 Case Report
Case Report
Facial Nerve Paresis Functional and Aesthetic Improvement with Min- Invasive Methods
Marlen Sulamanidze1, Konstantin Sulamanidze2, George Sulamanidze3, Mariam Tsivtsivadze4* and Nino Vadachkoria4
1Department of Plastic and Reconstructive Surgery Total Charm Clinic, Irkutsk State Medical University, Russia
2Department of Plastic and Reconstructive Surgery Total Charm Clinic, Sechenov Medical University, Russia
3Department of Plastic and Reconstructive Surgery Total Charm Clinic, Pirogov Russian National Research Medical University, Russia
4Department of Plastic and Reconstructive Surgery Total Charm Clinic; Tbilisi’s State Medical University Hospital Department of Neurology, Tbilisi State Medical University, Georgia
Mariam Tsivtsivadze, Resident Plastic Surgeon, V.Orbeliani st 18, Tbilisi, Georgia.
Received Date: August 26, 2023; Published Date: September 07, 2023
Abstract
Facial paresis is a condition associated with loss of VII cranial nerve function. The facial nerve has an intricated course from the brain to the periphery. It consists of afferent somatic efferent, parasympathetic and branchiomotor fibres. It innervates up to 20 muscles of the face and head. The severity of facial paresis manifestation depends on the underlying cause. Facial reconstructive surgery approaches treating severe facial paresis can be divided in two group groups static and dynamic. The dynamic treatment approach address’s function while static treats facial deformities. All up-mentioned techniques represent a major surgical intervention lasting up to 12 hours with limited outcomes. The mini-invasive procedures are aiming to reduce functional and aesthetic problems associated with facial paralysis without aggressive interventions. The methods described in an article are used in 10 patients with total and partial facial paresis. Patients Follow-up for ten years demonstrated functional and facial symmetry improvement. Problems associated with a disability of eye closer, mastication and speech production has been reduced, and facial symmetry and self-esteem has been improved in all cases.
Keywords:Facial paralysis; Aptos threads; Eye closer; Monography; Facial asymmetry; Mini-invasive; Facelift
Introduction
Facial paresis is a condition associated with loss of facial muscle movement ability. This life-changing condition can be caused by several factors and can be permanent or temporary. The Human face is one of the most functionally and socially important parts of the body [1]. Only one glimpse of a person’s face identity, sex, age, health conditions, mood and their attitude are identified. Faces can leave a strong impression and can affect judgment about the owner’s personality. In a quarter of mint, decisions are made if the person is interesting or not. So facial paresis has a significant impact on individuals’ life not only on a functional level but in social dimension [2]. The facial paralytic state can have many etiological causes including neurologic, autoimmune, congenial, traumatic and iatrogenic. Facial paresis can be permanent caused by head trauma, stroke, head or a neck tumour, VII cranial nerve damage. The cause of temporary facial weakness can be an inflammation of the facial nerve, which causes temporary muscle weakness on one side of the face and affected part of the face droops like Bell’s palsy or polyneuropathy like in Guillain-Barré syndrome [3]. Complex pathogenetic mechanism is the reason for need of multidisciplinary treatment approaches. Investigation of Facial paresis causes, and its evaluation is the most important step for correct treatment planning. Only one method is rarely used. The Treatment planning is intricated due to lack of reliable indicators of spontaneous recovery. Contemporary treatment approaches can be divided in to pharmacologic, physical therapeutic and surgical [4,5,6]. The surgical interventions are classified as static and dynamic. Of course, all up mentioned techniques have their limitations [7,8]. This is the reason of demand on less invasive procedures for overall functional and aesthetic improvement. Aptos Thread Methods can be a substitution to static surgical interventions [9]. It is a mini-invasive procedure with long-lasting results which can improve functional and aesthetic problems associated with Facial paresis. Indications for Aptos Methods treatment are More than one year of facial paresis without improvement and Electromyoneurography data showing the absence of electrical and graded potential, correction need after dynamic or static surgeries [10].
Thanks to Aptos Threads unique designs improvement of facial symmetry and functionality can be achieved. Positioning Aptos threads in subcutaneous tissue gives the ability to elevate, fixate and create a volume of tissue in affected areas. There are several design threads for different indications making working on all parts of the face possible. All Aptos thread is available in two versions absorbable and non-absorbable. Absorbable one is made of polylactic aside and caprolactone (75:25). Non-absorbable is made of polypropylene. All polymers used in the creation of Atos threads are used in Surgery for more than fifty years. Aptos threads have fixators around which connective capsule forms. This guarantees thread anchoring in tissues, there fixation in a favourable position and prevention of thread migration as other sutures to. Besides all ap mentioned connective capsule formation provides long lasting result even in case of absorbable threads [11].
