 Research Article
Research Article
Effect of Attachment Profile on Affective Symptoms of Beginning Cognitive Disorders: the Oxytocin Receptor Polymorphisms
Olivier Tible, Departement of Psychiatry, Switzerland.
Received Date: October 23, 2018; Published Date: November 19, 2018
Abstract
Background: Behavioural and psychological symptoms (BPS) occur frequently in patients with dementia. These symptoms include affective (depression, anxiety) as well as psychotic features. In addition, many reviews have highlighted that a neurodegenerative disease can also be influenced by the subject’s personal attachment style (AS) and his social life quality. Recent studies have found that oxytocin receptor polymorphisms (OTrx) appears as a marker of emotional intensity and attachment that are paramount in social exchanges. Moreover, these studies have shown that OT likewise improves cognitive function, reducing amygdala responses to fear. Therefore, our approach is based on the following hypothesis: there are correlations between affective BPS, AS and OT receptor polymorphisms.
Methods: The present study assessed both OT blood levels and OT receptor polymorphisms (OTrx) in MCI patients. 9 MCI subjects and 8 controls are included. AS, BPS and depression were assessed using standardized scales. OTrx were determined using PCR.
Results: All MCI patients showed higher neuroticism, with an inhibited attachment style profile in one’s relationship to a parent. Insecure AS and OTrx were found in the two MCI patients presenting with the most severe affective BPS.
Conclusion: These results are in favour of our hypotheses (OTrx rs53576 and insecure AS are found in patients with severe BPS). Then, we found an inhibited attachment profile in patients with MCI, but it must be confirmed in the future.
Keywords: Oxytocin; Oxytocin receptor polymorphism; Mild cognitive impairment; Behavioral and psychological symptoms in dementia; Attachment; Personality; Neuroticism; Social anxiety
Abbreviations: BPS: Behavioural and Psychological Symptoms; OT: Oxytocin; OTrx: Oxytocin Receptor Polymorphisms; CDR: Clinical Dementia Rating; AS: Attachment Style (profile); HAD: Hospital Anxiety and Depression Scale; RAID: Rating Anxiety in Dementia; NPI: Neuro Psychiatric Inventory (assessment); MCI: Mild Cognitive Impairment; AMMI: Attachment Multiple Model Interview (AMMI)
Introduction
Behavioral and psychological symptoms (BPS) of dementia occur in most patients with dementia [1,2]. The clinical features of BPS include a wide variety of affective, psychotic and behavioural symptoms and signs. They cause great suffering in patients and caregivers. BPS, due to a complex and multifactorial etiopathogenesis, often occur in both mild cognitive impairment and dementia. Indeed, the causes and risk factors for BPS are multiple and include biological, psychological and environmental variables. Frequently, their combination explains the occurrence of BPS in an individual patient. Studying affective BPS, we have argued premorbid personality and attachment style towards relatives can help explain BPS during dementia [1-3]. Biological factors (e.g. cerebral lesions and altered neurotransmitters, comorbidities), may interact with psychological aspects (e.g. attachment, personality, social well-being). Some studies [1-5] have shown insecure attachment (through social behaviour)5 as well as personality traits (e.g. behavioral inhibition [4], neuroticism [5]) may lead to BPS in patients with cognitive impairment. Then, BPS are linked with changes in neurotransmission and neuromodulation.
