 Research Article
Research Article
Antopometric Evaluation of Employees at the Municipal Hospital of Cuiabá-HMC
Rodrigo PODEROSO1, Pedro, PODEROSO2 and Drackcyelle ALMEIDA³
¹Poderoso, Rodrigo, PhD in Sports Science in the Physical Education course at the University of Cuiabá- UNIC- Cuiabá-Mato Grosso, USA
²Poderoso, Pedro, Bachelor’s Degree in Physical Education at the University of Marília-UNIMAR, Marília-São Paulo, USA
³ALMEIDA, Drackcyelle, Nursing graduate at UNIVAG, USA
Rodrigo PODEROSO, Poderoso, Rodrigo, PhD in Sports Science in the Physical Education course at the University of Cuiabá- UNIC- Cuiabá- Mato Grosso, USA.
Received Date: July 06, 2023; Published Date: August 21, 2023
Abstract
Introduction:Currently, non-communicable chronic diseases have an important impact on the population’s morbidity and mortality, which is influenced by demographic and epidemiological changes, increased life expectancy and the practice of unhealthy habits. Obesity presents itself as a serious public health problem, being considered a risk factor and, at the same time, a chronic disease Objective: To evaluate the anthropometric profile of collaborators at Hospital Municipal de Cuiabá-HMC. Methodology. The sample had 580 employees, 360 female and 190 male, aged between 20 and 70 years, employees of the HMC. All assessments were carried out in the morning and volunteers were recommended to prepare for the assessment: fasting from food for 8 hours and fasting from alcohol for 48 hours, not practicing physical exercise in the 12 hours prior to the test. Anthropometric assessment included weight, height, waist and hip circumferences to verify data normality. The collected data were: age, practice time, weight data, abdominal circumference, hip circumference, height, ICQ, BMI, IAC. Results: The results found according to the references in the literature is that most employees of the Hospital Municipal de Cuiabá are overweight or obese. Conclusion: As a result of our study, and with the whole approach related to it, and in accordance with the literature, most of the collaborators are committed to the development of the metabolic syndrome or chronic degenerative diseases, the intervention of the practice of physical exercise and a diet would be essential for the number of overweight and obese people to change to low-risk metabolic syndrome patterns. waist and hip circumferences to verify data normality. The collected data were: age, practice time, weight data, abdominal circumference, hip circumference, height, ICQ, BMI, IAC. Results: The results found according to the references in the literature is that most employees of the Hospital Municipal de Cuiabá are overweight or obese. Conclusion: As a result of our study, and with the whole approach related to it, and in accordance with the literature, most of the collaborators are committed to the development of the metabolic syndrome or chronic degenerative diseases, the intervention of the practice of physical exercise and a diet would be essential for the number of overweight and obese people to change to low-risk metabolic syndrome patterns. waist and hip circumferences to verify data normality. The collected data were: age, practice time, weight data, abdominal circumference, hip circumference, height, ICQ, BMI, IAC. Results: The results found according to the references in the literature is that most employees of the Hospital Municipal de Cuiabá are overweight or obese. Conclusion: As a result of our study, and with the whole approach related to it, and in accordance with the literature, most of the collaborators are committed to the development of the metabolic syndrome or chronic degenerative diseases, the intervention of the practice of physical exercise and a diet would be essential for the number of overweight and obese people to change to low-risk metabolic syndrome patterns. abdominal circumference, hip circumference, height, ICQ, BMI, IAC. Results: The results found according to the references in the literature is that most employees of the Hospital Municipal de Cuiabá are overweight or obese. Conclusion: As a result of our study, and with the whole approach related to it, and in accordance with the literature, most of the collaborators are committed to the development of the metabolic syndrome or chronic degenerative diseases, the intervention of the practice of physical exercise and a diet would be essential for the number of overweight and obese people to change to lowrisk metabolic syndrome patterns. abdominal circumference, hip circumference, height, ICQ, BMI, IAC. Results: The results found according to the references in the literature is that most employees of the Hospital Municipal de Cuiabá are overweight or obese. Conclusion: As a result of our study, and with the whole approach related to it, and in accordance with the literature, most of the collaborators are committed to the development of the metabolic syndrome or chronic degenerative diseases, the intervention of the practice of physical exercise and a diet would be essential for the number of overweight and obese people to change to low-risk metabolic syndrome patterns. The results found according to the references in the literature is that most employees of the Hospital Municipal de Cuiabá are overweight or obese. Conclusion: As a result of our study, and with the whole approach related to it, and in accordance with the literature, most of the collaborators are committed to the development of the metabolic syndrome or chronic degenerative diseases, the intervention of the practice of physical exercise and a diet would be essential for the number of overweight and obese people to change to low-risk metabolic syndrome patterns. The results found according to the references in the literature is that most employees of the Hospital Municipal de Cuiabá are overweight or obese. Conclusion: As a result of our study, and with the whole approach related to it, and in accordance with the literature, most of the collaborators are committed to the development of the metabolic syndrome or chronic degenerative diseases, the intervention of the practice of physical exercise and a diet would be essential for the number of overweight and obese people to change to low-risk metabolic syndrome patterns.
