 Research Article
Research Article
Comparison of Fluocortolone and Fluocortolone + Acyclovir Treatment in Patients with Bell Palsy
Yalim SD1, Yilmaz I2 and Ozluoglu L3
1Department of Otorhinolaryngology, Adana City Training and Research Hospital, Turkey
2Department of Otorhinolaryngology, Baskent University, Adana Dr. Turgut Noyan Application and Research Center, Turkey
3Department of Otorhinolaryngology, Baskent University Medical Faculty, Turkey
Sıdıka Deniz Yalım, Department of Otorhinolaryngology, Adana City Training and Research Hospital, Turkey
Received Date: March 06, 2020; Published Date: March 16, 2020
Abstract
Objective: This study compares the effectiveness of fluocortolone and fluocortolone+acyclovir treatments in patients with Bell palsy.
Materials and Methods: Thirty-eight patients with Bell palsy who received fluocortolone treatment and twenty one patients with Bell palsy who received fluocortolone+acyclovir treatment were evaluated according to the full recovery times, stapes reflexes and electromyography measurements.
Results: There was no significant difference between the treatment groups in terms of facial function, recovery time, stapes reflex and electromyography measurements.
Conclusion: Both fluocortolone and fluocortolone+acyclovir treatments are effective in the treatment of Bell palsy.
Keywords: Bell palsy; Treatment; Stapes; Electromyography
Introduction
Bell palsy is idiopathic, sudden onset and the most common cause of facial paralysis. Herpes simplex virus is the causative pathogen [1]. In a study which was done in 1996, herpes simplex virus genomes were found in the patients’ facial nerve fluids and herpes simplex virus genome reactivation was observed in the geniculate ganglion in 79 % of the patients [2]. Also, in animal studies herpes simplex virus has been shown to form facial paralysis. Varicella zoster virus reactivation was also proposed in the etiology of Bell palsy. Acyclovir is used in the treatment of herpes simplex virus and varicella zoster virus infections [3]. Acyclovir interacts with herpes virus DNA polymerase and inhibits DNA replication [2]. Steroid treatment has been found to be effective in the treatment of Bell palsy [2]. According to the metanalysis of Ramsey corticosteroids increased the treatment seventeen percent and this was statistically significant. Regardless of the severity of the palsy, the treatment should be started to all patients as soon as possible [4]. Recently it has been proposed that combined steroid and acyclovir treatment has been found to be more effective than the steroid treatment alone [2]. Adaour et al. reported that acyclovir+ prednisone treatment is more beneficial than prednisone treatment alone in patients with Bell palsy [5]. Hato et al reported that valacyclovir+steroid treatment had a 96% recovery rate; only steroid treatment was 89% successful and the difference was statistically significant [6]. However, before giving a definitive advice about the effect of antiviral treatment, there is a need for information from multicentric, randomized and double-blind studies with large patient populations with at least twelve months of follow up. Therefore, we planned to investigate the effects of fluocortolone and fluocortolone +acyclovir treatment on early and late recovery times and full recovery time, stapes reflexes and electromyography measurements in the treatment of Bell palsy.
Introduction
Fifty nine patients with Bell palsy were investigated retrospectively. The study was approved by the local ethic committee and the informed consent was taken from all of the patients. The patients were divided into two groups according to the drugs they used. The first group (38 patients) received only oral fluocortolone, the second group (21 patients) received fluocortolone and acyclovir. The inclusion criteria of the study were as follows: 1) patients who were admitted within 72 hours after the onset of paralysis were included in the study. 2) antiviral treatment had been given to the patients who had a viral infection recently. 3) all of the patients received 250 mg intravenous methylprednisolone at the beginning of the treatment. 4) the patients with Ramsey Hunt syndrome were excluded from the study.
Steroid and antiviral treatment given patients received acyclovir 2000 mg/day (Asiviral tablet 400 mg; Terra,Turkey) for five days and 1 mg/kg/day fluocortolone (Ultralan 20 mg tablet, Bayer Schering Pharma AG, Germany) for three days and then lowering 10 mg every three days. The patients were evaluated in terms of presence of diabetes mellitus, day of treatment start, full recovery time, stapes reflex and electromyography measurements. Facial functions were classified according to the House-Brackman classification before and after the treatment. The effects of drugs on facial nerve functions were evaluated with the nerve excitability and the voluntary facial movements. The decrease in the electromyography thresholds greater than 3.5 mA on the affected side was taken as a sign of a decrease in the nerve excitability. Facial nerve function was graded as complete, partial or absent according to electromyography. All of the patients were followed until full treatment.