Neurohormonal and neurotransmitters or their changes are involved in the occurrence of BPS [1,2]. Oxytocin (OT) is one of them [1,6-9]. These last several years, research on attachment suggest OT may be a determinant of attachment characteristics [6-9]. An increasing number of studies has also begun to reveal an important role of oxytocin (OT) in brain structures involved in social behavior. So, OT could play a key role in social modulating attachment and affiliative behavior [8]. Then, Oxytocin receptor with single nucleotid polymorphisms (SNP) rs53576 and rs2254298 (OTrx) are sometimes involved in affective disorders, such as depression as well as social anxiety or separation anxiety [10,11]. Correlations have been found between higher amygdala volume and rs53576 presence, underlying stress reactivity and neuroticism. Sippel et al. [12] indicate that the interactions between polymorphisms rs53576 and AS (insecure attachment) may contribute to vulnerability to post-traumatic stress disorder. In the same way, according to Schiele et al. [13], OT rs2254298 has a role in complicated grief, in separation anxiety, (especially if traumatic life event has occurred in children) with behavioural inhibition. Therefore, from what precedes, I have hypothesized that OTrx polymorphisms rs 53576 and rs2254298 as well as insecure AS should be involved in MCI with affective BPS (Figure 1).
Material and Methods
Subjects
This pilot study grafted upon a more comprehensive study conducted at Lausanne (Lausanne University Hospital) was approved by the ethics committee of Canton of Vaud. Nine patients with mild cognitive impairment (MCI) and eight healthy volunteers over 60 years participated in the study. For each subject and his relative, informed and written consent was obtained. We have explained to each subject and proxy the goals of this project. Patient recruitment was performed at the outpatient consultation of the Old-Age Psychiatry and the Lenard’s Memory Clinic of the Lausanne University Hospital. The recruitment of a cognitive healthy elderly control group was done by mouth of word and local advertisements in the above centers.
Inclusion criteria for MCI patients
• Patients > 60 years
• Diagnosis of MCI; CDR=0,5
• Possible AD, with or without subcortical vascular impairment
• Informed consent and patient has a proxy
• Patient accepts drawing blood for oxytocin analyses
Exclusion criteria for MCI patients
• Presence of a major psychiatric except for dysthymia or mild depression
• Presence of a neurological CNS disorder (epilepsy, stroke, tumor)
• Alcohol or drug abuse or dependency or presence of a severe physical illness
Procedure
Psychopathology and medical interview: We used the Mini International Neuropsychiatric Interview – French version 5.0.0 – to exclude patients or controls with major psychiatric disorders. Traumatic life events (since childhood into nowadays) were also checked.
Assessment of affective symptoms and BPS [1,2]
Standardized scales were used:
• The Hamilton anxiety and depression scale (selfevaluation).
• The NPI questionnaire.
• The RAID (Rating Anxiety in dementia) and Cornell scale were employed to assess respectively anxiety and depressive symptoms in dementia or MCI.
Assessment of attachment style: The Attachment Multiple Model Interview (AMMI) [14]: In our study, all attachment interviews were recorded. The AMMI assesses internal working models of specific relationships (e.g. mother, father, and romantic partner). AMMI dimensions for each subject in a specific relationship are the following:
• Secure attachment
• Inhibited attachment
The AMMI is a validated instrument. Its structure was developed based on the Adult Attachment Interview (AAI). For each dimension (inhibition and security), scores range from 0 to 8.
Personality assessment: big five inventory: The BFI is a wellknown and validated scale to measure 5 personality characteristics including extraversion, agreeableness, conscientiousness, neuroticism and openness to experience.
OT neuropeptide and OTrx (OT receptor polymorphism) by PCR: A blood test was realized at 9 am (for circadian rhythm). Two single nucleotid polymorphisms (SNP) rs 53576 then rs 2254298) were studied by Polymerase Chain Reaction with a thermal cycler (see https://www.thermofisher.com/ch/en/home.html online about these two polymorphisms).
