures? A study of insomniacs and healthy controls. Depression and anxiety 17(3): 162-72.
- Munezawa T, Kaneita Y, Osaki Y, Kanda H, Minowa M, et al. (2011) The association between use of mobile phones after lights out and sleep disturbances among Japanese adolescents: a nationwide cross-sectional survey. Sleep 34(8): 1013-1020.
- Liu X, Zhao Z, Jia C, Buysse DJ (2008) Sleep patterns and problems among Chinese adolescents. Pediatrics 121(6): 1165-1173.
- Haseli-Mashhadi N, Dadd T, Pan A, Yu Z, Lin X, et al. (2009) Sleep quality in middle-aged and elderly Chinese: distribution, associated factors and associations with cardio-metabolic risk factors. BMC Public Health 9(1): 130.
- Cheng SH, Shih C-C, Lee IH, Hou Y-W, Chen KC, et al. (2012) A study on the sleep quality of incoming university students. Psychiatry research 197(3): 270-274.
- Bidulescu A, Din-Dzietham R, Coverson DL, Chen Z, Meng Y-X, et al. (2010) Interaction of sleep quality and psychosocial stress on obesity in African Americans: the Cardiovascular Health Epidemiology Study (CHES). BMC Public Health 10(1): 581.
- Hung HC, Yang YC, Ou HY, Wu JS, Lu FH, et al. (2013) The association between self‐reported sleep quality and overweight in a Chinese population. Obesity 21(3): 486-492.
- Stea T, Knutsen T, Torstveit M (2014) Association between short time in bed, health-risk behaviors and poor academic achievement among Norwegian adolescents. Sleep medicin 15(6): 666-671.
- Ohida T, Osaki Y, Doi Y, Tanihata T, Minowa M, et al. (2004) An epidemiologic study of self-reported sleep problems among Japanese adolescents. Sleep 27(5): 978-985.
- Jaehne A, Unbehaun T, Feige B, Lutz UC, Batra A, et al. (2012) How smoking affects sleep: a polysomnographical analysis. Sleep medicine 13(10): 1286-1292.
- Lemola S, Perkinson-Gloor N, Brand S, Dewald-Kaufmann JF, Grob A (2015) Adolescents’ electronic media use at night, sleep disturbance, and depressive symptoms in the smartphone age. Journal of youth and adolescence 44(2): 405-418.
- Canan F, Yildirim O, Sinani G, Ozturk O, Ustunel TY, et al. (2013) Internet addiction and sleep disturbance symptoms among Turkish high school students. Sleep and Biological Rhythms 11(3): 210-213.
- Arora T, Broglia E, Thomas GN, Taheri S (2014) Associations between specific technologies and adolescent sleep quantity, sleep quality, and parasomnias. Sleep medicine 15(2): 240-247.
- Yang YS, Yen JY, Ko CH, Cheng CP, Yen CF (2010) The association between problematic cellular phone use and risky behaviors and low self-esteem among Taiwanese adolescents. BMC Public Health 10(1): 217.
- White AG, Buboltz W, Igou F (2011) Mobile phone use and sleep quality and length in college students. International Journal of Humanities and Social Science 1(18): 51-58.
- Lund HG, Reider BD, Whiting AB, Prichard JR (2010) Sleep patterns and predictors of disturbed sleep in a large population of college students. Journal of adolescent health 46(2): 124-132.
- Chen MY, Wang EK, Jeng YJ (2006) Adequate sleep among adolescents is positively associated with health status and health-related behaviors. BMC Public Health 6(1): 59.
- Ortega FB, Chillón P, Ruiz JR, Delgado M, Albers U, et al. (2010) Sleep patterns in Spanish adolescents: associations with TV watching and leisure-time physical activity. European journal of applied physiology 110(3): 563-573.
- Al‐Hazzaa H, Musaiger A, Abahussain N, Al‐Sobayel H, Qahwaji D (2014) Lifestyle correlates of self‐reported sleep duration among Saudi adolescents: a multicentre school‐based cross‐sectional study. Child: care, health and development 40(4): 533-542.
- Foti KE, Eaton DK, Lowry R, McKnight-Ely LR (2011) Sufficient sleep, physical activity, and sedentary behaviors. American journal of preventive medicine 41(6): 596-602.
- Gellis LA, Lichstein KL (2009) Sleep hygiene practices of good and poor sleepers in the United States: an internet-based study. Behavior Therapy 40(1): 1-9.
- Jefferson CD, Drake CL, Scofield HM, Myers E, McClure T, et al. (2005) Sleep hygiene practices in a population-based sample of insomniacs. Sleep 28(5): 611-615.
- Al-Disi D, Al-Daghri N, Khanam L, Al-Othman A, Al-Saif M, et al. (2010) Subjective sleep duration and quality influence diet composition and circulating adipocytokines and ghrelin levels in teen-age girls. Endocrine journal 57(10): 915-923.
- Nedeltcheva AV, Kilkus JM, Imperial J, Kasza K, Schoeller DA, et al. (2008) Sleep curtailment is accompanied by increased intake of calories from snacks–. The American journal of clinical nutrition; 89(1): 126-33.
- Chaput JP (2014) Sleep patterns, diet quality and energy balance. Physiology & behavior 134: 86-91.
- Garaulet M, Ortega F, Ruiz J, Rey-Lopez J, Beghin L, et al. (2011) Short sleep duration is associated with increased obesity markers in European adolescents: effect of physical activity and dietary habits. The HELENA study. International journal of obesity 35(10): 1308-1317.
- Mindell JA, Meltzer LJ, Carskadon MA, Chervin RD (2009) Developmental aspects of sleep hygiene: findings from the 2004 National Sleep Foundation Sleep in America Poll. Sleep medicine 10(7): 771-779.
- Drescher AA, Goodwin JL, Silva GE, Quan SF (2011) Caffeine and screen time in adolescence: associations with short sleep and obesity. Journal of Clinical Sleep Medicine 7(04): 337-342.
-
Vladimir A Mikhaylov. Intravenous Laser Therapy in the Complex Treatment of Nervous System and Brain Diseases and the New Development Mechanism of the Diseases. Arch Neurol & Neurosci. 11(4): 2021. ANN.MS.ID.000768.
-
Sleep quality; Lifestyle correlates; Secondary schools, napping, cognitive restitution, learning, decision making, memory consolidation, weight gain, obesity, daytime sleepiness, exhaustion, impaired glucose tolerance and diabetes, depression and anxiety, impaired memory, and higher risk of motor vehicle accidents.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






