 Research Article
Research Article
Psychophysiological Features of Primary Headache: New Findings and Some Confirmation
Pruneti C1*, Guccini I1 and Torelli P2
1Department of Medicine and Surgery, University of Parma, Italy
2Department of Medicine and Surgery, Unit of Neurology, University of Parma, Italy
Carlo Pruneti, Department of Medicine and Surgery, Clinical Psychology, Clinicaql Psychophysiology and Clinical Neuropsychology Labs. University of Parma, Italy.
Received Date: April 29, 2020; Published Date: May 26, 2020
Abstract
Primary headaches are heterogeneous clinical conditions, characterized by multifactorial etiology and partially unknown eziopathogenesis. In this study, we have investigated the psychophysiological aspects related to autonomic activation and psycho physiological stress response in primary headache patients, in order to identify possible statistically significant relationships between psycho physiological pattern, measured by the PPP (psycho physiological profile) , and the differential neurological diagnosis of primary headaches.The sample consisted of 68 subjects aged between 18 and 70 years (Mean= 39,6; S.D.=12,1), who underwent continuous and simultaneous psycho physiological registration (PPP) of the following parameters: surface electromyography (sEMG), skin conductance level/response (SCL/SCR), heart rate (HR), Inter Beat Interval (IBI) and peripheral temperature (THE).The statistical analysis, performed using non parametric tests, since the data was non-normally distributed, on average showed that: the whole sample reveals already in baseline, an autonomic hyper activation that continues throughout the registration; the category of migraine with aura seems to be physiologically less activated compared to the other diagnostic categories identified.Moreover, we did not detect significant correlations between psycho physiological pattern and clinical neurological diagnosis.In conclusion, it seems reasonably possible to state that these clinical conditions are strongly influenced by stress reaction and management, as an important variable in the disease pathogenesis. This typical stress reaction seems also to have an important role in the disease maintenance and/or worsening, though the strong intra-individual variability.
Keywords: Primary-idiopathic headaches;Psychophysiology;Biofeedback; Neurovegetative activation;Stress response
Introduction
According to the guidelines of the International Headache Society beta version (IHS, 2013), headache can be distinguished in:
• Primary or primitive-idiopathic, not supported by any traceable and / or underlying pathological condition; (traumatic, neoplastic, febrile).
• Secondary or symptomatic, linked to pathologies that have headache symptoms (eg intracranial or systemic).Tra le cefaleeprimario-idiopatiche, la cefalea di tipotensivo (CTT) e l’emicraniasenz’aurarappresentano le categoriepiùfrequenti, considerate patologieadeziologia incerta, caratterizzate da multifattorialità e multicausalità [1,2].
Tension-type headache is the most frequent (90%) of headaches, characterized by severe-constricting head pain, sometimes associated with an increase in the tone of the head and / or neck muscles; pain, non-throbbing, is frequently bilateral, typically mild or moderate.In migraines, the headache is unilateral, pulsating in nature, with a duration that can vary from 2 to 72 hours. Associated symptoms can include nausea, vomiting, photophobia (increased sensitivity to light), phonophobia (increased sensitivity to sound). Pain generally worsens as a result of physical activity. Up to a third of people with migraines experience the aura: a transient visual, sensory, motor or speech disorder that just precedes the occurrence of a headache episode.One of the factors recognized as important in the exacerbation and maintenance of the disorder appears to be psychophysiological stress, a chronic and non-adaptive alteration of the individual’s neurovegetative homeostatic balance, strictly interconnected with a dysfunctional stress management deriving from stimuli present in daily life [3,4].
Headaches present a wide spectrum of clinical manifestations with very varied etiological and symptomatic characteristics. The clinical approach therefore requires in-depth assessment work useful for formulating a correct differential diagnosis with the forms of secondary headaches attributable to organic pathologies. From a psychic point of view, headaches frequently have important psychological connotations: it is in fact known [5,6] that some forms of headache can be an expression of mental disorders such as anxiety or depression.
These are clinical pictures with a predominantly somatic expression, which is why it becomes difficult to establish their clinical autonomy and identify a unique cause [Pellegrino, 2008].However, some precise dysfunctional mechanisms have been identified, such as an excessive sensitivity and excitability of the nociceptive nervous system, fueled by other factors of the psychophysiological area.It is also described an electrophysiological phenomena named “Cortical Spreading Depression” (CSD), a sudden wave of excitement of the neurons of the cerebral cortex followed by an equally rapid “shutdown” that begins at the level of the occipital lobe of the brain, the area where the vision is located, and then propagates anteriorly towards the sensitive and motor areas [7].