Keywords:Nurses; Anthropometry; Obesity
Introduction
Chronic non-communicable diseases currently have an important impact on the morbidity and mortality of the population, which is influenced by demographic and epidemiological changes, increased life expectancy and the practice of unhealthy habits. Obesity presents itself as a serious public health problem, being considered a risk factor and, at the same time, a chronic disease (World Health Organization, 2017) [64]. The World Health Organization estimated that, in 2016, the rate of overweight people consumed more than 1.9 billion adults, of which 650 million would be obese, corresponding to 13% of the world’s adult population. Regarding children under 5 years of age, the estimate was 41 million (World Health Organization, 2017) [64]. Work is an essential activity for human beings; incorporates the man-nature relationship and the relationship between men and with themselves, which is established through social interaction. Seen as a growth factor, personal achievements or even survival. It can be considered an organizer of social life, although it contemplates paths for the process of cultural, social and economic dominance, and for the submission of the worker to capital, according to historical determinants (ALVESJÚNIOR, 2016) [3].
The transformations that have occurred in this environment in recent decades have caused changes in the work environment and, depending on the way it has been performed, may be related to wear and tear, worsening health conditions and even generate the illness itself (TEIXEIRA; MANTOVANI , 2009) [61]. In the era of globalization, the distribution of work activities, the increase in productivity in the labor market and the rejection of unemployment end up inducing the worker to submit to moral and sexual harassment, accumulation of functions, to achieve professional goals, excessive workload, among others. These factors can contribute to the imbalance of the emotional state, eating pattern, physical activity routine, sleep and, thus, reaching the incident of psychic and metabolic diseases (FERNANDES et al., 2017) [7]. As a result of these changes in the work environment, there was a concern with the Quality of Life at Work (QWL), which is defined by factors and characteristics present in the work environment. This theme aims to enable (ensure) the needs of workers when carrying out their work activities, with the purpose of acquiring more satisfied, productive people and better quality services. Specifically, in the case of nursing, which is a technical-scientific profession in which mental activities are used, but also physical activities; if the individual does not have both in perfect harmony, he begins to present health problems that compromise his work activity. Obesity is considered a serious public health problem worldwide, affecting men and women of all social classes, ages and cultures. It constitutes a risk factor for cardiovascular, musculoskeletal and neoplastic diseases. The prevalence of obesity is increasing among adults in both developed and developing countries. In Brazil, obesity reached between 2010 and 2019 at least 30% of the population. Projections based on national surveys carried out in recent decades estimate that obesity will reach, in 2025, 40% of the population in the United States, 30% in England and 20% in Brazil.
Anthropometry is the most used method in the diagnosis of obesity in population studies because it is the cheapest, non-invasive, universally applicable and well accepted by the population. Among the most used anthropometric indicators are the Body Mass Index (BMI) and Waist Circumference (WC).3 The practice of physical exercise, in addition to combating a sedentary lifestyle, contributes significantly to maintaining the physical fitness of the elderly, whether in terms of health or functional capabilities (GUARIDO, 2014). However, physical exercises may present some limitations for the elderly, due to the physiological changes imposed by the aging process. Water aerobics has some advantages for this population group, with the use of the physical properties of water allowing better performance for the elderly, Risk factors associated with obesity among workers include social stressors, psychosocial work factors, working hours, night work, and sedentary behavior (YARBOROUG et al., 2018). Work-related stress includes conflicts with colleagues and supervisors, lack of job control, and negative group climate at work (BLOUIN et al., 2017). The cited authors studied the influence of social stress among working women on the Body Mass Index (BMI) and the change in BMI over a year. Measures of social stress in the workplace - including job control and conflict with co-workers - were positively correlated with BMI. In addition, the authors observed that increased social stressors at work and reductions in work control increased BMI longitudinally (BLOUIN et al., 2017) [4].
Body mass index (BMI) and waist circumference (WC) have been widely used in the assessment of excess weight and abdominal obesity; are measures recommended by the World Health Organization (1) and by the National Heart, Lung, and Blood Institute of the National Institute of Health.
Methods
The study complied with the Regulatory Guidelines and Norms for Research Involving Human Beings by opinion (466/2022) and (510/2016) edited by the National Health Commission. Initially, a request was sent to the study site for data collection. That after the authorization of the place that was approved and authorized, the research project was sent to the Ethics Committee in Research with Human Beings of the UNIC University of Cuiabá for the ethical opinion, which was approved by the same institution, all signed the Term of Consent Free and Clarified (TCLE). All assessments were carried out in the morning and volunteers were recommended to prepare for the assessment: fasting from food for 8 hours and fasting from alcohol for 48 hours, not practicing physical exercise in the 12 hours prior to the test. Anthropometric assessment included weight, height, waist and hip circumferences. Weight was measured on a digital scale with a maximum capacity of 150kg and division of 100g, according to the standards recommended by Jelliffe 1966 [15], with barefoot individuals. Height was measured with a stadiometer fixed to a wall without a baseboard, with a length of two meters, divided into centimeters and subdivided into millimeters, with a plastic display and a square attached to one end, according to Jelliffe’s 1966 [15] standards. body weight (BMI) was calculated from weight and height measurements using the formula:
Circumferences were obtained with a flexible and inelastic tape, according to the techniques proposed by Callway et al. [6]. To measure the waist circumference, the tape was placed around the normal waist or in the smallest curvature located between the ribs and the iliac crest, keeping it tight, without compressing the tissues. The reading was taken between one expiration and one inspiration and the hip circumference was obtained by placing the tape around the hip region, in the area of greatest protuberance, without compressing the skin.