The Aptos Methods used in provided clinical cases:
Nano Spring Method Is 23G diameter device. The resorbable spirally thread USP 5.0 wrapped around blunt tip cannula. It is intended for armouring and lifting tissues around eyes and upper third of the face. Tissue fixation between spirals stabilises spring threads. Light lift Spring Method is spirally wrapped thread USP 2.0 around lancet pointed needle with the sharp tip. The thread is available in absorbable and nonabsorbable versions. This thread maintains its elasticity and shape after insertion thanks to its spiral shape which makes it the only choice for mimicry active areas. It lifts a middle third of the face and diminishes marionette lines effectively. Excellence Method represents multidirectional barbed thread USP 2.0 preloaded in 21G round tip cannula. The barbs unique design enhances tissue holding abilities. Which makes this thread plausible for all parts of the face and body.
Light Lift Thread Method is available in absorbable and non-absorbable version. The microscopic barbs are distributed along the thread bidirectionally. The peculiarity of the thread method is that it forms one sharp/blunt tip. After insertion into the required depth, the needle is separated into two parts, and each of them passes through hypodermic tissues in the necessary direction. The result is powerful, stable and long-lasting, and what is more important, it does not require the skin incision at all. Aptos Needle Method represents bidirectionally barbed thread connected to double sharp pointed Needles at the ends. Its design gives the ability to combine two needles forming one sharp end which provides the ability to insert threads from one entry point. Double-edged needles allow passing the threads along any necessary contour rotate needle under the dermis avoiding skin retractions. All manipulations are performed without skin cuts. The design of the device allows to stitch soft tissues, group them and shift to aesthetically favourable position.
The mini-invasive Static Aptos Method Procedures are performed under local anaesthesia after forming entry points with 18 G needle, the thread introducers are tunnelled sub-dermally in the pre-marked location that will provide the desired tissue fixation and result.
Case Report
The mini-invasive Static Aptos Method Procedures are performed under local anaesthesia. In the the case report patient history, treatment approaches, techniques and results are described and grouped by areas of intervention.
Orbital area

Case one is a 64-year-old male patient with total facial paresis. No improvement after two years of pharmacological and physical therapy treatments has been achieved. Electromyoneurographic investigation demonstrated lack of electrical and graded potentials. Both static and dynamic classical surgical interventions were offered besides mini-invasive Aptos Method treatment. The mini-invasive static procedure Aptos Needle Method procedure was performed for Brow and Nano Spring Method for lower eyelid ptosis treatment after two years of facial paresis onset. (See Figure 1)
Case two is a 35 YO old female patient with partial facial paresis. No improvement after one year of pharmacological and physical therapy treatments has been achieved. Electromyoneurographic investigation demonstrated lack of electrical and graded potentials. Both static and dynamic classical surgical interventions were offered besides mini-invasive Aptos Method treatment. The mini-invasive static Nano Spring Method procedure was used for lower eyelid ptosis correction after one year of facial paresis onset. (See Figure 2)

Case three is a 55 YO female patient with total facial paresis. No improvement after one year of pharmacological and physical therapy treatments has been achieved. Electromyoneurographic investigation demonstrated lack of electrical and graded potentials. Both static and dynamic classical surgical interventions were offered besides mini-invasive Aptos Method treatment. The mini-invasive static Nano Spring Method procedure was used for lower eyelid ptosis correction after one year of facial paresis onset. (See Figure 3)

Middle third of the face
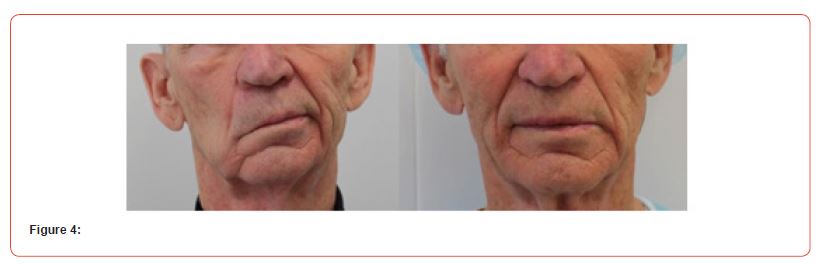
Case one is a 64 YO male patient with total facial paresis. No improvement after one year of pharmacological and physical therapy treatments has been achieved. Electromyoneurographic investigation demonstrated lack of electrical and graded potentials. Both static and dynamic classical surgical interventions were offered besides mini-invasive Aptos Method treatment. The mini-invasive static procedure Aptos Needle Method for volume creation in malar area, Thread Method was used for lower third of the face after two years of facial paresis onset. (See Figure 4)
