 Case Report
Case Report
Cerebral Venous Thromboembolism Complication of Isotretinoin Use: A Case Report
Okuyucu E Esra1, Guntel Murat1* and Demetgul Ozcan2
1Department of Neurology, Mustafa Kemal University Research Hospital, Turkey
2Neurology Clinic, Antakya Goverment Hospital, Turkey
Guntel Murat, Department of Neurology, Mustafa Kemal University Research Hospital, Turkey.
Received Date: January 27, 2020; Published Date: February 07, 2020
Abstract
Introduction: Isotretinoin (13-cis-retinoic acid (RA) is commonly used medication for the treatment of severe cystic acne that does not respond other therapies. Isotretinoin treatment has been associated with rare but serious complications such as cerebral thromboembolism.
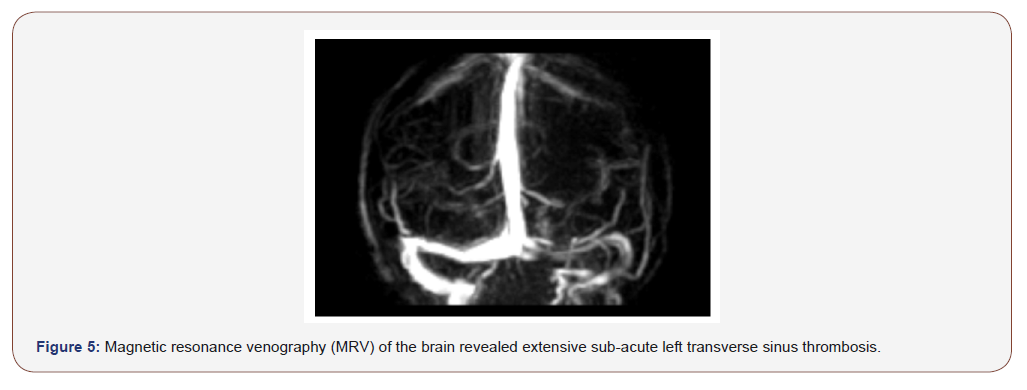
Case Report: A healthy 27-year-old woman, with no significant past medical history, presented with sudden onset of headache, vomiting, right hemiparesis and unconsciousness associated with convulsions. She had a history of taking isotretinoin for acne for the last 2 months. A magnetic resonance scan of her brain showed the presence of cerebral infarction of left thalamic area, magnetic resonance venography ultimately revealed left transverse sinus thrombosis. Treatment with anticoagulation recovered her from headache but not from hemiparesis.
Conclusion: Isotretinoin is one of the most used treatment modalities in many patients with acne. However, isotretinoin use can be associated with life-threating thrombotic side effects especially in young patients. Physicians must be more alert to be aware of this side effect.
Keywords: Isotretinoin; Complication; Cerebral venous thromboembolism
Introduction
Isotretinoin (13-cis-retinoic acid (RA) is commonly used medication for the treatment of severe cystic acne that does not respond other therapies. Isotretinoin treatment has been associated with neurological side effects such as; headache, insomnia, seizures, pseudotumor cerebri, muscle and joints pains, and rarely thrombotic-thromboembolic or hemorrhagic events [1,2]. Canadian Adverse Reaction Newsletter has mentioned 11 cases of thromboembolic events, strokes and myocardial infarction between 1983-2005 [3]. We report a case presented with right hemiparesis due to left transverse venous sinus occlusion associated with isotretinoin use for acne.