To verify the normality of the age data, the weight, height and BMI data were normal. Initially, descriptive statistics were performed to obtain mean, standard deviation, 95% confidence intervals, and absolute and relative frequency values. The Mann Whitney U test was performed to compare non-parametric variables between sexes for. Student’s t test was performed to compare parametric variables between genders. For all analyses, a 95% confidence level was adopted (p<0.05). Data were analyzed using SPSS IBM® version 20.0 statistical software.
Results
When it comes to epidemiological studies, the most frequently reported is the body mass index or BMI. It represents the most common measure, calculating the ratio between weight in kg by the square of height in meters. It is considered a world standard for analyzing the accumulation of body fat, as it is inexpensive and easy to analyze. Created in the 19th century by the mathematician Lambert Quételet, the Body Mass Index, known by the acronym BMI, is a simple calculation that allows you to measure whether or not someone has the ideal weight. It points out if the weight is adequate or if it is under or over weight. To calculate, simply divide weight by height squared. The final number represents how much muscle mass + fat mass + bone mass the person has. With the result, the next step is to interpret it. It is used by the WHO to classify the degree of obesity, when its value is above 30 kg/m². Classification is carried out as follows: grade I obesity, BMI is between 30 and 34.9 kg/m², grade II obesity, BMI is between 35 and 39.9 kg/m², grade III obesity, BMI is equal to or above 40kg/m², considered morbid obesity.
Although BMI does not clearly show one’s body composition, it has a good correlation with body mass and a poor correlation with a person’s size (Table 1, Graph 1, Graph 2).
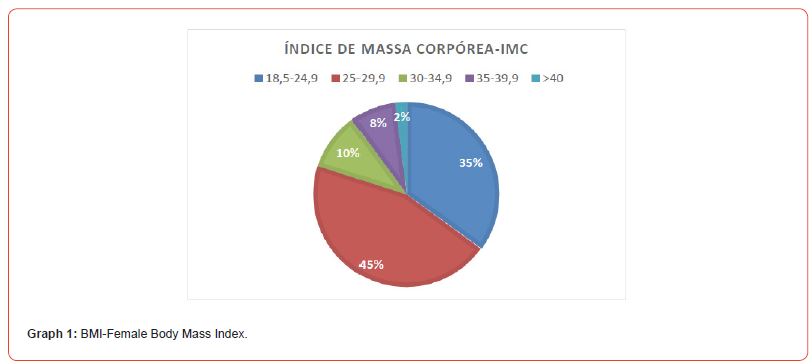
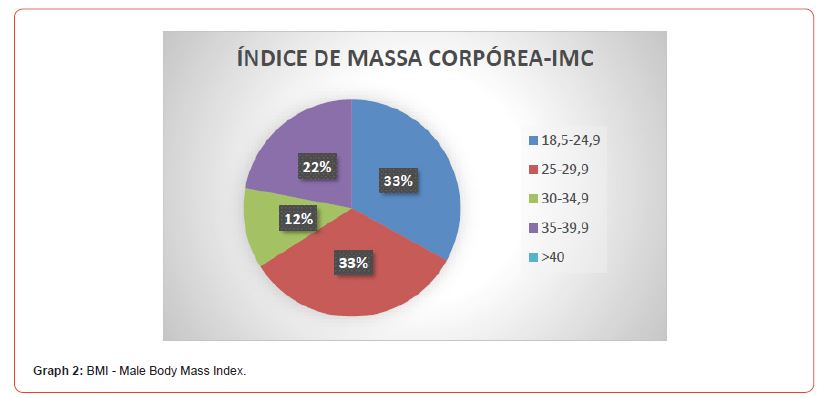
Table 1:Classification of nutritional status by BMI.
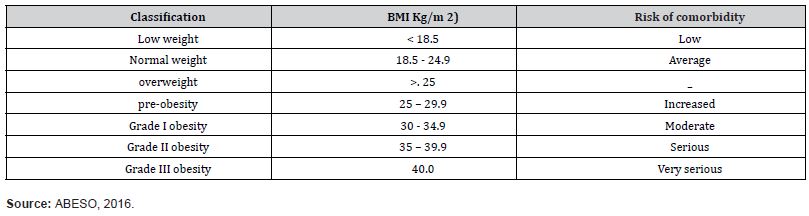
According to table 1, the HMC male employees are as follows: 33% healthy, 33% overweight, 12% obesity grade 1 and 22% obesity grade II (considered severe), no employee with obesity grade III (considered morbid) was found.
For females, according to Table 1, we find the following classification: 35% Healthy, 45% Overweight, 10% Obesity Grade I, 8% Obesity Grade II (considered severe) and 2% Obesity Grade III (considered morbid) When the recommended body mass index is exceeded, it is because the person may be overweight with a tendency to obesity or already have obesity. If the index is far below the normal range for men and women, it indicates that the person may be in a state of malnutrition, of significant loss of mass. And just like obesity, there are also degrees of thinness (Source: Ministry of Health 2019). According to the 2019 IBGE census, HMC employees, both male and female, are overweight, female employees have a higher prevalence of overweight compared to males. Considering the limitations presented by the BMI to estimate body adiposity and the absence of an index that would directly, simply, objectively and safely identify the percentage of total body fat, Bergman et al (2011) apud Segheto (2015), suggested a new form of assessment called IAC. This index is calculated based on measurements of height and hip circumference, with no need to measure body mass.
