 Case Report
Case Report
Fahr Syndrome with Fluctuation in Consciousness and Temporary Vision Loss
Ozkara B*, Ozcan M and Budak F
Department of Neurology, Alanya University and Kocaeli University, Turkey
Buket Özkara, Department of Neurology, Alanya University and Kocaeli University, Turkey.
Received Date: December 05, 2019; Published Date: December 13, 2019
Abstract
Fahr syndrome, also known as bilateral striatopallidodentate calcinosis is a rare neurological disorder, characterized by abnormal vascular calcium deposits in the basal ganglia, cerebellar dentate nuclei and white matter [1,2]. Symptoms may contain deterioration of motor function, movement disorders like parkinsonism, Korea and athetosis, dementia, ataxia, seizures, headache, dysarthria, spasticity and psychiatric disorders. The major differential diagnosis includes hypoparathyroidism [2]. Here, we report a case of Fahr’s syndrome with calcification of the basal ganglia caused by hypoparathyroidism in a patent with fluctuation in consciousness and temporary vision loss.
Keywords: Fahr Syndrome; Loss of consciousness; Vision loss; Hypoparathyroidism
Introduction
Fahr syndrome, also known as bilateral striatopallidodentate calcinosis is a rare neurological disorder, characterized by abnormal vascular calcium deposits in the basal ganglia, cerebellar dentate nuclei and white matter. Diagnostic criteria of Fahr’s disease are as follows: bilateral calcification of the basal ganglia on neuroimaging, progressive neurologic dysfunction, absence of biochemical abnormalities, and family history consistent with autosomal dominant inheritance r The term Fahr’s disease is used when primary familial brain calcification is present, and the term Fahr’s syndrome is used for secondary causes, Secondary causes include calcium metabolism disorders, endocrinopathies hypoparathyroidism, pseudohypoparathyroidism, autoimmune diseases vasculitis, infections. Symptoms may contain deterioration of motor function, movement disorders like parkinsonism, Korea and athetosis, dementia, ataxia, seizures, headache, dysarthria, spasticity and psychiatric disorders. Movement disorders, especially parkinsonism is the most common presentation followed by cognitive impairment and ataxia.
Case Report
A 65-year-old woman was admitted us because of repeated episodes of transient loss of consciousness and minimal cognitive and behavioral disturbances. She did not have a history of head trauma, central nervous system infection, stroke, hypertension, diabetes, thyroid disease, or autoimmune disease. On physical examination, the patent was uncooperative and agitated. Neurological exam revealed brisk patellar reflexes and an unsteady gait but was otherwise normal. The patent developed bilateral vision loss during clinical follow-up and visual loss lasted for about one hour. Ophthalmological examinations were evaluated as normal. Visual acuity was 0 Visual field examination revealed no loss. On ophthalmologic examination, optic disc and vessels were observed naturally.
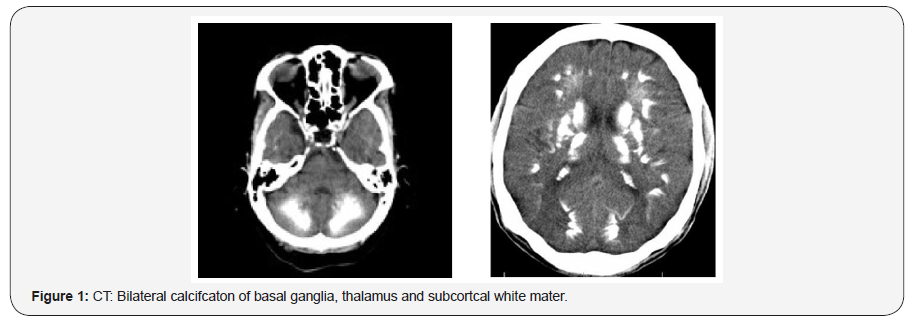
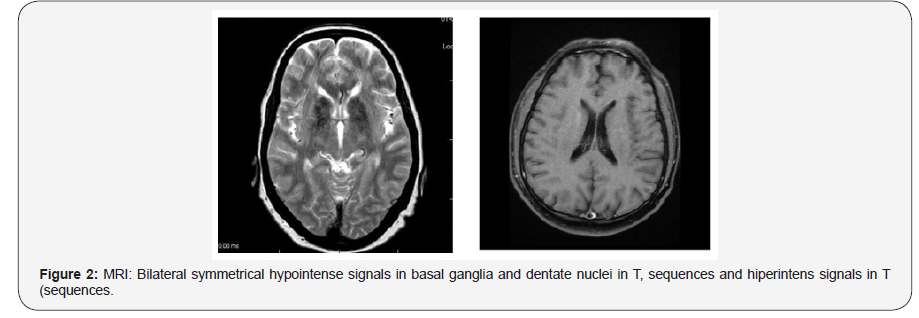
Noncontract computed tomography CT2 of the brain showed bilateral, extensive, and dense calcifications involving the dentate nuclei and basal ganglia with preserved cerebral and cerebellar hemispheres picture. Brain MRI showed bilateral symmetrical hypointense signals in basal ganglia and dentate nuclei in T, sequences (Figure 1 & 2).
Laboratory investigations revealed a normal hemoglobin, lipid profile, glucose, iron, ferritin, HbA (c, and electrocardiogram. Liver, kidney, and thyroid function tests were all normal. Her serum calcium indicate persistent hypocalcemia total serum calcium 6r5 [normal 9–(0r5] mg/ (00 mL2 while serum parathyroid hormone was 4r0 [normal –7, pg/mL2 consistent with primary hypoparathyroidism. The patent’s reduced parathyroid hormone levels committed hypocalcemia due to hypoparathyroidism. Primary hypoparathyroidism was diagnosed because there were no evidences of secondary causes such as a history of congenital anomalies, thyroid surgery, history of neck radiation, history of autoimmune disease, or hypomagnesemia. The patent received, g of calcium gluconate, administered, followed by (0 g of calcium gluconate for ,4 hours intravenously. Furthermore, oral medication started.