Data analysis
SPSS.17 package programmed was used for data analysis. The datas in the study were given as mean ± standard deviation. Levene test was used to test homogeneity of group variances. The independent samples t-test used to compare means of the groups. Pearson’s chi square test is used to test if there is a relationship between two categorial variables. Statistical significance level was taken as 0.05 in the analysis.
Results
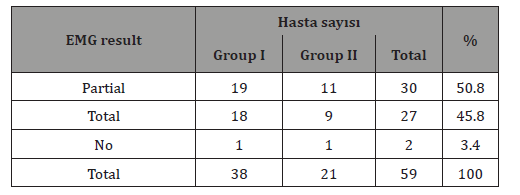
The ages of the patients was between 22 and 77. (mean 53.9±13.9) Twenty six patients were with diabetes mellitus. In the first group of patients (steroid treatment group) the average time to start treatment was 2.9 days and the average recovery time was 35.4 days. In the second group (steroid+antiviral treatment group) the average time to start treatment was 4.8 days and the average recovery time was 23.1 days respectively. Stapes reflex improved in 6.8 % of the patients. The facial functions of the patients were given in Table 1. The electromyography measurements of the patients were given in Table 2 (Table 1& 2).
Table 1:Facial functions of the patients before the treatment.
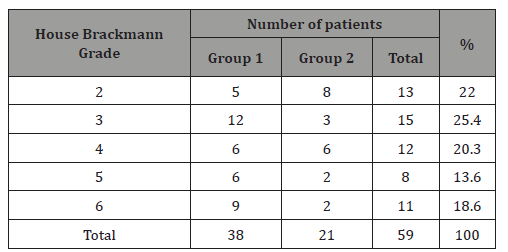
Table 2:Electromyography measurements of the patients.
There was not a statistically significant difference between the recovery times of groups. (Levene test, p=0.196; independent sample T-test, p=0.431). There was not a statistically significant difference between the day of treatment start of groups.(Levene test, p=0.01) The groups were not homogeneous so Mann-Whitney U test was used. (p=0.208). There was not a statistically significant difference between the House-Brackman facial paralysis grades of the patients before and after the treatment. (Pearson’s chi-square, p=0.08 and p=0.210 respectively). The House–Brackman grades of the patients were given in Table 3.
Table 3:House-Brackman Grades of patients after the treatment.
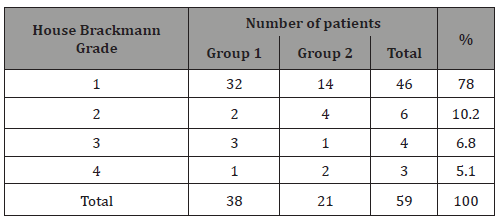
The initial House-Brackman classification of facial functions and the ratio of the patients were shown in Figure 1. The House-Brackman classifications of facial functions after the treatment were shown in Figure 2. There was not a statistically significant difference between the presence of the stapes reflex and electromyography measurements. The stapes reflexes and the ratio of patients were shown in Figure 3. The electromyography measurements were shown in Figure 4 (Figures 1-4).