Results
MCI patient’s vs controls
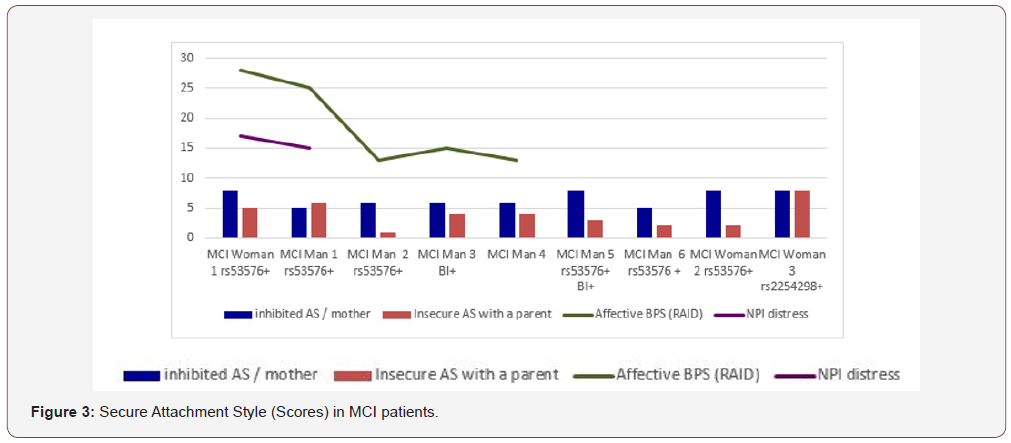
9 men and 8 women are included. Two patients and one control subject had to be excluded because of alcoholism, depression and stroke. First, there are no matches for age or gender between MCI and Controls, in each group (men and in women). However, each MCI group (men, women) is respectively comparable to controls. Table 1 shows the studied population characteristics (MCI vs Controls, in Men and Women) about age, educational level (from 1 school < 12 years; to 3, high school or university degrees), living alone or with relatives. Men have higher educational level than women do. Cardiovascular risk factors equally found in MCI and Controls. Finally, 3 MCI patients were alone without relatives, whereas all controls lived with their family. We found stressful life events in MCI (n=3) and controls (n=2), for the past five years (Table 1).
Table 1: MCI patients vs Controls.
*Socio-educational levels: 1= obligatory school 2= middle school 3= high school
*n=number of subjects with impaired cognitive test
Cognitive characteristics found in MCI patients
All MCI subjects have an altered episodic memory (observed during Grober Buschke test and also MoCA assessment), associated or not with others impaired cognitive functions (inhibition n=3; verbal fluency n=4; orientation n=3 in MCI). The MoCA test distinguishes MCI subjects from the others, even if scores are not always found pathological (sometimes scores are over 26 in MCI). Then, all subjects are autonomous and independent in everyday life (BADL=6/6; IADL=6/8 at least) (Table 1).
Attachment style
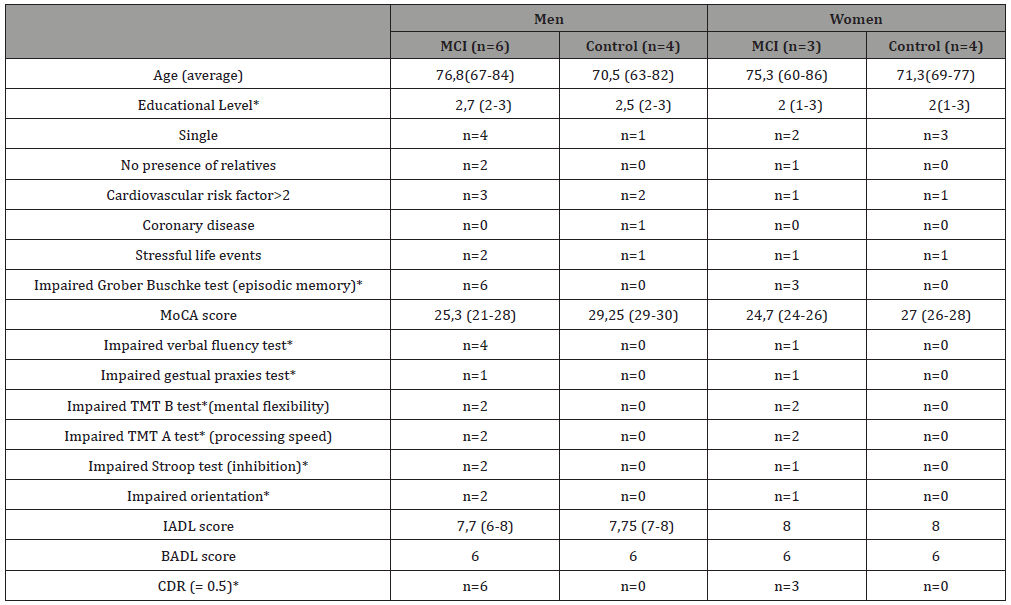
Inhibited attachment (with a parent) has been found in all MCI patients (men and women) (Figure 2). A statistically significant result (p < 0,05) was obtained, studying inhibited attachment with the mother, in MCI men, compared to control group (Mann-Whitney test studying median scores) (Figure 2).