This form of evaluation, according to Jucá (2013) [16], the IAC considers the differences in the hips of men and women. In this sense, the use of hip circumference could represent an important conceptual advantage of the BAI. The formula described by Jucá (2013) [16] shows that the BAI formula is a little more complex, considering that it considers hip circumference and height, being represented by the following equation: [Hip/ (height x √height)] – 18 (Chart 2, Graph 3, Graph 4).
Table 2:WHO percentage fat classification.
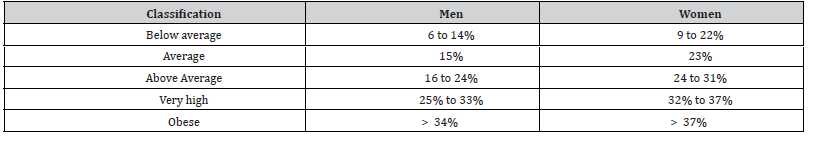
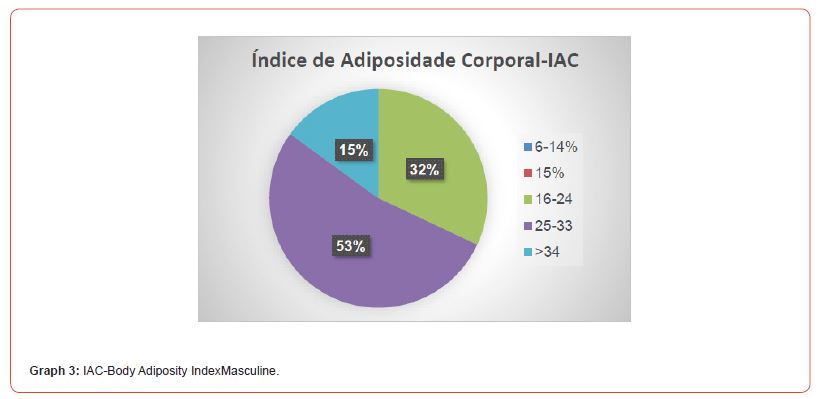
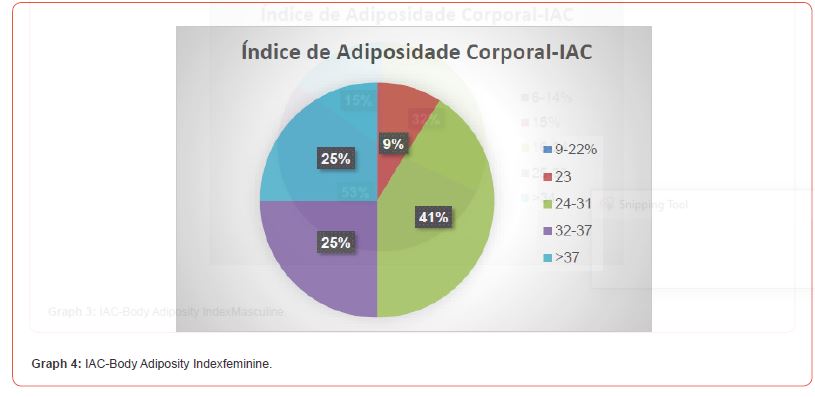
The BAI is calculated by the ratio [Hip / (height x height)] – 18. A healthy CAI for women ranges from 21 to 32; 33 to 38 indicates overweight and values above 38 are considered cases of obesity. Already healthy men should be between the range of 8 and 20; from 21 to 25 are considered overweight, and from 25 onwards, obese. According to chart 2 and comparing it to chart 3, we find that the percentage of fat among HMC male employees is 32% above average, 53% very high and 15% obese. Concerning the increase in the % of fat for the collaborators that there is a tendency of the development of the metabolic syndrome. Comparing chart 2 with chart 4 for females we find the following result, 9% average 41% above average 25% very tall and 25% obese. In the present study, we found that 50% of female employees are overweight and obese, a worrying factor for the development of metabolic syndrome. The relationship between gynecoid and android body fat distribution patterns and the prevalence of chronic diseases was first described by Vague in 1956. In 1984, Larsson et al. published a classic study showing that central body fat distribution better predicts the cardiovascular risk than excess weight per se. A simple and very revealing measurement is the abdominal circumference, which is taken with a measuring tape around the abdomen. According to the World Health Organization, ideal measurements for this region of the body are between 102 cm for men and 88 cm for women.
These authors used the waist/hip ratio to predict cardiovascular risk. Approximately 10 years after the publication by Larsson and collaborators, studies by Lean and collaborators were published, confirming what other studies had already pointed out, that simple waist circumference (WC) represented a risk for chronic disease. Lean et al. (1995) proposed cutoff points of 80 and 88 cm for women and 94 and 102 cm for men, characterizing risk (level 1) and increased risk (level 2). Based on these references, many studies were developed in different parts of the planet and evidence of an association between abdominal obesity and a higher prevalence of morbidities has been confirmed.
The measurement of WC, as it is recognized as an important and simple indicator of central obesity and risk for chronic diseases, is therefore considered in the diagnosis of the metabolic syndrome (INTERNATIONAL DIABETES FEDERATION, 2006; NATIONAL INSTITUTES OF HEALTH, 2002) (Table 3, Graph 5, Graph 6).