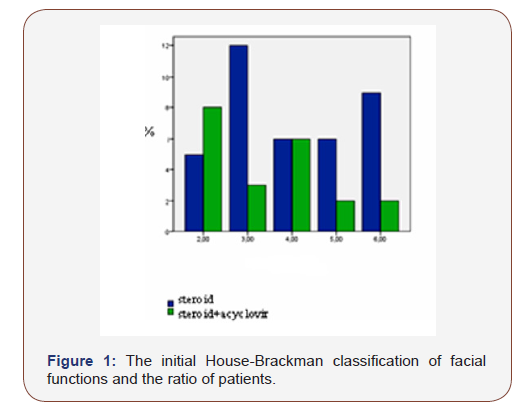
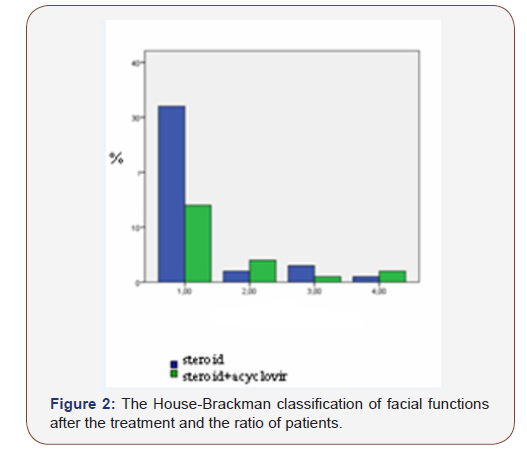
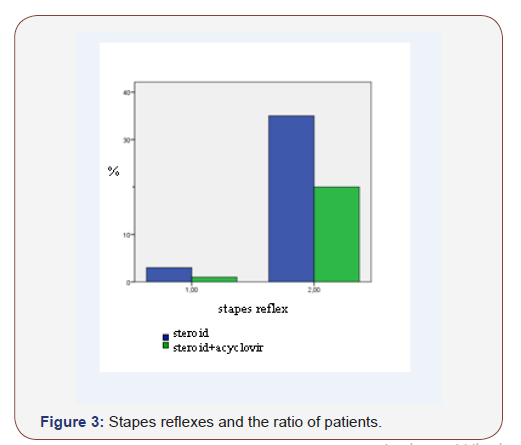
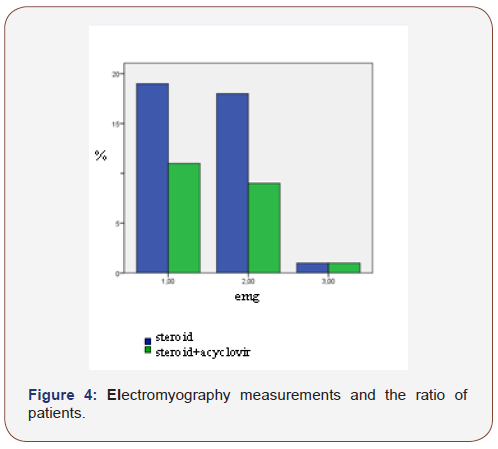
Table 4:The statistical analysis of group 1 (only fluocortolone) and group 2 (fluocortolone+acyclovir).
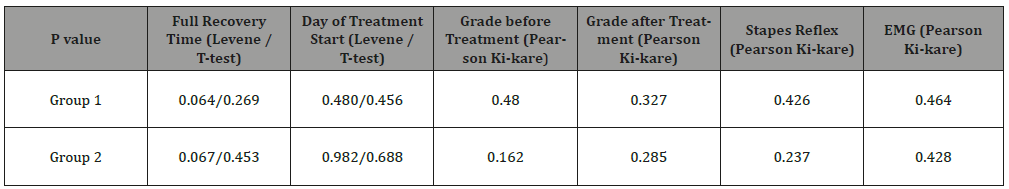
As a result of the analysis made between the patients with diabetes mellitus and the patients without diabetes mellitus there was not a statistically significant difference between the groups. The statistical analysis results of the groups were given in Table 4.
Discussion
Seventy percent of the patients with Bell palsy heal without a sequela. Corticosteroid treatment is effective in increasing the prognosis of Bell palsy but more than 10% of the patients cannot gain normal facial function and 5% of the patients remain with residual permanent facial paralysis, facial contracture, synkinesis and/or spasm [6]. Corticosteroid treatment provided a clinically and statistically significant improvement in the idiopathic facial prognosis [4]. Bell palsy resolves late in the diabetic patients and facial motion score is lower than the non-diabetic patients. More aggressive advanced treatments are needed in diabetic patients with Bell palsy, for example facial nerve decompression may be required [7].
Hato et al. reported that 100% improvement was achieved as an early treatment with both acyclovir and steroids in Bell palsy patients. According to their study in order for the combined acyclovir+ prednisolone treatment to show the highest effect in Bell palsy, the treatment should start within the first three days after the onset of paralysis besides early diagnosis [2]. According to Adaour et al. acyclovir+prednisone treatment is superior to prednisone only. Yeo et al. found higher recovery rates with steroid and acyclovir than steroid only, but the difference was not statistically significant. Therefore, acyclovir’s superiority to steroids in Bell palsy could not be proved [8]. As a result, steroid and antiviral treatment started in first three days may increase recovery rates in patients with Bell palsy when viral etiology was suspected [2].