Case four is a 32 YO female patient with total facial paresis. No improvement after one year of pharmacological and physical therapy treatments has been achieved. Electromyoneurographic investigation demonstrated lack of electrical and graded potentials. Both static and dynamic classical surgical interventions were offered besides mini-invasive Aptos Method treatment. The mini-invasive static Aptos Spring Method and Needle Method procedure was used for middle face ptosis correction and Aptos Thread method was used for lower third of the face after three year of facial paresis onset. (See Figure 5)

Case five is a 54 YO male patient with partial facial paresis. No improvement after one year of pharmacological and physical therapy treatments has been achieved. Electromyoneurographic investigation demonstrated lack of electrical and graded potentials. Both static and dynamic classical surgical interventions were offered besides mini-invasive Aptos Method treatment. The mini-invasive static procedure Aptos Needle Method procedure was performed for Brow and Needle Method for lower middle face and Thread Method for lower third of the face treatment after two years of facial paresis onset. (See Figure 6)

Results
The mini-invasive Aptos Thread Method procedures correct both functional and cosmetic problems effectively in patients with facial paresis. It eliminates problems associated with eye function, mastication, and speech production. The satisfactory facial symmetry is obtained without surgical interventions. In 80% of cases described thread lifting procedures were done the first time. The side effects have not been identified during the trial. The mild brushing and oedema which lasts up to 10 days were evaluated as normal. Only In 8% of patients received painkillers on the same day after the procedure. According to patient satisfaction survey analysis, up to 50% of patients were very, up to 20% fully, and up 15 % moderately satisfied with results during the first two years from the procedure. The result lasted more than two years in 80% of patients. The 90 % of patients evaluated their appearance as more attractive version of per-procedural appearance. The Patient per-procedural and postprocedural pictures were evaluated according to the Global Aesthetic Improvement Scale (GAIS) by dermatologists. The min index received is 3.1. These results demonstrate that Aptos Methods are mini-invasive procedures which treat cosmetic problems effectively with facial paresis. The satisfactory facial symmetry, tissue elevation and volume creation are obtained without surgical interventions. The Aptos mini-invasive Method procedures have minimal risk, short procedural and recovery time and provide long-lasting functionally and aesthetically favourable results. The Mini-invasive Aptos Thread Method Procedure result duration depends on Aptos thread type. In case of non-absorbable thread versions result lasts up to 5 years. The Same threads are used for cosmetic non-surgical facelifts. The following result lasts up to 2 years but due to muscular activity absence in patients with facial paresis results are preserved longer. In case of non-absorbable threads version results last more than ten years but due to ageing proses which have an impact on the non-effected side of the face thread procedure must be done on the non-effected side of the face after several years from procedure to preserve the symmetry of hemi sides of the face.
Discussion
The facial nerve has an intricated course from the brain to the periphery. It consists of afferent somatic efferent, parasympathetic and branchiomotor fibres. Facial nerve rote crosses frequently accessed surgical structures in head and neck surgery, otorhinolaryngology, and finally plastic surgery. It innervates up to 20 muscles of the face and head. Due to its complex structure, several conditions can affect its function. And veracious pathologies are causing facial paresis. The severity of its manifestation depends on the underlying cause. Facial reconstructive surgery approaches treating severe facial paresis can be divided in two groups static and dynamic one. Dynamic techniques are used in propose to restore the muscular activity of the face. The Dynamic methods can be divided into two types itself. One of which is neural and second musculofascial. The static treatment approach can address cosmetic and functional problems and corrects facial asymmetry and deformities. The approaches technique used by physician depends on the duration of paralyses, damage severances and patient age. The treatment of facial paresis with neural methods are indicated if the facial nerve is injured and its function is lost but muscular tissue is preserved. The muscular techniques are used in patients with anamnesis of facial paresis more than one year where neural techniques are not effective any more due to distal neural fibrosis and atrophy of neuromuscular junctions. The muscular approach is used in the middle third of the face