According to Pellegrino (2008), in cephalalgic patients there would be an interruption of the physiological and psychological adaptive systems as a manifestation of an altered adaptive response to stress. The daily life distress would induce the individual to seek adequate adaptation responses to preserve biological homeostasis by creating a vicious circle of the “stress-headache-stress” type [8].
The multiplicity of psychological, physiological, social and economic aspects salient in primary headaches, therefore, make it difficult, if not contraindicated, to approach only a single disciplinary area. Specifically, the properly psychophysiological analysis of primary headaches in the literature turned to the study of variables susceptible to empirical verification such as: vulnerability and stress responses, coping styles, neurovegetative regulation, making it clear that different are the psychophysiological parameters involved in development and maintenance of headaches, such as: high levels of sEMG (surface electromyography), THE (peripheral temperature) and BVP (peripheral vasodilation) [9].
In particular, among the pathogenetic mechanisms of tension-type headache (CTT), two aspects are considered fundamental: muscle tension, understood as an increase in the tone of pericranial muscles and the psychological component [10]. Recently, a considerable number of studies suggest the existence of a neurobiological basis: it is, in fact, common opinion that pericranial muscles in CTT are more contracted than the values normally assumed, a conviction that the latter is so widespread that the previous terminology referred to these syndromes with the name of muscle tension headache, thus underlining the muscular implication in the pathogenesis [3]. It is known [5,11,12] that the onset of numerous forms of primary headache can be considered as the result of the action of psycho-social factors (conflicts family, work stress, emotional crises), cyclic hormonal changes (especially related to the female sex), geoclimatic (e.g. changes in external temperature), autonomic (related to the response of pain) on a personality with a low pain threshold (susceptibility cephalalgic): that is, there would be an individual vulnerability to develop cephalalgic clinical pictures together with a natural “physiological acceleration” which translates into a lifestyle characterized by disordered and long-term maladaptive responses; hence the need for an integrated psychosomatic as well as biopsychosocial approach (Pini, 2006).
To conclude, it is necessary to develop multidimensional and multidisciplinary assessment procedures in which to include the assessment of basic psychophysiological activity and subjective reactivity to stress through indicators of psychophysiological activation [13-16]. For this purpose and in the light of the literature examined that was found to be lacking in research aimed at the specific assessment of the psychophysiological structure in primary headaches, the present study aims to investigate the existence of correlations and / or associations between the different subcategories of primary headaches and the psychophysiological trend measured by Psychophysiological Profile (PPP) on a sample of subjects with neurological diagnosis of primary headache [17].
Sample and patient selection
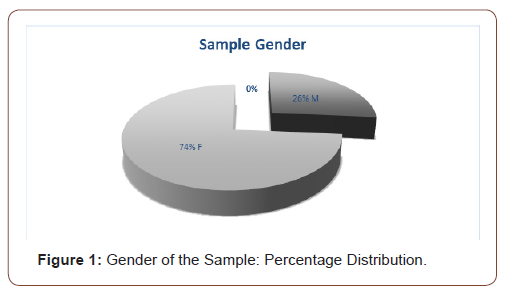
68 subjects (18 men and 50 women), aged between 18 and 70 (Average age = 39.6; SD = 12.1) were subsequently recruited through consecutive sampling, within the Headache Center of the University Hospital of Parma (Figure1). All subjects voluntarily participated in the study by signing a written consent which safeguarded privacy and which explained that the interview and the short psychological questionnaires an psychophysiological test would only slightly extend the time dedicated to usual medical visits. All subjects accepted with pleasure to participate in the research. At the end of the observation, there was an interview, carried out individually between the subject and a clinical psychologist for the discussion of the results that emerged from the reports of the tests carried out.
Inclusion/exclusoion criteria
Subjects presenting with cognitive deficits or degenerative diseases, psychiatric diseases confirmed by documented medical diagnosis, organic neurological damage were excluded. Furthermore, for the purposes of this research, data relating to foreign people with poor understanding of the Italian language have been excluded.