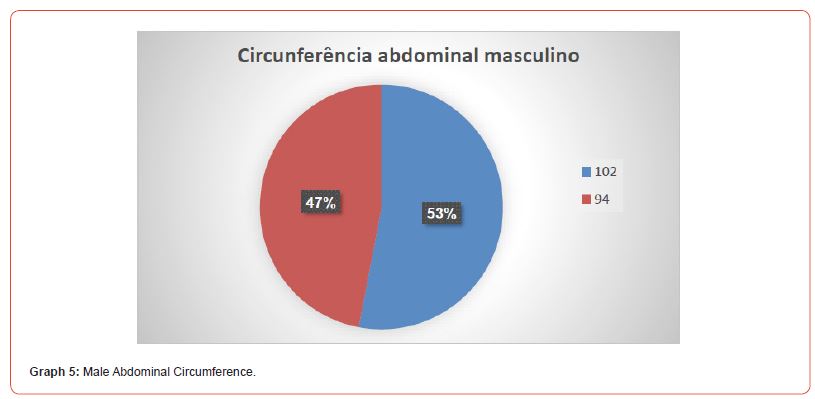

Table 3:Waist circumference.
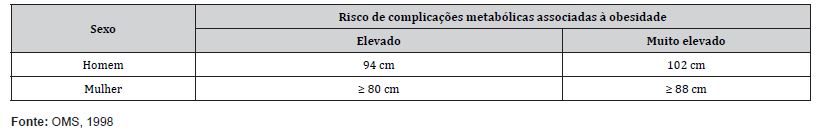
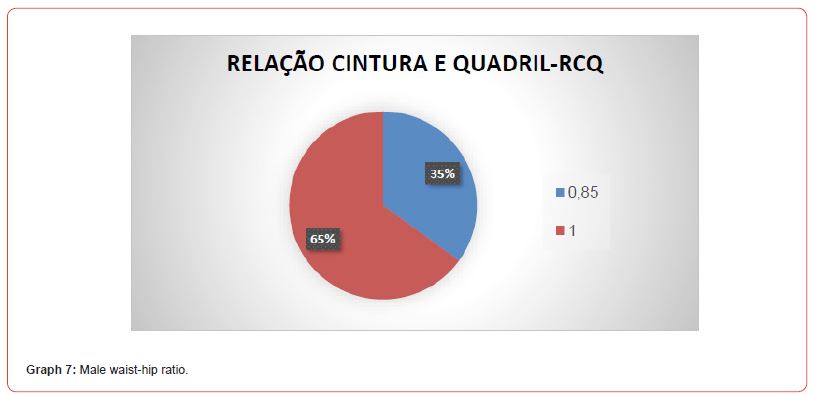
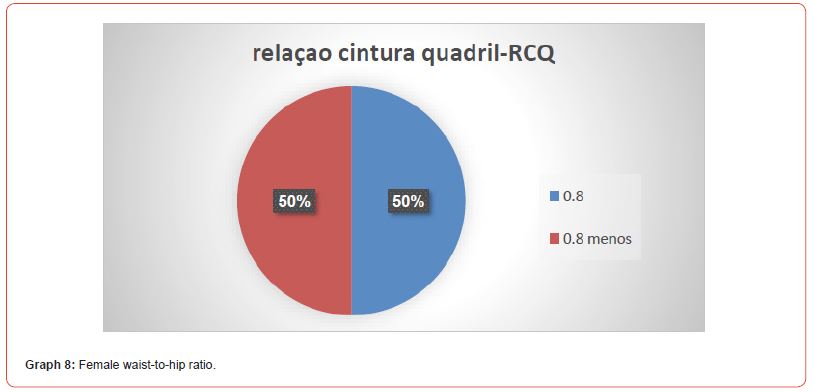
Following the reference of Chart 3 of the WHO - World Health Organization, we found male employees with 47% risk factor and 53% at risk breastfeeding, among female employees we found that 55% are in the risk group and 45% in the increased risk. In evaluating these protocols, we found that there is a high level of risk for both groups. Abdominal obesity affects more women than men. This data is worrying, since overweight is considered a public health problem with a growing tendency.). This variable deserves attention, since excess weight and waist circumference are included in the risk factors for CVD and for chronic degenerative diseases. The ICQ is used as an indicator or measure of a person’s health, and the risk of developing serious adverse health conditions. Research shows that apple-shaped people (with more weight around the waist) face more health risks than pear-shaped bodies, who carry more weight around the hips. ICQ is used as a measure ofobesity, which in turn is a possible indicator of other more serious health risks. WHOSTEPS says that abdominal obesity is defined as a waistto- hip ratio above 0.90 for men and 0.85 for women.
Waist-Hips Ratio (WHR)
Analyzing the data we found that both groups have an increased risk of developing the metabolic syndrome. This data is worrying, since overweight is considered a public health problem with a growing trend, especially in nurses. This variable deserves attention, since excess weight and WHR are included in the risk factors for CVD and for chronic degenerative diseases (Graph 7, Graph 8).