mainly to aid mastication this technique is not able to restore movements associated with emotions. The static procedures improve facial appearance correcting asymmetry and facial deformities. It can address the functional problem as well as mastication, speech production and vision. Techniques used for this purpose are a surgical facelift, malar rise, tendon grafts, fat grafting. Static techniques can be used in patients who have undergone any dynamic treatment procedure to correct facial asymmetry and deformity or, patients who are more than 60 years old. Of course, all up mentioned techniques have its limitations, advantages, and disadvantages. Many patients are not willing to undergo through invasive procedures with long rehabilitation periods and with the unclear and not fully satisfactory outcome. Therefore, there is a rising demand for non- aggressive, mini-invasive treatment approach with plausible and long-lasting results. Aptos Thread Methods are mini-invasive procedures which do not need incisions. It is performed under local anaesthesia. Threads are inserted subcutaneously from entry point formed with 18 G needle. The Threads with fixators guaranties tissue fixation in a favourable position which provides functional and facial deformity correction. Aptos threads differ from stain and golden threads which have demonstrated poor corrective abilities. Aptos Thread method is a safe and effective procedure which lasts only 30 min. Its downtime lasts less than ten days and provides the favourable outcome. Aptos threads are indicated in patients with late facial paresis, for patients who are more than 60 years old or do not want to undergo complex, long-lasting surgeries or patients who have gone through dynamic or static surgeries and need additional corrections. Aptos thread Method represents a static non-invasive treatment approach intended for facial paresis functional and facial deformity correction. It improves problems associated with vision, mastication, and articulation. It enhances self-esteem in patients. Aptos mini-invasive Method procedures have minimal risk, short procedural and recovery time and provide long-lasting functionally and astatically favourable results.
Acknowledgement
None.
Conflict of Interest
The authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
References
- Danner CJ (2008) Facial Nerve Paralysis. Otolaryngologic Clinics of North America.
- O’Doherty J, Winston J, Critchley H, Perret D, Burt D, et al. (2003) Beauty in a smile: the role of medical orbitofrontal cortex in facial attractivess. Neuropsychologia 41: 147–155.
- Garcia RM, Hadlock TA, Klebuc MJ, Simpson RL, Zenn MR, et al. (2015) Contemporary Solutions for the Treatment of Facial Nerve Paralysis. Plastic and Reconstructive Surgery 135(6): 1026e–1046e.
- Lindsay RW, Robinson M, Hadlock TA (2010) Comprehensive Facial Rehabilitation Improves Function in People with Facial Paralysis: A 5-Year Experience at the Massachusetts Eye and Ear Infirmary. Physical Therapy.
- Brach JS, VanSwearingen JM, Lenert J, Johnson PC (1997) Facial neuromuscular retraining for oral synkinesis. Plastic and Reconstructive Surgery.
- Monini S, De Carlo A, Biagini M, Buffoni A, Volpini L, et al. (2011) Combined protocol for treatment of secondary effects from facial nerve palsy. Acta Oto-Laryngologica.
- Henstrom DK, Lindsay RW, Cheney ML, Hadlock TA (2011) Surgical treatment of the periocular complex and improvement of quality of life in patients with facial paralysis. Arch Facial Plast Surg 13(2): 125–128.
- Mehta RP, Hadlock TA (2008) Botulinum toxin and quality of life in patients with facial paralysis. Archives of Facial Plastic Surgery.
- Sulamanidze M, Sulamanidze G (2008) Facial lifting with aptos methods. Journal of Cutaneous and Aesthetic Surgery 1(1): 7.
- Grosheva M, Wittekindt C, Guntinas-Lichius O (2008) Prognostic value of electroneurography and electromyography in facial palsy. Laryngoscope.
- Sulamanidze M, Sulamanidze G (2009) APTOS Suture Lifting Methods: 10 Years of Experience. Clinics in Plastic Surgery 36(2): 281–306.
-
Marlen Sulamanidze, Konstantin Sulamanidze, George Sulamanidze, Mariam Tsivtsivadze* and Nino Vadachkoria. Facial Nerve Paresis Functional and Aesthetic Improvement with Min- Invasive Methods. Arch Neurol & Neurosci. 15(5): 2023. ANN.MS.ID.000874.
-
Brain Disorders. Nerves, Psychology, Spinal Cord, Neuropathies, Anorexia Nervosa, vertigo, Hyperactivity Disorder, Seizure, Mental Health, Nervous System, Cortex, Dementia, Multiple , sclerosis, Cognitive neuroscience, Schizophrenia, Concussion, Alzheimer’s, Dementia, Depression, Motor , neurone Disease, Parkinson’s, Stroke, Addiction, Neurodegenerative Diseases, Consciousness, Dyslexia, Brain Disorders, Traumatic Stress Disorder, Migraine, Epilepsy, Hypertension, Anxiety, Sleep Disorders Autism, Aneurysm.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