Case Report
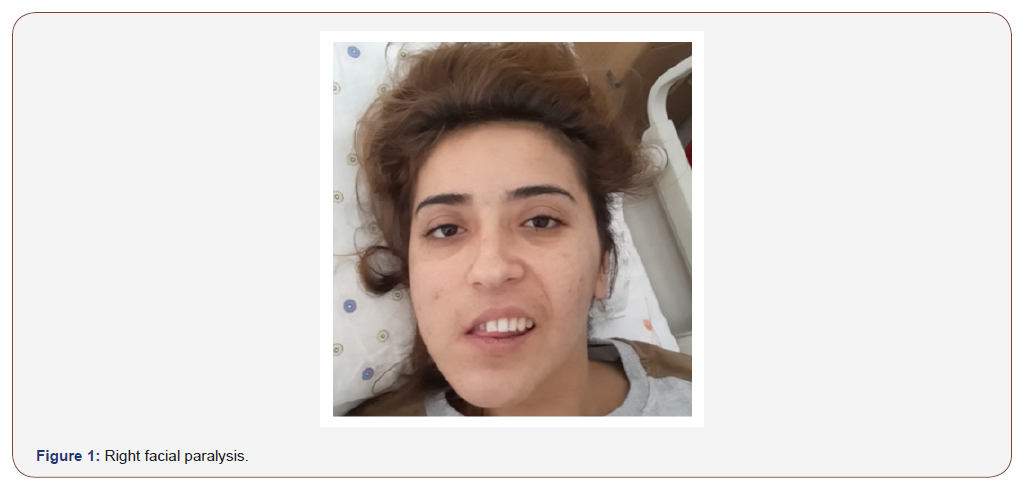
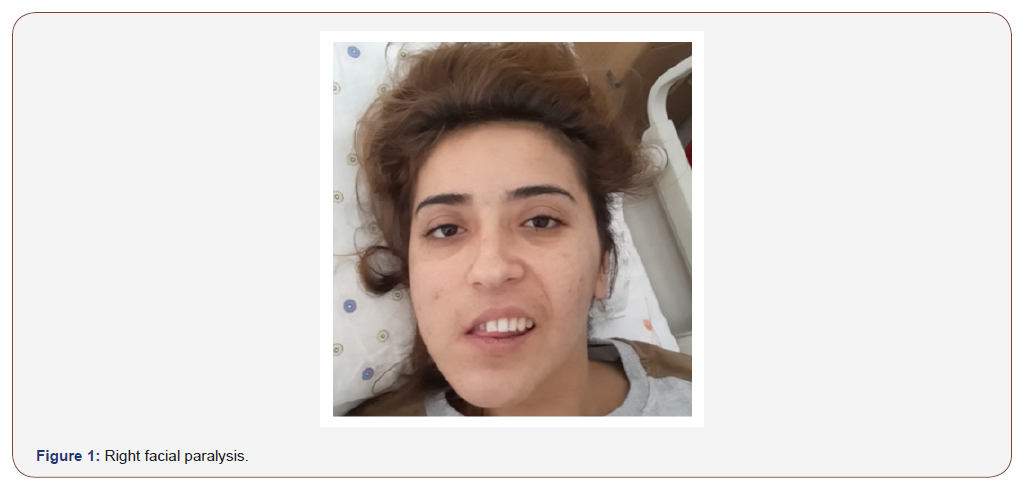
The patient is a 27-year-old woman presented with the sudden onset “worst headache of her life”, vomiting, weakness of the right side of her face, arm and leg, unconsciousness associated with convulsions. Her medical history was unremarkable except for acne. She had been treated with oral isotretinoin 20 mg three times daily for the previous 8 weeks. A review of system was negative. There was no family history of cancer, neurologic and hematologic disorders , cardiac problems. Her initial physical examination was negative. On admission, her initial vital signs were temperature 36.8 C, heart rate 88, respiratory rate 21, and blood pressure 120/72. Physical examination showed right upper and lower extremity weakness of a pyramidal pattern, right –sided facial motor and sensory impairment to touch and pin prick over the V1 and V2 distribution (Figure 1).
She had right sided hemihypoestesia and, severe broca aphasia. She was also quite restless and had intermittent disorientation due to convulsions. She consecutively developed severe focal seizure.
A detailed clinical investigation of all systems, including cardiovascular and hematologic assessment was unremarkable. Total blood count, erythrocyte sedimentation rate (ESR), C- reactive protein (CRP), creatinine kinase and electrolytes were normal.
Serum protein electrophoresis, autoimmune markers, work-up for vasculitis, hypercoagulable screening including anti-phospholipid antibodies, antithrombin III deficiency, protein C and S, activated protein C resistances, hyper homocysteinemia, factor V leiden and prothrombotic gene mutation were all unremarkable. DNA testing for genetic thombophilic predisposion were also negative.
Electroencephalography showed epileptiform discharges (Figure 2).