Material and Methods
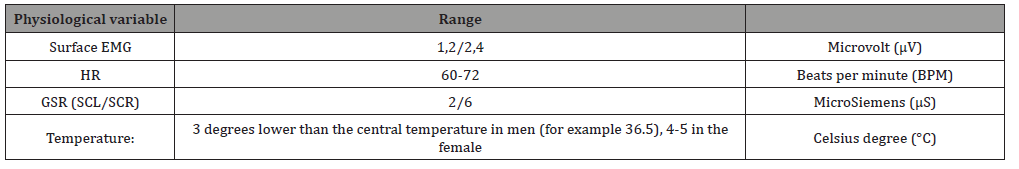
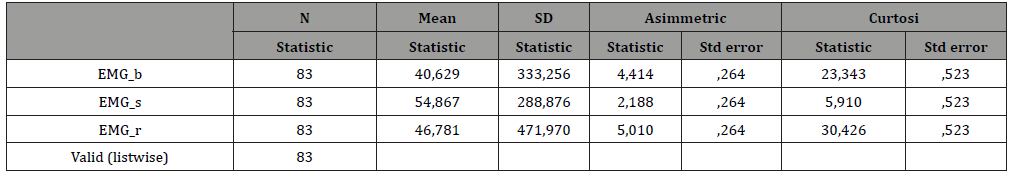
The assessment of the neurovegetative aspects was carried out through the use of the Satem®Physiolab system for the recording of psychophysiological data during the Psychophysiological Stress Profile (PPP), an assessment procedure which consists in measuring multiple psychophysiological signals continuously and simultaneously [13]. The parameters registered were: surface electromyography (sEMG) (μV, microvolt), for detecting the tension of the head and neck muscles by means of 3 recording electrodes placed in correspondence of the frontal muscle; Skin conductance (SCR / SCL) (μS, microSiemens) for the electro-galvanic response of the skin, detected by Ag / ACl electrodes positioned on the distal phalanges of the first and second fingers of the dominant hand; Peripheral temperature (pTHE) (C°, degrees centigrade), detected by means of a thermistor applied to the tenar eminence of the palm of the non-dominant hand. Heart rate (HR) measured in beats per minute (BPM) and Interval Beat (IBI), detected by means of electrodes placed on the non-dominant forearm. According to Fuller (1979) the registration of the PPP is carried out in three distinct moments: in the first phase, following a period of adaptation and stabilization of the signal, it records the basic activation for a duration of 6 minutes; follows a phase of stress induced by objectively stressful tasks consisting, for example, of mathematical tasks (Mental Arithmetic Task, MAT) lasting 4 minutes; finally, a 6-minute recovery phase is foreseen in which it is possible to monitor the homeostatic recovery capacity (Table 1) [18].
Table 1:Expected normal values [18].
For the evaluation of psychological and behavioral variables, the Cognitive Behavioral Assesment 2.0 (Hawton, Salkovskis, Kirk, Clark, 1989) was used, a test battery, consisting of ten scales, including one of them, card 4, is useful for the collection of anamnestic data relating to family history, life habits and the presence or absence of traumatic or in any case particularly salient events in the life of the person who completes the battery.
Statistical Analysis and Results
Table 2:Mean values GSR.
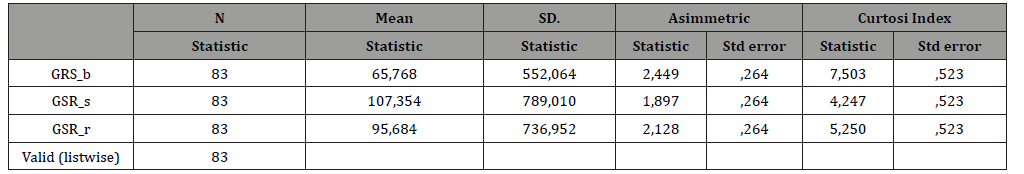
Table 3:Mean values Thermal.

Table 4:Mean Values HR.
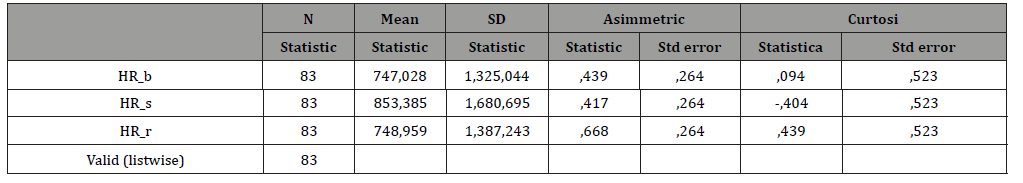
Table 5:Mean values EMG.
The data were processed using the IBM SPSS Statistic 21.0 package supplied by the University of Parma.
The descriptive statistics and the normality tests of the parameters showed a non-normal distribution, therefore nonparametric statistics were used for subsequent analyzes. For each individual subject, the means of each parameter of the PPP were calculated in the three moments: at rest, during the administration of mental stress, in recovery (Table 2-5).
