 Review Article
Review Article
A Case Report of Posterior Reversible Encephalopathy Syndrome in a Libyan Child Stung by Scorpion and Review of the Literatures
Shirin Alougly1,2, Suliman Elbragathy1,2, Alia Alhsony1,2, Aisha Elarwah1,2, Abdulhamid ElShiky1,2, Emhemed Mousa1,2, Fatma F Almijbri1,3 and Awad Magbri4*
1Department of Pediatrics, Benghazi Children’s Hospital, Libya
2Department of Pediatrics, Benghazi University, Libya
3Department of Pediatrics, Libyan International Medical University, Libya
4Regency Surgery and vascular access center, Toledo, Oh
Awad Magbri, MD, Regency Surgery and vascular access center, Toledo, Oh, Libya.
Received Date: May 12, 2021; Published Date: June 07, 2021
Posterior reversible encephalopathy syndrome (PRESS) is a disorder of reversible subcortical vasogenic brain edema predominantly involving the parieto-occipital regions of the brain bilaterally. The pathophysiology of PRESS is not yet well known. PRESS occurs more in patients with acute neurological symptoms (seizures, encephalopathy, headache, and visual disturbances) or patients with renal failure and fluctuation of blood pressure. PRESS can also happen with the use of cytotoxic drugs, autoimmune disorders, sepsis, and pre-eclampsia or eclampsia. PRESS after scorpion sting is uncommon and rarely reported in literature. PRESS is generally reversible, both radiologically and clinically. Treatment of PRESS is symptomatic and involve determining and treating the underlying cause. We report on a case of 2.5-year old female developed PRESS with normal blood pressure after being stung by a scorpion. Her outcome was favorable despite the tumultuous hospital course. To the best of our knowledge, this is the third child reported with PRESS in the literature following a scorpion sting.
Keywords:Posterior reversible encephalopathy syndrome (PRESS); Seizures, Scorpion sting; Brain MRI; Cerebral autoregulation; Blood brain barrier; Edema
Introduction
Posterior reversible encephalopathy syndrome (PRESS) first described by Hinchey et al, in 1996 [1]. It is a clinicopathological condition presenting with transient neurological symptoms including headache, seizures, altered sensorium, and loss of vision. It has characteristic magnetic resonance imaging (MRI) findings which are potentially reversible [2]. Brain imaging usually reveals vasogenic edema predominantly involving the parieto-occipital regions bilaterally. The pathophysiology of PRESS is thought to be due to endothelial injury related to abrupt blood pressure fluctuations and/or direct effects of cytokines on the endothelium, which leads to breakdown of the blood– brain barrier and subsequent brain edema. PRESS is generally reversible, both radiographically and clinically, and usually has a favorable prognosis [3]. The underlying causes of PRESS include sudden rise in blood pressure, treatment with immunosuppression, or chemotherapeutic agents for lymphoma and leukemia, severe hypercalcemia, thrombocytopenic syndromes, Henoch–Schoenlein purpura, vasculitis, and renal failure [1,2,4]. A sudden rise in blood pressure in patients with renal failure appear to be well known cause of PRESS [2]. The prevalence of PRESS in children is not well established; however, there have been some reports of PRESS in children following chemotherapy and tumor lysis syndrome. Rapid fluctuation of blood pressure is common factor seen in PRESS [5]. The reports of PRESS especially after scorpion bites are uncommon in literature. The first case was reported by Luiz Carlos Porcello Marrone et al, in Brazil in 2012 [6] and the second case was reported by Houssam Rebahi et al, in Morocco [7]. This is the third case of PRESS after scorpion sting in a 2.5-year old Libyan girl.
Case History
A 2.5-year old female Libyan child who is known to be completely healthy before the incident. she was referred to our pediatric intensive care unit (PICU) in Benghazi children hospital (BCH), from a local hospital in southern part of Libya on July 25th, 2018. Her history began one week before admission to our PICU. She was reported to be stung by scorpion in her neck when she was asleep at home. Few minutes later, she started to feel unwell with pain and vomiting. She was taken to the local hospital where she received hydrocortisone and anti-scorpion venom antiserum following the diagnosis of scorpion bite. She was kept in the observation room for 12- hours. In the interim she developed generalized seizure and high-grade fever. Treated with an antipyretic, and a second dose of anti-scorpion venom. Her physical examination and vital signs including blood pressure were stable. However, because her Neurological examination revealed a marked visual impairment, aphasia, hypotonic and deterioration of her Glasco coma scale (GCS) to 10/15. Hence, no significant improvement in her condition was noticed, the decision was made to transfer her to our hospital for further management and care. In the PICU of BCH, her neurological examination showed mild deterioration in her GCS. Confirmation of blindness, aphasia, hypotonia and hyporeflexia were also noted on examination. Her vital signs (blood pressure, pulse, and temperature) were normal during her stay in the BCH-PICU.