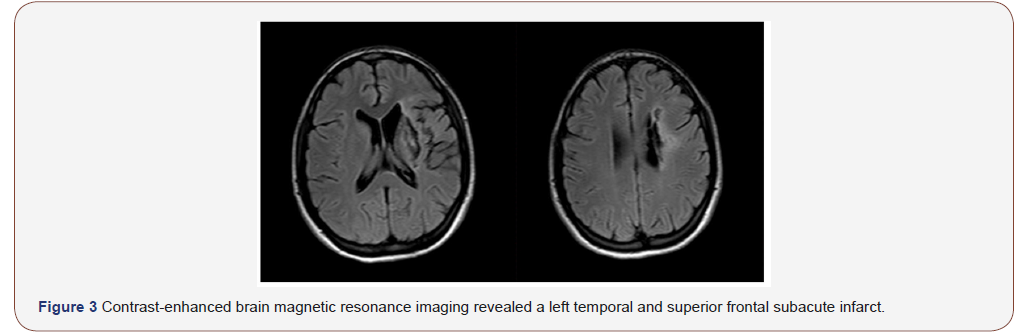
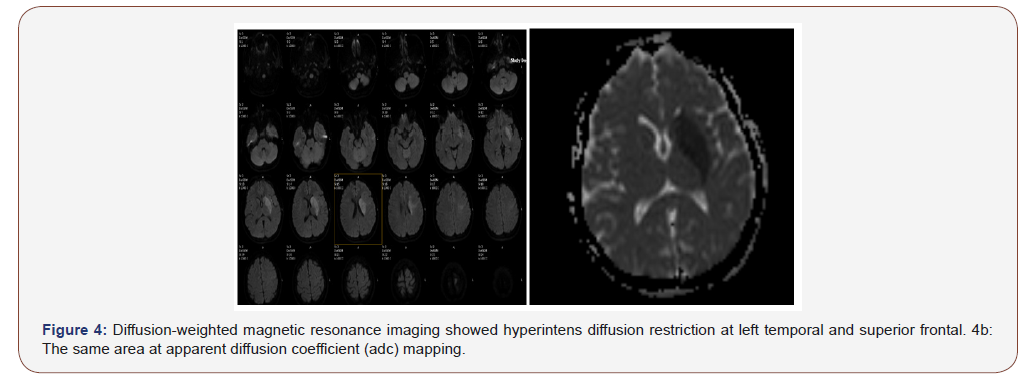
Contrast-enhanced brain magnetic resonance imaging revealed a left temporal and superior frontal subacute infarct (Figure 3), diffusion-weighted magnetic resonance imaging showed hyperintense diffusion restriction at the same area (Figure 4a and 4b). Magnetic resonance venography (MRV) of the brain revealed extensive sub-acute transverse sinus thrombosis (Figure 5). Doppler ultrasonography did not show any lesion on cervical arteries. Transthoracic and transesophageal cardiac ultrasound excluded thrombus or cardiac abnormalities.
At that time isotretinoin was discontinued and low molecular weight heparine, followed by oral warfarin was initiated to treat a suspected case of subacute cerebral venous infraction due to cerebral venous thrombosis (CVT) and antiepileptic drugs for acute symptomatic seizures (levetiracetam at 1,000 mg/day). One day later, and in spite of the treatment, the patient continued to have partial seizures with or without impairment of consciousness. Levetiracetam 2000 mg/day were necessary in order to control the seizures. She made remarkable clinical recovery 8 weeks later.
Discussion
Although the most common adverse effects of systemic retinoids are mucocutaneous (dry skin, cheilitis, scaling of the palms and soles, rash, dermatitis), gastrointestinal and ocular, the less common neurologic adverse effects must be recognized in some cases. Those most frequently forgathered are headache, insomnia, seizures, and confusion [1,2,4]. The absolute contraindication for isotretinoin usage is intracranial hypertension. Intracranial hypertension has been reported in patients under isotretinoin treatment [5]. The other rare neurologic adverse effects are memory disorder, neuralgia, facial paralysis, coma, and Guillain- Barré syndrome [1-6].
Ischemic strokes are not uncommon in young adults. Causes of cerebral ischemias are arterial (cervical dissection, arteriosclerosis, small-vessel occlusion on vasculopathy), cardiac (atrial fibrillation, endocarditis, cardiac malformations), hematological, genetic, and drugs (eg, cocaine, heroin, sympathomimetics, antihypertensives, heparin, oral contraceptives, sumatriptan, antineoplastic agents etc)[7].
In our patient, there wasn’t any risk factor that can have explained the young –onset stroke except isotretinoin usage. Moller et al, Laroche et al and Labiris et al reported thrombotic or hemoragic cerebrovascular adverse effects with systemic retinoids [5,8,9]. The Canadian Adverse Reaction Newsletter described 11 cases of myocardial infarction, stroke, and thromboembolic disorders associated with isotretinoin from 1983 to 2005 [3]. So several studies have reported cerebrovascular adverse effects with retinoids. However the mechanism is stil unknown, probably it seems to act on coagulation system.