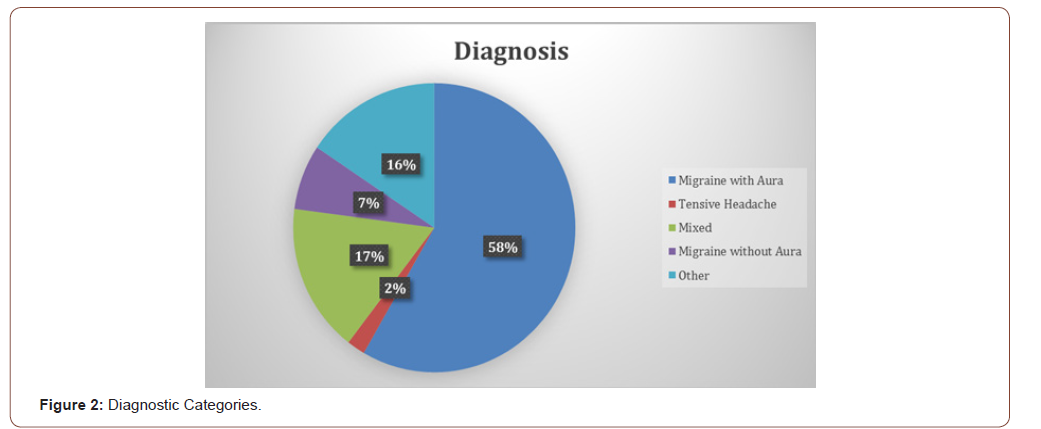
The main diagnostic categories were identified and sorted, according to frequency, as follows: 1 = aura without migraine; 2 = tension-type headache; 3 = migraine tension headache; 4 = migraine with aura; 5 = other (post-coitum headache or linked to sexual activity, of the weekend, stabbing, aura without migraine, connected to the menstrual cycle, from drug overuse), see Figure 2.
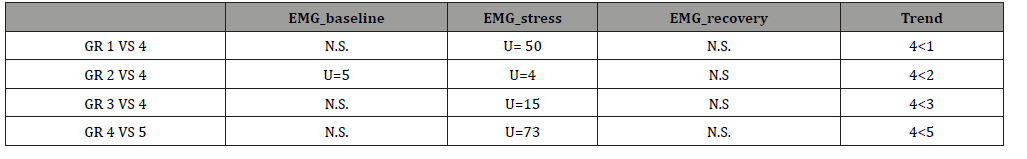
Subsequently, pairwise comparisons were made for independent samples between EMG, HR, GSR, THE values in the three moments and the different diagnostic categories using the Mann-Whitney nonparametric U test.The average values of the PPP parameters are higher than the normative values assumed [18] in the sample of patients with primary headache, already in baseline (baseline) while recovery is often slow or absent. Specifically, for 68% of the participants there was a baseline GSR value greater than 6 μS and differentiating by diagnostic category it was higher in group 5, followed by group 3, 4, 1 and finally 2.In addition, sEMG values greater than 2.4 μV were detected for 99% of the participants with higher levels for group 2, followed by group 1, then 5, 3 and finally group 4 (Table 6-9).
Table 6:Mean values sEMG.
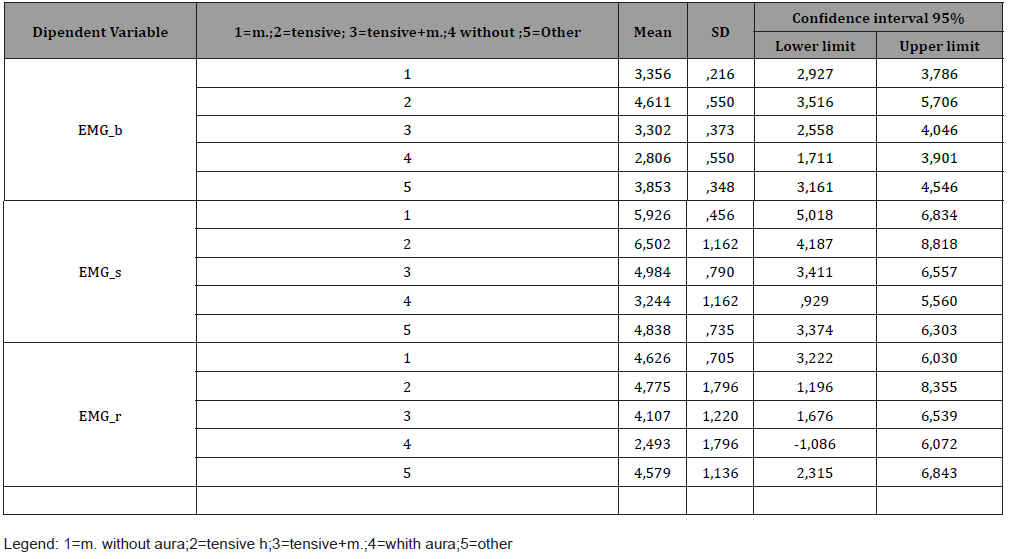
Table 7:Means values GSR.