However according to Sullivan et al. there was no evidence that only acyclovir was beneficial, and the combination of acyclovir and prednisolone had no additional benefits [9]. Similarly, Furuta [10], Allen [11] reported that acyclovir and prednisone treatment did not affect the improvement of facial paralysis. Also, Da Diego et al. reported that the acyclovir treatment, 800 mg three times daily was not as useful as 1 mg/kg steroid treatment for 10 days in the treatment of idiopathic facial paralysis [12]. As a result of metaanalysis comparing the corticosteroids with corticosteroid and antiviral agents, it was reported that addition of antiviral agents to the corticosteroids does not increase the rate of complete recovery of facial motor functions. The Cochrane study [11] and Goudakos’ metaanalysis reported the same results [13]. Our results are similar to these studies. Our results are related to acyclovir but the results from valacyclovir may differ.
Conclusion
As a conclusion, both fluocortolone and Fluocortolone + acyclovir treatments are effective in the treatment of Bell palsy but there is not a significant difference between the fluocortolone and fluocortolone+acyclovir treatments. Further studies are needed to confirm our results.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Coker NJ (1998) Bell Palsy: A Herpes Simplex Mononeuritis? Arch Otolaryngol Head Neck Surg 124(7): 823-824.
- Hato N, Matsumato S, Kisaki H, Takahashi H, Wakisaka H, et al. (2003) Efficacy of early treatment of Bell’s Palsy with oral acyclovir and prednisolone. Otology & Neurootology 24(6): 948-951.
- Kawaguchi K, Inamura H, Abe Y, Koshu H, Takashita E, et al. (2007) Reactivation of Herpes Simplex Virus Type-1 and Varicella-Zoster Virus and therapeutic effects of combination therapy with prednisolone and valacyclovir in patients with Bell’s palsy. Laryngoscope 117: 147-156.
- Ramsey MJ, Der Simonian R, Holtel MR, Burgess LP (2000) Corticosteroid treatment for idiopathic facial nerve paralysis: A meta-analysis. Laryngoscope 110: 335-341.
- Adour KK, Ruboyianes JM, Von Doersten PG, Byle FM, Trent CS, et al. (1996) Bell’s palsy treatment with acyclovir and prednisone compared with prednisone alone: a double-blind, randomized clinical trial. Ann Otol Rhinol Laryngol 105: 371-388.
- Hato N, Yamada H, Kohno H, Matsumato S, Honda N, et al. (2007) valacyclovir and prednisone treatment for Bell’s palsy: A multicenter, randomized, placebo-controlled study. Otology & Neurootology 28: 408-413.
- Haginomori S, Hasegawa A, Kitagawa Y, Nonaka R, Araki M, Takenaka H (2000) Prognosis of Bell’s palsy: Comparison of diabetic patients and nondiabetic patients. Otolaryngology Head and Neck Surgery 133: 209.
- Yeo SG, Lee YC, Park DC, Cha CI (2008) Acyclovir plus steroid vs steroid alone in the treatment of Bell's palsy. Am J Otolaryngol 29(3): 163-166.
- Sullivan F, Swan I, Donan PT, Morrison JM, Smith BH, et al. (2007) Early treatment with prednisolone or acyclovir in Bell’s palsy. N Engl J of Med 357(16): 1598-1607.
- Furuta Y, Ohtani F, Chida E, Mesuda Y, Fukuda S, et al. (2001) Herpes simplex virus type 1 reactivation and antiviral therapy in patients with acute peripheral facial palsy. Auris Nasus Larynx 28: suppl.13-7.
- Allen D, Dunn L (2004) Aciclovir or valaciclovir for Bell’s palsy (idiopathic facial paralysis). Cochrane Database Syst Rev 3: CD001869.
- Da Diego JI, Prim MP, De Sarria MJ, Madero R, Gavilan J (1998) Idiopathic facial paralysis: a randomized, prospective and controlled study using single-dose prednisone versus acyclovir three times daily. Laryngoscope 108: 573-575.
- Goudakos JK, Markou KD (2009) Corticosteroids vs corticosteroids plus antiviral agents in the treatment of Bell palsy: a systematic review and meta-analysis. Arch Otolaryngol Head Neck Surg 135(6): 558-564.
-
Yalim SD, Yilmaz I, Ozluoglu L. Comparison of Fluocortolone and Fluocortolone + Acyclovir Treatment in Patients with Bell Palsy. Arch Neurol & Neurosci. 7(4): 2020. ANN.MS.ID.000667.
-
Fluocortolone, Acyclovir Treatment, Bell Palsy, Otorhinolaryngology, Stapes; Electromyography, varicella zoster virus infections.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