In contrast to these reports of adverse effects, several studies have mentioned isotretinoin as a protector in thromboembolic disorders. They do this effect by reducing level of lipoprotein(a), which is related to premature coronary heart disease and stroke. And also, retinoids do not affect platelet aggregation, inhibited the vascular smooth muscle proliferation and vessel remodeling [10- 12].
This drug seems to act as a precipitator and a protector in thromboembolic events. Gornicki and Gutsze have reported that retinoid etretinate has role in increasing the erythrocyte membrane fluidity and later increase deformability of these cells [13,14].
Considering our patient, the relationship between isotretinoin intake and cerebrovascular event is “probable” according to the Naranjo adverse drug reaction probability scale [15].
Conclusion
Oral isotretinoin treatment is usually prescribed for young adults and cerebral ischemia is rare but a serious adverse reaction to isotretinoin. So, the patient must be aware of this potential side effect. Although in our patient, there was no potential vascular risk factor, to protect these patients from this adverse event, vascular risk factors must be evaluated prior to treatment.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- De Groot AC (2000) Dermatological drugs, topical agents and cosmetics. In: Dukes MNG, Aronson JK, (Eds.), Meyler’s side effects of drugs (14th), Amsterdam: Elsevier: 449-452.
- Marroni M, Bellomo G, Bucaneve G, Stagni G, Baldelli F (1993) Isotretinoin:possible cause of acute seizure and confusion. Ann Pharmacother 27: 793-794.
- Springuel P, Roy G Isotretinoin (2006) (Accutane): myocardial infarction,cerebrovascular and thromboembolic disorders. Can Adverse React Newslett 16: 3.
- DRUGDEX (2007) Greenwood Village, CO: Thomson Micromedex. Edition expires 12/.
- Laroche ML, Marcian Montoro F, Merle L, Vallat JM (2007) Cerebral ischemia probably related to Isotretinoin. Ann Pharmacother 41: 1073-1076.
- Pritchard J, Appleton R, Howard R, Hughes RAC (2004) Guillain-Barré syndrome seen in users of isotretinoin. BMJ 328: 1537.
- Modan B, Wagener DK (1992) Some epidemiological aspects of stroke: mortality/morbidity trends, age, sex, race, socio-economic status. Stroke 23: 1230-1236.
- Moeller KE, Touma SC (2003) Prolonged thrombocytopenia associated with isotretinoin. Ann Pharmacother 37: 1622-1624.
- Labiris G, Katsanos A, Karapetsa M, Ioanna M, Chatzoulis D (2009) Association between isotretinoin use and central retinal vein occlusion in an adolescent with minor predisposition for thrombotic incidents: a case report. J Med Case Reports 3: 58.
- Lee JY, Mak CP, Wang BJ, Chang WC (1992) Effects of retinoids on endothelial cell proliferation, prostacyclin production and platelet aggregation. J Dermatol Sci 03: 157-162.
- Georgala S, Schulpis KH, Potouridou I, Papdogeorgaki H (1997) Effects of isotretinoin therapy on lipoprotein (a) serum levels. Int J Dermatol 36: 863-864.
- DeRose JJ, Madigan J, Umana JP, Prystowsky JH, Nowygrod R, et al. (1999) Retinoic acid suppresses intimal hyperplasia and prevents vessel remodeling following arterial injury. Cardiovasc Surg 7: 633-639.
- Gornicki A, Gutsze A (2001) In vivo and in vitro influence of etretinate on erythrocyte membrane fluidity. Eur J Pharmacol 423: 127-134.
- Gornicki A (2006) Influence of the retinoid acitretin on erythrocyte microrheology in vitro. Int J Clin Pharmacol Ther 44: 648-654.
- Naranjo CA, Busto U, Sellers EM, Sandor P, Ruiz I, et al. (1981) A method for estimating the probability of adverse drug reactions. Clin Pharmacol Ther 30: 239-245.
-
Okuyucu E E, Guntel M, Demetgul O. Cerebral Venous Thromboembolism Complication of Isotretinoin Use: A Case Report. Arch Neurol & Neurosci. 7(1): 2020. ANN.MS.ID.000651.
-
Cerebral Venous, Thromboembolism Complication, Isotretinoin, Neurology, Brain, Isotretinoin, Complication, Cerebral venous thromboembolism.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