Affective BPS
Affective BPS have been found in 5 MCI patients. For these 5 patients, we find depressive (Cornell, HAD) as well as anxious symptoms (HAD, RAID). However, only two patients present severe distress using the NPI; (Subject MCI 1 and Subject MCI woman) in the MCI group. Neither delusion nor hallucination have been found in MCI patients. We found insomnia, depressive symptoms, anxiety and autonomic activity (sub-scale in RAID) in the 5 subjects.
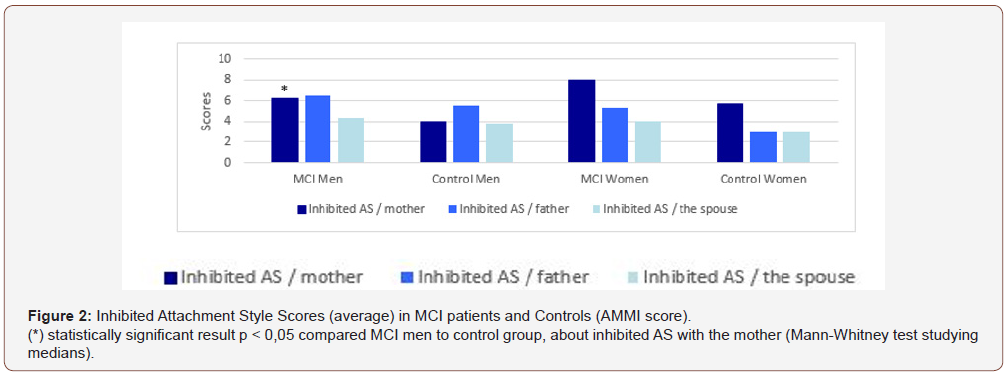
Figure 3 shows the 5 MCI subjects who have significant affective and anxious symptoms (green color). We found insecure attachment style with a parent in two subjects who have the most severe BPS (MCI Woman 1 and Man 1). These two patients have severe distress and suffering (on the NPI, in violet colour); they have the rs53576 OTrx (AG+ carrier). Otherwise, four MCI subjects have no BPS and are not insecurely attachment with a parent, nor do they have the rs53576 polymorphism. Two MCI men (number 3 and 5) presented behavioural inhibition BI+ (as a well-known risk factor to anxiety). Finally, MCI subjects who experienced the most severe affective BPS (n=2) have insecure attachment and rs53576 OTrx with higher neuroticism. Two others MCI subjects (with BPS) have insecure attachment (n=2) with behavioural inhibition BI (n=1). Only one MCI subject (MCI Man 2 with BPS) has not insecure attachment, but he presented rs 53576 with a recent life event (his wife died two years ago) (Figure 3).
The big five inventory
Personality assessment using the Big Five inventory (relative French version) showed higher neuroticism (statistically significant result) in the MCI group compared to controls (Figure 4).