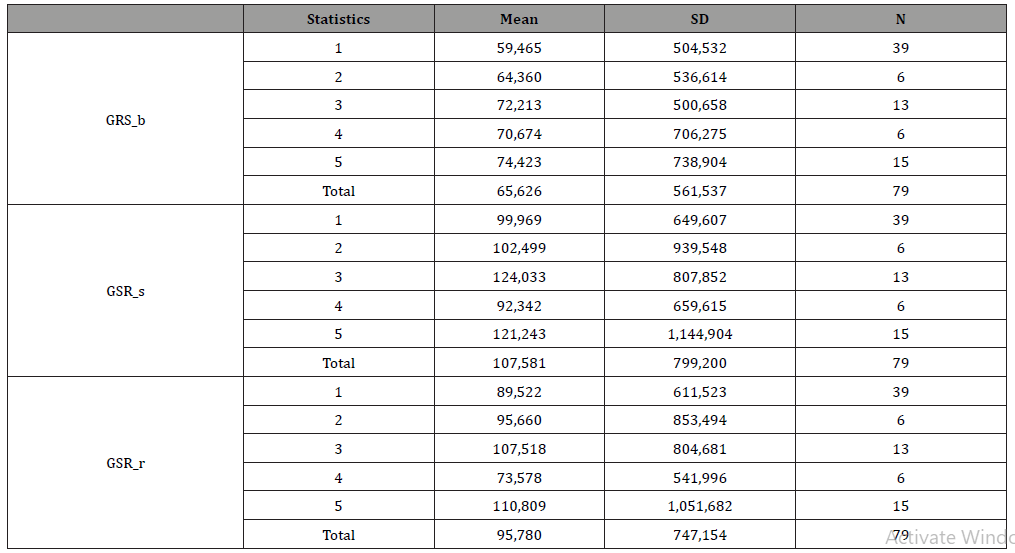
Table 8:Thermal Meams values.
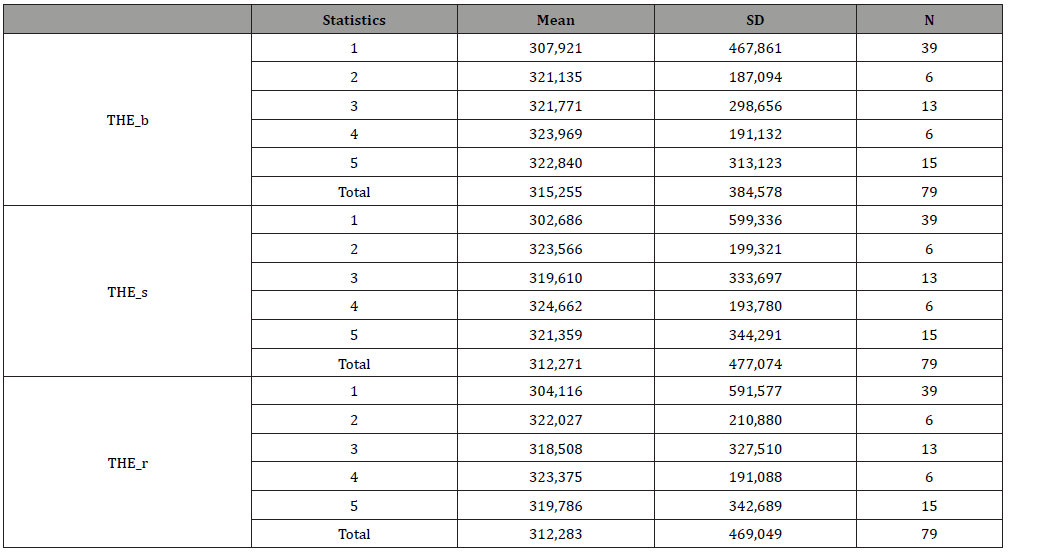
Table 9:HR Means values.