Discussion
The profile of overweight and obesity in nursing workers in intensive care and emergency units, which showed a high percentage of overweight and obesity in the investigated workers, where changes in lifestyle, mainly the inclusion of a healthy diet and the practice of physical exercises are important and necessary measures for the prevention and control of cardiovascular diseases, considering the growing increase in overweight and obesity in this society. According to Hoffmeister and Sousa (2016, p. 49), the classification into different groups as a result of the BMI calculation is important in view of the “high obesity rate”, which is present among Brazilian children and adolescents and has as causes main ones: “indulgence, in which they do not practice physical activities and the excessive use of electronic equipment, mainly caused by a sedentary lifestyle”. In this perspective, the BMI values can be used both to diagnose overweight and obesity and to diagnose chronic malnutrition, in the same way when obtaining the BMI values, which classify the percentage of fat in: risk (high body fat), excess of fat, moderately lean, lean, ultra lean, risk (low body fat). These studies, however, are contaminated by the influence of factors such as smoking, pre-existing diseases, recent weight loss, small number of participants and short observation period. In addition, BMI is an imprecise parameter, because it does not allow discriminating whether excess weight is linked to the exuberance of fatty tissue or muscle hypertrophy. It also does not allow for differentiating whether the adipose tissue is more concentrated in the abdomen – a higher risk situation – or in the buttocks and thighs, less threatening locations. These limitations reduce the accuracy of BMI in identifying those most likely to develop chronic diseases, such as cardiovascular,diabetesand cancer. The accumulation of fat in the abdominal region does not only involve aesthetic issues, it is directly related to the deposition of adipose tissue inside the abdominal cavity, a characteristic associated with increased overall mortality. The fat present in the buttocks or thighs has a less harmful metabolic effect. The largest study ever carried out on the influence of waist circumference on population mortality, in the various BMI ranges, has just been published by James Cerhan and collaborators of the Mayo Clinic, in the United States. There is evidence that moderate physical activity combined with less caloric diets causes metabolic changes capable of preventing the onset of diseases such as diabetes, high blood pressure, heart attacks and strokes, even when body weight loss is less than 3%. Eleven prospective studies conducted among 650,000 participants were evaluated. In each of the four BMI ranges – undernourished, healthy weight, overweight and obese – participants were divided into six subgroups, separated by 5 cm increments in waist circumference. The mortality rates of each subgroup were compared with those in which the participants had the smallest waist circumference (within that BMI range). During the observation period, 78,000 deaths occurred. In both men and women, waist circumference measurement was strongly linked to overall mortality. Compared to men with a circumference smaller than 90 cm, those measuring 110 cm or more had a 52% higher mortality. Women measuring 95 cm or more had 80% higher mortality than those with a circumference less than 70 cm. For every 5 cm increase in abdominal circumference, there was a 7% increase in male mortality and a 9% increase in female mortality, data that was repeated in all BMI ranges, with the exception of those below 20 kg/m2, in men. The association was most pronounced among 20- to 59-year-olds, but was documented even among 70- to 84-year-olds.
Compared with the subgroup with the smallest waist circumference, men with the largest circumference lost approximately 3 years of life; in women, the loss was 5 years. The most evident association was with respiratory and cardiovascular diseases; the relationship with cancer deaths was less clear, although significant. There is evidence that moderate physical activity combined with less caloric diets causes metabolic changes capable of preventing the onset of diseases such as diabetes, arterial hypertension, heart attacks. It is strokes, even when body weight loss is less than 3%. ICQ is used as a more efficient predictor of mortality in older people than waist circumference or BMI (PRICE 2006) [45] If obesity is redefined using ICQ instead of BMI, the proportion of people categorized as at risk of attack around the world increases by three times (YRSURF 2005) [63] The body fat rate is considered to be an even more accurate measure of relative weight. Of these three measurements, only the waist-hip ratio takes differences in body structure into account. So, it is possible for two women to have vastly different body mass indices but the same waist and hip indices, or to have the same body mass indices but vastly different waist and hip indices. Even in ancient civilizations, globally, female representations are more frequent in variations of 0.6 to 0.7 for ICQ, suggesting a preference for low ICQ (SINGH 2006). ICQ has been shown to be a better predictor of cardiovascular disease than waist circumference and body mass index (MORKEDAL 2011) [40]. However, other studies have shown that waist circumference, not ICQ, is a good indicator of risk factors cardiovascular, [8] Body fat distribution (Ketel 2007) [17] and hypertension in type 2 diabetes.
Conclusion
As a result of our study, and with the entire approach related to it, and in agreement with the literature, anthropometric assessment is of great importance to verify the level of obesity, and the association with metabolic syndrome. The intervention of the practice of physical exercise to improve the profile of HMC employees is extremely important to raise awareness of the practice of physical exercise, to improve the anthropometric profile as well as improve their quality of life.
Acknowledgement
None.
Conflict of Interest
No Conflict of interest.
References
- ABESO (2009) Brazilian Association for the Study of Obesity and Metabolic Syndrome.
- (2016) Brazilian obesity guidelines. 4.ed. São Paulo: ABESO.
- ALVES JUNIOR (2016) Self-perception of the physical education professional's role in combating obesity: a pilot study. Motricity 12: 30-41.
- BLOUIN C, HAMEL D, VANDAL N, Amadou Diogo Barry, Ernest Lo, et al. (2017) The economic consequences of obesity and overweight among adults in Québec. Can J Public Health 107(6): 507-e513.
- BRAZIL (2012) Ministry of Health. Secretary of Health Care. Department of Primary Care. National Food and Nutrition Policy. Ministry of Health. Secretary of Health Care. Department of Primary Care. Brasília: Ministry of Health.
- Callway CW (1988) Circumferences. In: Lohman TG, Roche AF, Martorell R. Anthropometric standardization reference manual. Champaign, IL Human Kinetics: 39-54.
