 Review Article
Review Article
Bilateral Intracranial Subacute Subdural Haematoma
Uduma FU1*, Emejulu JKC2 and Okoye IJ3
1Department of Radiology, University of Uyo, Nigeria
2Department of Surgery, Nnamdi Azikiwe University Teaching Hospital, Nigeria
3Department of Radiation Medicine, University of Nigeria, Nigeria
Uduma FU, Department of Radiology, Faculty of Clinical Sciences, University of Uyo, Uyo, Nigeria.
Received Date: November 11, 2019; Published Date: November 19, 2019
Abstract
Bilateral intracranial subacute subdural haematoma is a subtype of intracranial haematoma with bleed in the subdural space that has lasted 4-21 days. It is relatively tasking to detect on CT but readily detected on different MRI sequences. Therefore, knowledge of its diagnostic imaging highlights is important to initiate management and prevent complications.
Keywords: Bilateral; Subacute; Subdural; Haematoma; MRI
Introduction
Intracranial subdural haematoma (SDH) is an extra-axial bleed into the potential space existing between the dura and arachnoid mater of the brain meninges. Subacute phase of this bleed is a temporal definition connoting that the bleed has lasted up to 4-21days [1]. Subdural haematoma is commonly due to trauma to the bridging veins between the calvarium and skull [2]. This is common in the elderly where age-related cerebral atrophy increases the space between the brain and skull to 6-11% of total intracranial space.2 On cross-sectional imaging subdural haematoma appears as crescent-shaped or concavo-convex extraaxial bleed on computed tomography (CT) and magnetic resonance imaging (MRI) images [3,4].
AIM- To depict imaging features of bilateral intracranial subacute subdural haematoma.
Discussion
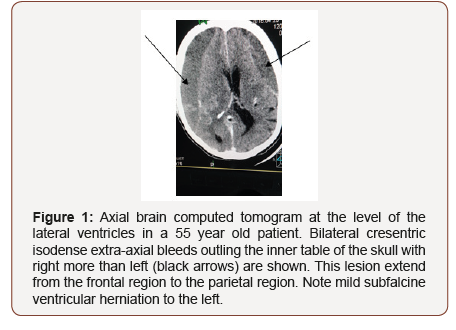
Subdural haematoma may not be accompanied by any visible injury to the scalp, skull or brain [3]. Hence radioimaging remains invaluable in its diagnosis. The temporal degredation of haemaglobin, a blood product after 4-21days of bleed will lead to the formation of methaemohlobinin. In early subacute phase (4- 7days), the methaemoglobin is intracellular whereas it becomes extracellular in late subacute phase (8-21days) [5]. In the latter, the bleed is isodense to grey mater on CT impairing easy detection (See Figure 1). Thus MRI becomes useful with up to 95% sensitvity in detecting variation in signal intensity from blood products in subacute SDH [3]. Since methaemoglobin is a paramagnetic material shortening T1 and T2 MRI relaxation times, in early subacute phase, the bleed will be hyperintense on T1W but hypointense on T2W and gradient echo (GRE) MRI images [5]. But this changes to T1W hyperintense, T2W Hyperintense with rim of low intensity and GRE hyperintense with rim of low intensity due to extracellular methaemoglobin in delayed subacute phase [5]. This bright signals of subacute SDH on MRI sequences including FLAIR is the beauty of MRI in the diagnosis of subacute SDH (Figures 1, 2 & 3).
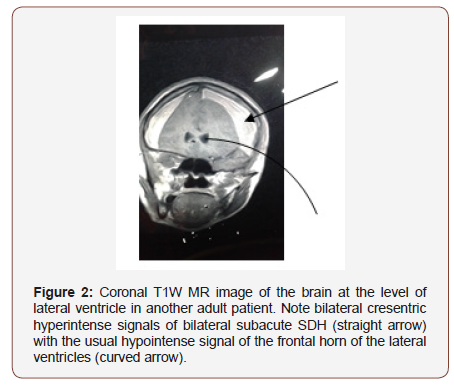
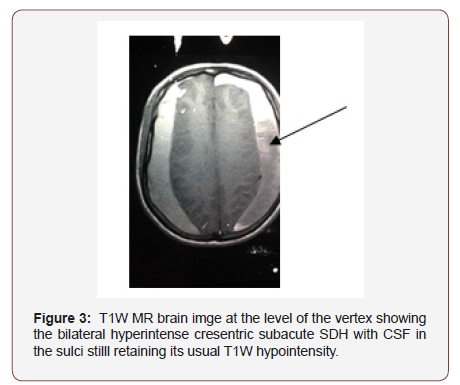
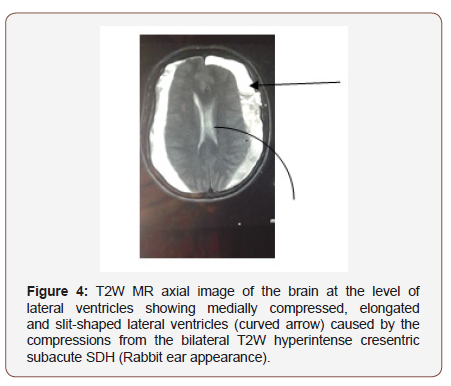
Worthy of note is the typical ‘rabbit ear appearance’ seen on MR images of bilateral subacute SDH.2 This is consequent upon the cerebral compressions by bilateral SDH which appears on MRI as bilateral cresentric hyperintersities outlining the inner table of the calvarium bilaterally (see Figure 2,3 & 4). The cerebral compressions will cause medial displacement of both lateral ventricles with frontal horns assuming a slit-shape with elongation called squeezed ventricles or rabbit’s ear appearance [2] (Figure 4).
Conclusion
Imaging is pivotal in bilateral intracranial subacute subdural haematoma as it may not be associated with any visible injury to the scalp or skull. Hence radio imaging remains the gold standard diagnostic method and knowledge of its typical imaging features is inevitable.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Jong-Ho Ha, Jong-Hyun Park, Je Hoon Jeong, Soo Bin Im, Sun-Chul Hwang (2018) Expanding subdural haematomas in the subacute stage and treatment via catheter drainage. Korean J Neurotrauma 14(2): 76-79.
- Adhiyaman V, Asghar M, Ganeshram KN, Bhomwick BK (2002) Chronic subdural haematoma in the elderly. Post-grad Med J 78 (916).
- Rao MG, Singh D, Khandelwal N, Sharma SK (2016) Dating of early subdural haemtoma: A correllative clinico-radiological study. J Clin Diagn Res 10(4): HC01-HC05.
- Uduma, FU, Motah M (2011) An accounting of pathology found on head computed tomography of road traffic accident (RTA) in Douala, Cameroon. Global J Health Sci 3(1):171-180
- Siddiqui FM, Bekker SV, Qureshi AI (2011) Neuroimaging of haemorrhage and vascular defects. Neurotherpeutics 8(1): 28-38.
-
Uduma FU, Emejulu JKC, Okoye IJ. Bilateral Intracranial Subacute Subdural Haematoma. Arch Neurol & Neurosci. 5(4): 2019. ANN. MS.ID.000616.
-
Bilateral, Subacute, Subdural, Haematoma, MRI, Concavo-convex, Magnetic resonance imaging, Visible injury, skull, scalp, brain, blood
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