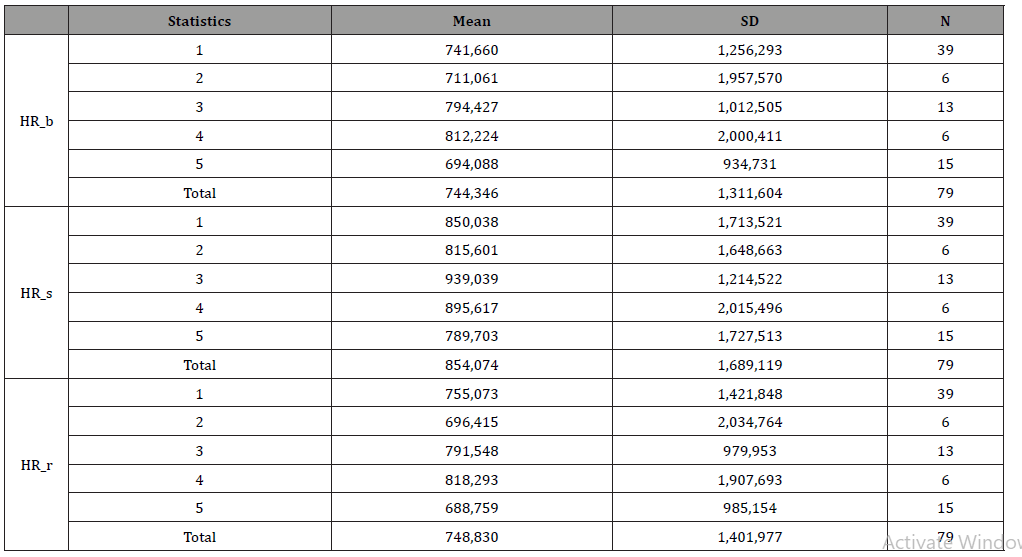
Table 10:Average values of the psychophysiological profile.
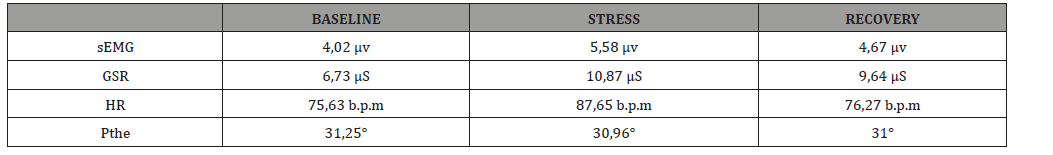
As regards peripheral temperature, unlike expectations, during stress, and with an increase in skin conductance values, there is either a slight increase in peripheral temperature values, or, more generally, a flat trend and rarely to an active constricting vessel phenomenon (Table 10).
Futhermore, by using the Mann-withney U test (Table 9), pairwise comparisons were made between diagnostic categories with respect to the psychophysiological indices: it was found that the group of migraines with aura was less activated than the other diagnostic categories identified as regards the EMG both in baseline than in stress (Table 11).
Table 11:Mann-Whitney’S U Test,
At the end, a correlation analysis was carried out using the Tau-B DI Kendal test but did not reveal any significant correlation between the measurements detected during the Psychophysiological registration and the diagnostic categories. Instead, statistically significant correlations were found between the obtained QPF scores and the STAI X1 scores (ρ,000 per p <.01). Furthermore, a statistically significant negative correlation was found between EPQ/RE and STAI X1 (ρ.047 for p <.05), that’s probably mean that, in our sample when the extroversion values increase, the trait anxiety values decrease.
Discussion and Conclusions
The data emerging from this research highlight important trends which it is necessary to discuss in greater detail, in order to then use them as possible guidelines for future studies. During the first interviews, many patients report suffering from widespread painful forms, essential hypertension or tachycardia and, therefore, they follow specific treatments with beta-blockers and / or cardioaspirin, In addition, many complain of sleep disorders and problems related to anxiety: already in an initial anamnestic phase shows general dysfunctional and maladaptive psychophysical conditions.The analysis of the medical records containing the medical-neurological diagnostic indications highlights a constant tendency in reporting and describing cephalalgic and noncephalalgic symptoms, with a propensity to amplify the symptoms themselves which is confirmed by the high scores obtained in the CBA QPF.
The majority of the sample presents forms of migraine without aura and is predominantly female. Such evidence suggests that the genetic-hormonal implications of migraine are strong.An important dysregulation in terms of thermoregulation was better observed in female subjects and, even more, among those in menopause, a factor implicated in the exacerbation of the cephalalgic attack, also in conjunction with changes in external / environmental temperature. This would confirm that common migraineurs (without aura) have a highly excitable central nervous system, behavior characterized by greater attention to sensory stimuli and an increased ability to identify simple stimuli from the surrounding environment as threats. Hence the neurovegetative hyperaurosal recorded during the psychophysiological assessment in the subjects of the Primary Headache sample.
The majority of the sample presents forms of migraine without aura and is predominantly female. Such evidence suggests that the genetic-hormonal implications of migraine are strong.An important dysregulation in terms of thermoregulation was better observed in female subjects and, even more, among those in menopause, a factor implicated in the exacerbation of the cephalalgic attack, also in conjunction with changes in external / environmental temperature. This would confirm that common migraineurs (without aura) have a highly excitable central nervous system, behavior characterized by greater attention to sensory stimuli and an increased ability to identify simple stimuli from the surrounding environment as threats. Hence the neurovegetative hyperaurosal recorded during the psychophysiological assessment in the subjects of the Primary Headache sample.