- FERNANDES JC (2017) Workday and health of nurses in public hospitals according to gender. Rev Saude Publica.
- FINKELSTEIN S, HAMBRICK DC, CANNELLA AA (2009) Strategic leadership: theory and research on executives, top management teams, and boards. New York: Oxford University Press.
- FRAME E, KAPLAN G, PRONK N, O'DONNELL M (2014) Chapter 17: Addressing obesity at the workplace. Health Promotion in the Workplace 4th ed. Troy, MI: American Journal of Health Promotion Inc: 509-534.
- FRANCISCHI RP, PEREIRA LO, BOAT JUNIOR AH (2017) Exercise, eating behavior and obesity: review of effects on body composition and metabolic parameters. Paulista Magazine of Physical Education.
- GU JK (2014) Prevalence of obesity by occupation among US workers: the National Health Interview Survey 2004– 2011. J Occup Environ Med 56: 516-528.
- GUDZUNE KA (2013) Physicians build less rapport with obese patients. Obesity (Silver Spring) 21: 2146-2152.
- (2010) IBGE. Brazilian Institute of Geography and Statistics. Household Budget Survey 2008-2009: anthropometry and nutritional status of children, adolescents and adults in Brazil. Rio de Janeiro: IBGE.
- (2006) INTERNATIONAL DIABETES FEDERATION - IDF. The IDF consensus worldwide definition of the metabolic syndrome. IDF: 16.
- Jelliffe DB (1996) The assessment of the nutritional status of the community. Geneva: 13.
- JUCÁ EO (2018) Correlation analysis of body adiposity, body mass and body fat percentage in schoolchildren in the city of Porto Velho. Graduation Monograph in Physical Education. Porto Velho, RO: Federal University of Rondônia.
- Ketel IJ, Volman MN, Seidell JC, Stehouwer CD, Twisk JW, et al. (2007) «Superiority of skinfold measurements and waist over waist-to-hip ratio for determination of body fat distribution in a population-based cohort of Caucasian Dutch adults». eur. J. Endocrinol 156(6): 655-661.
- KIM MJ (2013) Association between shift work and obesity among female nurses: Korean Nurses' Survey. BMC Public Health 13: 1204.
- KOTTWITZ MU (2014) Social stress at work and change in women's body weight. Ind Health 52: 163-171.
- KOUWENHOVEN-PASMOOIJ T (2016) Cardiovascular disease, diabetes and early exit from paid employment in Europe; the impact of work-related factors. Int J Cardiol 215: 332-337.
- KRUSSIG K (2012) Obesity among nurses: prevalence and impact on work. Am J Nurse Practice 8: 14-21.
- KYLE RG, NEALL RA, ATHERTON IM (2016) Prevalence of overweight and obesity among nurses in Scotland: a cross-sectional study using the Scottish Health Survey. Int J Nurs Stud 53: 126-133.
- KYLE RG (2017) Obesity prevalence among healthcare professionals in England: a cross-sectional study using the Health Survey for England. BMJ Open 7: e018498.
- LAVOIE-TREMBLAY M (2014) Impact of a pedometer program on nurses working in a health-promoting hospital. Health Care Manag (Frederick) 33: 172-180.
- LETVAK S, RUHM C, GUPTA S (2013) Differences in health, productivity and quality of care in younger and older nurses. J Nurs Manag 21: 914-921.
- LOBELO F, QUEVEDO IG (2016) The evidence in support of physicians and health care providers as physical activity role models. Am J Lifestyle Med 10: 36-52.
- LORING B, ROBERTSON A (2014) Obesity and inequities: guidance for addressing inequities in overweight and obesity. Copenhagen.
- LOWDEN A (2010) Eating and shift work – effects on habits, metabolism and performance. Scand J Work Environ Health 36: 150-162.
- MACEDO TTS (2013) The meaning of obesity: the perception of obese patients. J Nurs UPE on line 7: 7064-7073.
- MACHADO LSF (2014) Health problems reported by nursing workers in a public hospital in Bahia. Rev Bras Enferm 67(5): 684-691.
- MAGNAGO TSBS (2010) Working conditions, sociodemographic characteristics and musculoskeletal disorders in nursing workers. Act paul. enferm., São Paulo 23(2): 187-193.
- MAURO MYC (2010) Nursing working conditions in the wards of a university hospital. Esc Anna Nery Rey Enferm 14(1): 13-18.
- MADRUGA SW (2012) Maintenance of eating patterns from childhood to adolescence. Journal of Public Health 46(2): 376-386.
- MARQUEZEA EC (2012) Weight gain in relation to night work among nurses. Work 41(1): 2043-2048.
- MCELLIGOTT D, CHAPTER KL, MORRIS DL, CLICK ER (2010) The effect of a holistic program on health-promoting behaviors in hospital registered nurses. J Holist Nurses 28: 175-183.
- MEDEIROS CRO, LOPES VR (2017) Stigmas of Obesity in the Context of Organizations: Abomination, Failure and Disability. Organizations in Context Magazine, São Bernardo do Campo 13(25): 21-49.
- MENDES KDS, SILVEIRA RCCP, GALVÃO CM (2008) Integrative review: research method for the incorporation of evidence in health and nursing. Text Context Enferm 17(4): 758-764.
- MONTEIRO CA, CONDE WL, POPKIN BM (2007) Income-specific trends in obesity in Brazil: 1975-2003. American Journal of Public Health 97(10): 1808-1812.