The patent was diagnosed with Fahr’s syndrome due to primary hypoparathyroidism based on the CT and laboratory findings. The patent was discharged from the hospital on the day after reception without symptoms.
Discussion
Fahr’s disease primary familial brain calcifcaton is a genetically dominant, inherited and progressive neurological disorder, which is sporadic and has a genetic locus on chromosome (4q48r 32 Although Fahr’s disease is associated with some underlying medical conditions, the exact etiology remains unknown r Causes include; endocrinopathies hypoparathyroidism primer or seconder2, pseudohypoparathyroidism, pseudo pseudohypoparathyroidism, hyperparathyroidism, hypervitaminosis D, vasculitis erg. Systemic lupus erythematosus2, mitochondrial disorders ergr mitochondrial myopathy, infections erg. Brucellosis, abstain bar virus EBV2, human immunodeficiency virus HIV2, radiation, chemotherapy and carbon monoxide and lead poisoning, 62 Fahr disease is characterized by deposition of calcium in the walls of the capillaries and larger arteries and veins Although there are many specific hypotheses, the causes of abnormal calcification in the brain are related to parathyroid dysfunction or other causes of calcium metabolism overall [4,5]. However, it is not clear whether abnormal calcium deposition in the brain is caused by the local destruction of the blood brain barrier or by calcium metabolic disorder of neuron [5,6]. Calcification is extensive and has a relatively typical distribution: basal ganglia symmetric involvement of Globus pallidus, caudate, lentiform nucleus2, thalamus, cerebellum especially dentate nuclei2 and subcortical white matter [3]. These observations suggest that the pathogenesis of cognitive and motor changes in Fahr’s disease is based in a dysfunction of crotch basal connections and their interhemispheric relations [7,8]. We think that our patent had visual loss due to occipital accumulation. Magnet resonance imaging MRI2 is sensitive in detecting brain abnormalities; however, it is difficult to identify calcifications by routine Mir Therefore, brain CT scan is considered to be critical for detecting and localizing the extent of intracranial calcification [3,4]. Movement disorders are the most common indication of Fahr’s disease and Parkinsonism accounts for 57%r 32 Other clinical features include disordered speech, cerebellar signs, chorea, dystonia, orofacial dyskinesia, tremors, seizures, cognitive impairment, neuropsychiatric features, psychotic disorders and dementia [4,5]. We wanted to share our case because the symptoms of fluctuation in consciousness and vision loss related to Fahr’s disease are quite rarer Laboratory examinations in the suspected cases of Fahr’s disease should include tests for blood calcium and parathyroid hormone. This will help differentiate idiopathic Fahr’s disease unremarkable laboratory test results, from secondary cases especially due to hypoparathyroidism [6].
Conclusion
We report a case of Fahr’s syndrome with calcification of the basal ganglia due to hypoparathyroidism in a patent with fluctuation in consciousness and temporary vision loss as the main symptom. Although rare, Fahr’s syndrome should be suspected if there is symmetrical and abnormal calcification of both basal ganglia, visible via brain CT, of patents with confusion or loss of consciousness. Moreover, parathyroid function should be tested along with the calcium concentration in the blood; calcium concentration correction should be started early if hypocalcemia is present.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Yoo Jin Lee, Sihyung Park, Yang Wook Kim, Kang Min Park, Il Hwan Kim E, et al. (2018) A Case of Seizure Revealing Fahr’s Syndrome with Primary Hypoparathyroidism. Am J Case Rep 19: 1430-1433.
- Mohammad Taghi Niknejad, Maiu Lan Ho (2005) Fahr Syndrome, Radiopaedia.
- Gholam Ali Shahidi, Mahdi Safdarian (2017) Fahr disease: Idiopathic basal ganglia calcification. Iran J Neurol 16(1): 53-54.
- Akaninyene Asuquo Otu, Jude Chinedu Anikwe, Derek Cocker (2015) Fahr’s disease: A rare neurological presentaton in a tropical setng. Clin Case Rep 3(10): 806-808.
- Seyedmohammad P, Mohammad NS, Mohanad E, Mohamed B, Mohammed B (2018) Fahr’s Disease: A Diferental to Be Considered for Various Neuropsychiatric Presentatons. Cureus 10(3): e2304.
- Swami A, Kar G (2011) Intracranial Hemorrhage Revealing Pseudohypoparathyroidism as a Cause of Fahr Syndrom. Case Reports in Neurological Medicine 2011: 407567.
- Younes Mhenni S, Thobois S, Streichenberger N, Giraud P, Mousson de Camaret B, et al. (2002) Mitochondrial encephalomyopathy, lactic acidosis and stroke-like episodes (Melas) associated with a Fahr disease and cerebellar calcifications. Rev Med İnterne 23(12): 1027-1029.
- Carter L, Pasig Cr, Comaz A, Lopez J (2002) Neuropsychological and neurophysiological features of Fahr's disease. Rev Med Chil 130(12): 1383-1390.
-
Ozkara B, Ozcan M, Budak F. Fahr Syndrome with Fluctuation in Consciousness and Temporary Vision Loss. Arch Neurol & Neurosci. 5(5): 2019. ANN.MS.ID.000625.
-
Fahr Syndrome; Loss of consciousness; Vision loss; Hypoparathyroidism
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