The research hypothesis has not been confirmed from a statistical point of view: no significant relationships have emerged between the performance of the PPP and diagnostic categories that allow the identification of specific patterns related to both the neurological differential diagnoses and the recorded neurovegetative activation.The data emerged strongly support the etiopathogenic multifactorial nature of the disorder and the fact that autonomic and neurovegetative dysregulations play a role in the etiopathogenesis of primary headaches [20-25].
Many disorders of uncertain etiology are strongly influenced by neurovegetative activity and the psychophysiological stress response. By integrating this assumption with the data obtained from the PPP of cephalalgic patients, it is suggested that the different diagnoses of primary headaches do not seem to bring with them specific patterns of neurovegetative activation or to be predictive of the psychophysiological structure of that given diagnostic category. Rather, it seems that, given the stress-related characteristics that emerged and the hyper-activation at the neurovegetative level of these patients, headaches can be interpreted as a functional disorder proper: this would be confirmed by the evident alterations of the PPP, typical also of other non-adaptive profiles, albeit not related to primary headaches and, in part, from the results obtained in some psychometric tests, in particular precisely in trait anxiety, in extroversion and in psychophysiological or psychosomatic symptoms[26-31].
In light of the obtained results, it can be concluded that there is a significant neurovegetative dysregulation and in the management of the stress response, factors capable of triggering, exacerbating and / or aggravating the various cephalalgic conditions.The limits of this study are different, mainly related to the small size of the sample, and the absence of a control group. In order to remedy the weight of this second factor, the collected data were compared and evaluated with the reference values deriving from the literature and relating to the PPP [18]. Despite the limitations, important methodological and design indications are obtained and, therefore, the development of further research on the population characterized by primary headache is suggested in which, in addition to considering more representative samples from the numerical point of view, the inclusion criteria can be improved, and study methods of statistical treatment of useful data on the one hand to improve the definition of categorical characteristics and on the other to improve the evaluation of indices of intra-individual variations[32-37].
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Moskovitz MA (2007) Pathophysioloy of headaches: past and present. Headaches 47: 58-63.
- Bussone G, Casucci G, Frediani F, Manzoni GC, Bonavita V ( 2008) Le cefalee: manuale teorico pratico. Milano. Springer-Verlag.
- Leistad RB, Sand T, Westgaard RH, Nilsen KB, Stovner LJ (2005) Stress-induced pain and muscle activity in patients with migraine and tension-type headache. Cephalalgia 26(1): 64-73.
- De Leeuw R, Schmidt JE, Charles RC (2005) Traumatic Stressors and Post-Traumatic Stress Disorder Symptoms in Headache Patients. Headache. The Journal of Head and Face Pain 45(10): 1365-1374.
- Nicholson RA, Houle TT, Rhudy JL, Norton PJ (2007) Psychological Risk Factors in Headache. Headache. The Journal of Head and Face Painc 47(3): 413-426.
- Boz C, Velioglu S, Ozmenoglu M, Sayar K, Alioglu Z, et al. (2004) Temperament and character profiles of patients with tension-type headache and migraine. Psychiatry and Clinical Neurosciences 58 (5): 536-543.
- Andrew CC, Serapio MB (2013) Cortical spreading depression and migraine. Nature Reviews Neurology 9: 637-644.
- Fanciullacci M, Alessandri M (2003) Le cefalee primarie nella pratica clinica. Firenze. SEE Editrice.
- Holroyd KA, O'Donnell FJ, Stensland M, Lipchik GL, Cordingley GE, et al. (2001) Management of chronic tension-type headache with tricyclic antidepressant medication, stress management therapy, and their combination: a randomized controlled trial. Journal published by the American Medical Association 285: 2208-2215.
- Bendtsen L, Fernández-de-la-Peñas C (2011) The Role of Muscles in Tension-Type Headache. Current Pain and Headache Reports 15(6): 451-458.
- Kröner Herwig B, Morris L, Heinrich M (2008) Biopsychosocial Correlates of Headache: What Predicts Pediatric Headache Occurrence? Headache: The Journal of Head and Face Pain 48(4): 529-544.
- Crocetti A, Merati S, Menotti R, Forti S, Aiello G (2011) PsychoPhysiological stress profile: a protocol to differenziate normal Vs Pathological Subjects. Activitas nervosa Superior Rediviva 52(4): 241-245.
- Pruneti C, Cosentino C, Sgromo M, Innocenti A (2014) Skin Conductance Response as a decisive variable in individuals with a DSM-IV TR Axis I diagnosis. JMED Res. 565009.