- MORAIS IC (2014) The role of nurses in the multidisciplinary team facing overweight/obesity in the workplace. Arch Health Invest 3(3): 15-23.
- Morkedal, Bjørn, Romundstad, Pal R, Vatten, et al. (2011) «Informativeness of indices of blood pressure, obesity and serum lipids in relation to ischaemic heart disease mortality: the HUNT-II studies». European Journal of Epidemiology 26(6): 457-461.
- (1998) NATIONAL INSTITUTES OF HEALTH - NIH. National Heart, Lung, and Blood Institute. Obesity Education Initiative Expert Panel. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults – The Evidence Report. obese. Res 6: 51S-209S.
- OLIVEIRA AFC, NOGUEIRA MS (2010) Obesity as a risk factor for hypertension among nursing professionals at a philanthropic institution. Rev. esc. sick USP [online] 44(2): 388-394.
- OLSON R (2016) Sleep, dietary, and exercise behavioral clusters among truck drivers with obesity. Implications for interventions. J Occup Environ Med 58: 314-321.
- PARK MH (2012) The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev 13: 985-1000.
- Price GM, Uauy R, Breeze E, Bulpitt CJ, Fletcher AE et al. (2006). «Weight, shape, and mortality risk in older persons: elevated waist-hip ratio, not high body mass index, is associated with a greater risk of death». Am. J.Clin. Nourish 84(2): 449-460.
- PROPER KI, KOPPES LL, MEIJER S, BEMELMANS WJ (2013) The Association between body mass index status and sick leave and the role of emotional exhaustion a mediation analysis among a representative sample of dutch employees. J Occup Environ Med 55: 1213-1218.
- QUIST H (2013) Psychosocial work environment factors and weight change: a prospective study among Danish health care workers. BMC Public Health 13: 43.
- REILLY JJ, KELLY J (2011) Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: systematic review. Int Jobs 35: 891-898.
- REIS FF, BRAGA ALS (2015) Night work and its impacts on the health of the nursing team: an integrative review. Rev Enferm UFPE online Recife 9(3): 7133-7145.
- ROOS E, Laaksonen M (2013) Working conditions and major weight gain—a prospective cohort study. Arch Environ Occupy Health 68: 166-172.
- RUSH T, LEARDMANN CA, CRUM-CIANFLONE NF (2016) Obesity and associated adverse health outcomes among US military members and veterans: Findings from the millennium cohort study. Obesity (Silver Spring) 24: 1582-1589.
- SANCHEZ BUSTILLOS A, VARGAS KGJRD, GOMERO-CUADRA R (2015) Work productivity among adults with varied body mass index: results from a Canadian population-based survey. J Epidemiol Glob Health 5: 191-199.
- SEGHETO W (2015) Body Adiposity Index: validation and associated factors in adults in a population-based study.
- Singh D (2002) «Female mate value at a glance: relationship of waist-to-hip ratio to health, fecundity and attractiveness»(PDF). Neuro Endocrinol. Lett. 23. Suppl 4: 81-91.
- SILVA FJ da (2011) Work ability and fatigue among nursing workers. São Paulog: 84.
- SILVA RM (2016) The effects of work on the health of nurses who work in clinical surgery departments at university hospitals. Rev. Latin-Am. Nursing 24: e2743.
- SILVEIRA CDS (2013) Profile of overweight and obesity in nursing workers in intensive and emergency care units. Science & Health Magazine, Porto Alegre 6(3): 157-162.
- SORENSEN G (2016) Integrating worksite health protection and health promotion: a conceptual model for intervention and research. Prev Med 91: 188-196.
- STEVENS S (2014) Get serious about obesity or bankrupt the NHS. NHS England.
- SWINBURN BA (2011) The global obesity pandemic: shaped by global drivers and local environments. Lancet 378: 804-814.
- TEIXEIRA RC, MANTOVANI MF (2009) Nurses with chronic illness: relationships with illness, prevention and the work process. Rev Esc Enferm USP 43(2): 415-421.
- YARBOROUGH CM (2018) Obesity in the workplace: Impact, outcomes and recommendations, Journal of Occupational and Environmental Medicine 60(1): 97-107.
- Yusuf S, Hawken S, Ounpuu S (2005) "Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: a case-control study". Lancet 366(9497): 1640-1649.
- (2017) World Health Organization. WHO. Obesity and overweight: Key facts [Internet].
-
Rodrigo PODEROSO, Pedro, PODEROSO and Drackcyelle ALMEIDA. Antopometric Evaluation of Employees at the Municipal Hospital of Cuiabá-HMC. Arch Neurol & Neurosci. 15(4): 2023. ANN.MS.ID.000869.
-
Brain Disorders. Nerves, Psychology, Spinal Cord, Neuropathies, Anorexia Nervosa, vertigo, Hyperactivity Disorder, Seizure, Mental Health, Nervous System, Cortex, Dementia, Multiple , sclerosis, Cognitive neuroscience, Schizophrenia, Concussion, Alzheimer’s, Dementia, Depression, Motor , neurone Disease, Parkinson’s, Stroke, Addiction, Neurodegenerative Diseases, Consciousness, Dyslexia, Brain Disorders, Traumatic Stress Disorder, Migraine, Epilepsy, Hypertension, Anxiety, Sleep Disorders Autism, Aneurysm.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