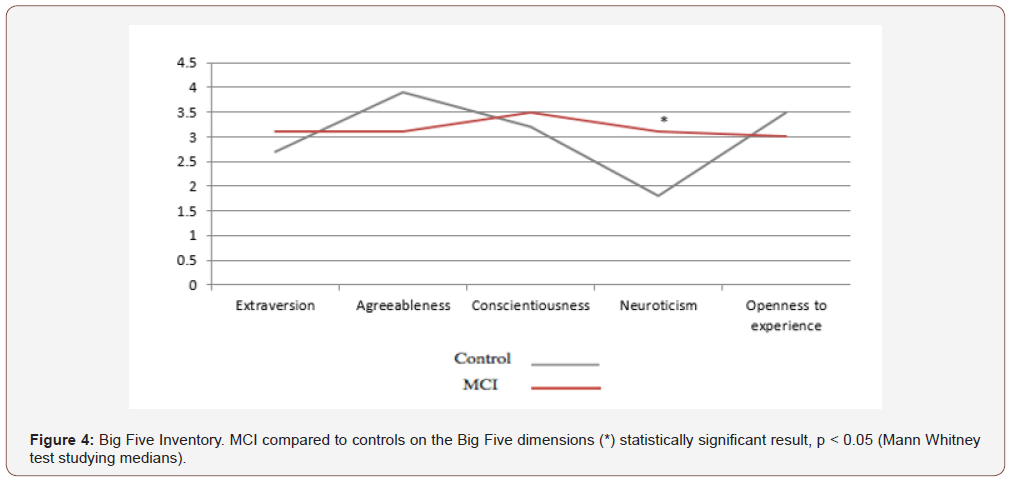
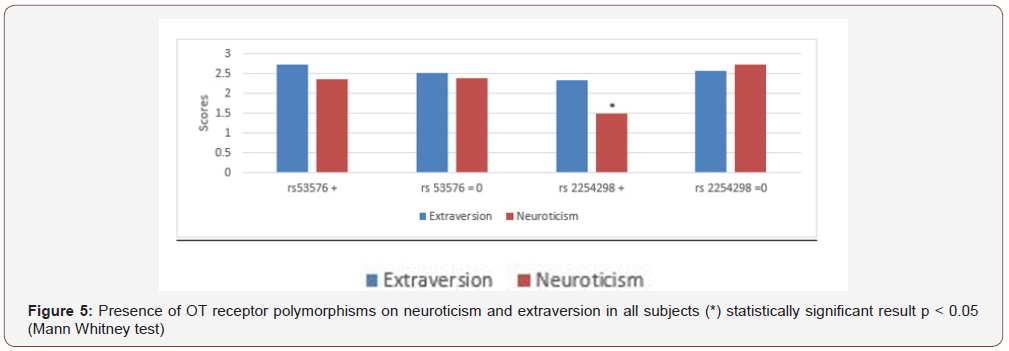
Figure 5 shows no correlation between the presence or absence of 53576 and extraversion or neuroticism levels. However, regarding rs 2254298 that is not present in MCI men, we found an opposite link between the neuroticism and the rs2254298 presence (significant difference) here (Figure 5).
Discussion
Summary of the clinical and neurobiological results
• Here, the episodic memory is altered for all MCI subjects.
• OTrx 53576 is often present in MCI, with or without affective symptoms (BPS).
• All MCI patients show an inhibited attachment style profile in one’s relationship to a parent.
• Higher Inhibited attachment (with a parent) is found with statistical significance (p < 0,05) in MCI men.
• Insecure Attachment and OTrx rs53576 were found in the 3 MCI patients having the most affective BPS.
• OTrx 2254298 is not involved in MCI or in affective BPS but linked with a low neuroticism.
• There is no link between OTrx and attachment style.
• Neuroticism is higher in MCI than in Controls (p< 0,05).