- Pruneti C, Saccò M, Cosentino C, Sgromo D (2016) Relevance of Autonomic Arousal in the Stress Response in Psychopathology. Journal of Basic & Applied Sciences 12: 176-184
- Pruneti CA, Fontana F, Fante C, Carrozzo E (2010) Autonomic changes and stress responsess diagnosis in psychopathology. European Journal of Clinical Psychologyand Psychiatry 3: 1-20.
- Pruneti CA, Lento RM, Fante C, Carrozzo E, Fontana F (2010) Autonomic arousal and differential diagnosis in clinical psychology and psychopathology. Journal of Psychopathology 16: 43-52.
- Ah Young Kim, Eun Hye Jang, Seunghwan Kim, Kwan Woo Choi, Hong Jin Jeon, et al. (2018) Automatic detection of major depressive disorder using electrodermal activity. Scientific Reports 8: 17030
- Khazan IZ (2013) Psychophysiological Stress Profile. The clinical Handbook of Biofeedback.
- Jensen R, Rasmussen BK, Pedersen B, Lous I, Olesen J (1993) Prevalence of oromandibular dysfunction in a general population. Pain 7(2): 175-182.
- Peroutka SJ (2004) Migraine: A Chronic Sympathetic Nervous System Disorder. Headache: The Journal of Head and Face Pain 44 (1): 53-64.
- Borkum J (2014) Chronic Headaches: Biology, Psychology, and Behavioral Treatment. Psychology Press.
- Drummond PD (1988) Dysfunction of the sympathetic nervous system in cluster headache. Cephalalgia 8: 181-186.
- Headache Classification Subcommittee of the International Headache Society (2013) The international classification of headache disorders, 3rd edition (beta version). Cephalalgia 33(9): 629-808.
- Holroyd KA, Nash JM, Pingel JD, Cordingley GE, Jerome AJ (1991) A comparison of pharmacological (Amitriptyline HCL) and nonpharmacological (cogntive-behavioral) therapies for chronic tension headaches. Journal of Consulting and Clinical Psychology 59: 387-393.
- Holroyd KA, Penzien DB (1990) Pharmacological versus non-pharmacological prophylaxis of recurrent migraine headache: a meta-analytic review of clinical trials. Pain 42(1): 1-13.
- Martin PR, Marie GV, Nathan PR (1992) Psychophysiological mechanisms of chronic headaches: investigation using pain induction and pain reduction procedures. J Psychosom Res 36(2): 137-148.
- Martin PR (1993) Psychological management of chronic headaches. New York: Guilford Press, USA.
- Martin PR (2009) Psychological management. In: P Selvaratnam, K Niere, M Zuluaga, (Eds.), Headache, orofacial pain and bruxism. Edinburgh, UK: Churchill Livingstone Elsevier, UK, pp. 2720087-288.
- Martin PR (2013) Psychological management of the common primary headaches. In: ML Caltabiano, LA Ricciardelli, (Eds.), Applied topics in health psychology. Wiley-Blackwell, USA, pp. 462-476.
- Martin PR, MacLeod C (2009) Behavioral management of headache triggers: Avoidance of triggers is an inadequate strategy. Clinical Psychology Review 29: 483-495.
- Martin PR, Forsyth MR, Reece J (2007) Cognitive-behavioral therapy versus temporal pulse amplitude biofeedback training for recurrent headache. Behavior Therapy 38: 350-363.
- Moss D (2004) Adjunctive interventions and assessment. In: A Crider, DD Montgomery (Eds.), Association for Applied Psychophysiology and Biofeedback.
- Nicholson RA, Buse DC, Andrasik F, Lipton RB (2011) Nonpharmacologic treatments for migraine and tension-type headache: how to choose and when to use. Curr Treat Options Neurol 13(1): 28-40.
- Oam PRM (2016) Psychological assessment and treatment of chronic headaches. InPsych 38(4).
- Olesen J, Goadsby PJ, Ramadan NM, Tfelt-Hansen P, Welch KMA (2006) The headaches (3rd ed.). Philadelphia: Lippincott Williams & Wilkins, USA.
- Rains JC, Penzien DB, McCrory DC, Gray RN (2005) Behavioral headache treatment: History, review of the empirical literature. and methodological critique. Headache 45(S2): S92-S109.
- Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, et al. (2015) A classification of chronic pain for ICD-11. Pain 156(6): 1003-1007.
-
Pruneti C, Guccini I, Torelli P. Psychophysiological Features of Primary Headache: New Findings and Some Confirmation. Arch Neurol & Neurosci. 8(1): 2020. ANN.MS.ID.000676.
-
Primary-idiopathic headaches; Psychophysiology; Biofeedback; Neurovegetative activation; Stress response
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