Firstly, the following hypothesis has been confirmed: there is a link between severe BPS and insecure attachment in subjects who have rs53576 (AG+ carrier). BPS occur frequently throughout the course of MCI and dementia. Here we can say there is an expected number of patients who have BPS (n=5 out of 9). Two of them have important NPI scores. Affective symptoms such as anxiety, depression, insomnia are found: these symptoms may worsen the course of dementia.15 We have found insecure attachment (n=4 out of 5 MCI with BPS), which is a known risk factor for later anxiety and depression in adulthood [4,15-17]. Insecure attachment is a likely risk factor to affective BPS in MCI as well [1-3,16,17]. So, the combination of risk factors (insecure attachment and OTrs 53576, or BI as well) may help explain the occurrence of affective BPS, in an individual patient [2,3].
rs53576 polymorphism was found in MCI, rather than in the general population [11-13,18]. Our results are in favour of our hypothesis that rs53576 OTrx may be a risk factor to affective disorder. The rs53576 genotype “may present a greater biological sensitivity as well as stress reactivity” according to Chang et al.18 This polymorphism would prevent the RNA polymerase from recognizing the RNA chain. Thus, it leads to anxiety through the high amygdala’s reactivity [6,18,20,21].
Regarding the rs2254298 carrier, this OTrx is not present in MCI men, but only one MCI woman. To our surprise, we found a significant link between this rs2254298 OTrx and a low neuroticism in controls compared to subjects without rs2254298. If this were confirmed in other studies, it would mean the stress life during infancy mediated by this receptor (found by some authors) could lead to an acquired stress reactivity [10,13].
Inhibited attachment style was found in all MCI patients, but not in controls. Regarding inhibited attachment in dementia, Magai et al. [17] found demented subjects with an avoidant (inhibited) attachment had higher premorbid levels of contempt and anger or inhibition [17]. Subjects presenting inhibited attachment had more difficulty talking to their relatives about their needs. Many avoidance situations with the relative/parent have been noted for many years. They don’t talk to their relatives about their own needs and wants, or their worries. Maybe they do not want to disturb their parents. They tend to keep their difficulties inside, without talking to relatives about their feelings and needs. Of course, the inhibited attachment is not specific to the MCI group. Finally, we have to analyze these results with caution, given the small and non-representative sample size. Inhibited attachment might be improving the cognitive impairment risk through a not well-being and inadequate emotional life.
Conclusion
These results are in favor of our hypotheses (OTrx rs53576 and insecure AS are found in patients with severe BPS). Then, we found an inhibited attachment profile in patients with MCI, but it must be confirmed in the future.
Limitations
We can cited as evidence the following limitations:
• A low number of MCI subjects n = 9.
• Patients are older than controls.
• Attachment interviews were recorded, but it is very difficult to confirm our results because of retrospective assessment without specific behavioural study, even if the AMMI is validated.
• Most subjects have lived in infancy during the World War II in Europe that might explain both inhibited and insecure attachment with their parent in that time.
• No OTrx methylation was studied, whereas it could be linked with self-reported attachment avoidance [22].
Despite several limitations, these results are in favour of our hypothesis. Separation and attachment style might be involved in MCI and dementia, with or without BPS [2,3]. Surely, these findings need confirmation in the future.
Acknowledgemnet
None.
Conflict of Interest
No conflict of interest.
References
- International Psychogeriatric Association (2010) The IPA complete guides to behavioral and psychological symptoms of dementia. Milwaukee. IPA.
- Tible O, Riese F, Savaskan E, Von Gunten A (2017) Best practice in the management of behavioral and psychological symptoms of dementia. Ther Adv Neurol Disord 10(8): 297-309.
- Tible O, Mendez M, von Gunten A (2018) Phenomenological contribution to understanding of vocally disruptive behaviour: a clinical case study in a patient with dementia. Int J Geriatr Psy In Press.
- Tible O (2008) Phobie sociale et inhibition comportementale chez l’enfant et l’adolescent. Thèse de Médecine. Université Bordeaux 2, HAL.
- Sutin AR, Stephan Y, Luchetti M, Terracciano M (2018) Self-reported personality traits are prospectively associated with behavioral and psychological symptoms of dementia. Int J Geriatr Psy 33(3): 489-494.
- Mottolese R (2013) Rôle central de l’ocytocine dans la neurophysiologie de la personnalité sociale : interaction avec la sérotonine et implication dans la pathologie de l’autisme. Thèse de Neurosciences. Université Claude Bernard Lyon I, HAL.
- Stoop R, Hegoburu C, van den Burg E (2015) New opportunities in vasopressin and oxytocin research: a perspective from the amygdala. Annu Rev Neurosci 38: 369-388.
- Gottschalk MG (2018) Oxytocin and anxiety disorders. Curr Top Behav Neurosci 35: 467-498.
- Di Simplicio M, Harmer CJ (2016) Oxytocin and emotion processing. J Psychopharmacol 30: 1156-1159.
- Onodera M, Ishitobi Y, Tanaka Y, Aizawa S, Masuda K, et al. (2015) Genetic association of the oxytocin receptor genes with panic, major depressive disorder, and social anxiety disorder. Psychiatry Genet 25(5): 212.
- Costa B, Pini S, Baldwin DS, Silove D, Manicavasagar V, et al. (2017) Oxytocin receptor and G-protein polymorphisms in patients with depression and separation anxiety. J Affect Disord 218: 365-373.
- Sippel LM, Han S, Watkins LE, Harpaz-Rotem I, Southwick SM, et al. (2017) Oxytocin receptor gene polymorphisms, attachment, and PTSD: results from the National Health and Resilience in veterans study. J Psychiatr Res 94: 139-147.
- Schiele M, Costa B, Abelli M, Martini C, Domschke K, et al. (2018) Oxytocin receptor gene variation, behavioral inhibition, and adult separation anxiety. World J Biol Psychiatry 19(6):471-479.
- Miljkovitch R, Moss E, Bernier A, Pascuzzo K, Sander E (2015) Refining the assessment of internal working models: the Attachment Multiple Model Interview. Attach Hum Dev 17(5): 492-521.
- John A, Patel U, Rusted J, Richards M, Gaysina D (2018) Affective problems and decline in cognitive state in older adults: a systematic review and meta-analysis. Psychol Med 24: 1-13.
- Karantzas GC, Romano D, Lee J (2018) Attachment and aged care: a systematic review of current research. Curr Opin Psychol 25: 37-46.
- Magai C, Cohen CI (1998) Attachment style and emotion regulation in dementia patients and their relation to caregiver burden. J Gerontol B Psychol Sci Soc Sci 53(3): 147-154.
- Chang WH, Lee IH, Chen K, Chi MH, Chiu NT, et al. (2014) Oxytocin receptor gene rs53576 polymorphism modulates oxytocin-dopamine interaction and neuroticism traits: a SPECT study. Psychoneuroendocrinology 47: 212-220.
- King LB, Walum H, Inoue K, Eyrich NW, Young L (2016) Variation in the Oxytocin Receptor Gene Predicts Brain Region-Specific Expression and Social Attachment. Biol Psychiatry 80(2): 160-169.
- Connelly JJ, Golding J, Gregory SP, Ring SM, Davis JM, et al. (2014) Personality, behavior and environmental features associated with OXTR genetic variants in British mothers. PLoS One 9(3): e90465.
- Haram M, Tesli M, Dieset I, Steen NE, Røssberg JI, et al. (2014) An attempt to identify single nucleotide polymorphisms contributing to possible relationships between personality traits and oxytocin-related genes. Neuropsychobiology 69: 25-30.
- Ebner NC, Lin T, Muradoglu M, Weir DH, Plasencia GM, et al. (2018) Associations between oxytocin receptor gene methylation, plasma oxytocin, and attachment across adulthood. Int J Psychophysiol In press.
-
Olivier Tible. Effect of Attachment Profile on Affective Symptoms of Beginning Cognitive Disorders: the Oxytocin Receptor Polymorphisms. Arch Neurol & Neurosci. 1(5): 2018. ANN.MS.ID.000523.
-
Oxytocin, oxytocin receptor polymorphism, Mild cognitive impairment, Behavioral and psychological symptoms in dementia, Attachment, Personality, Neuroticism, Social anxiety
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