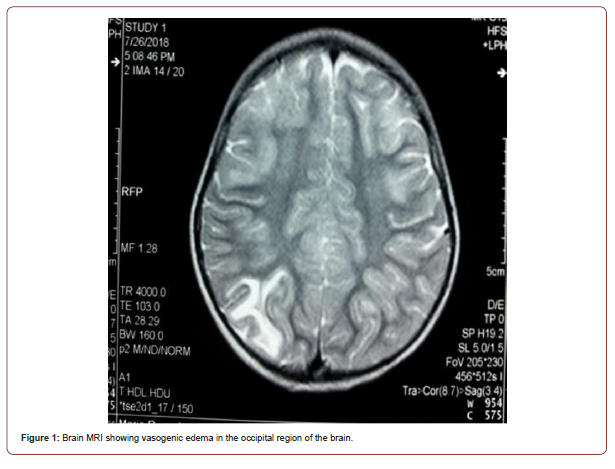
Complete blood count, creatinine, liver function tests, creatinine phosphokinase, lactate dehydrogenase and urine analysis were all normal. Magnetic resonance imaging (MRI) in the second day {July 26, 2018} showed vasogenic edema in the occipital & parietal lobes suggesting PRESS, (Figure-1). She was treated on IV phenytoin to control anticipated seizures.
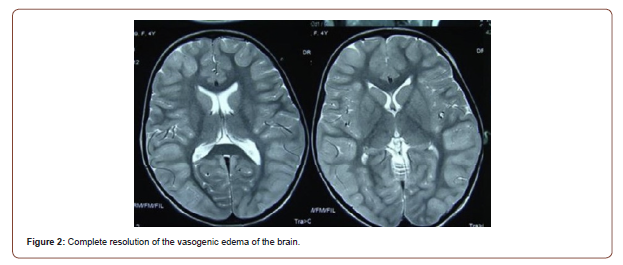
She improved tremendously with physical therapy and rehabilitation and was discharged home after 15-day stay in the hospital. Her general condition improved, however, the low visual acuity, aphasia, and the significant motor weakness persisted. On her follow up one month later, she had tangible clinical improvement, she was talking, walking, and playing with dramatic clinical improvement in her vision and her general condition. She underwent a repeated MRI scan on {September 10th, 2018} which showed complete resolution of the radiological finding (Figure-2).
Discussion
Scorpion envenomization is a significant public health problem in Libya due to the great incidence of scorpion stings in the southern part of the country. Of around 1,500 species of scorpions worldwide, only 30 are potentially dangerous to human [8]. Scorpion sting has many clinical manifestations, such as pain sensation at the sting site, itch, erythema, local tissue swelling, ascending hyperesthesia, Hyperthermia, tachypnea, tachycardia, hypertension, and cardiac arrhythmia [9]. The most common neurological manifestations are ptosis, dysphagia due to paralysis of the pharyngeal muscles, generalized paralysis and hypotonia, and seizure.
Scorpion sting can cause cerebrovascular accidents by various mechanisms such as venom induced autonomic disorders leading to labile blood pressure with episodes of hypertension, and or hypotension, disseminated intravascular coagulation, or vasculitis [6,9]. PRESS is commonly seen in the setting of hypertension or endothelial dysfunction; probably due to a breakdown of cerebral autoregulation [6]. However approximately 20%-40% of patients with PRESS are found to have normal blood pressure [10]. The endothelial dysfunction plays a pivotal role in the presence of cerebral edema by causing increased capillary permeability as result of interplay of multiple factors. In Fact, it has been shown that proinflammatory mediators, either exogenous originating from the venom itself or endogenous induced by the venom brings about the changes in vascular permeability [7,11].
PRESS due to scorpion stings is quite rare. We here presented a case of PRESS due to scorpion stings in normotensive child. The mechanism of PRESS in this patient could be due to systemic immune response mediated reaction to the stings rather than arterial pressure exceeding the limits of cerebral vascular autoregulation. We reviewed the literature for the relationship between insect bites/sting and the occurrence of PRESS and found only few cases of bites or sting followed by PRESS. In three of such patients reported in the literature, PRESS occurred with normal blood pressure [12-14]. Only two cases of PRESS occurred after scorpion sting [6,7]. In four cases PRESS was due to bees or wasp stings [11-15]. Moreover, three out of six cases of PRESS following sting/bites occurred in children as reported in literature [6,7,11- 15]. Two previous cases of PRESS following scorpion sting were reported from brazil [6] and morocoo [7]. High blood pressure is well known cause associated with PRESS; however, normal blood pressure is unusual in PRESS due to any cause.
Ganqin Du, et al. [12] in china report on a case of PRESS in a normotensive woman after wasps’ stings. In the workers’ opinion, the underlying mechanism of PRESS was mediated by systemic immune reaction and or the antigen-antibody complexes. These cascades of events may play an important role in cerebral vasoconstriction which lead to brain edema. The case reported by Gauqin et al may support the view that the pathophysiology of PRESS is much more complex and not follow a uniform pattern [12]. In the current case the BP was normal and the encephalopathic changes as well as the regional cerebral edema in the posterior circulation might be explained by breakdown of the blood brain barrier caused by the inflammatory process incited by the scorpion bite. No other possible cause of encephalopathy could be elicited. Activation of the systemic immune response triggered by the scorpion venom is plausible cause for PRESS if the BP is normal.
Conclusion
This case demonstrate that PRESS can be a complication of scorpion stings even in the presence of normal blood pressure. Neurologists and neuroradiologists as well as clinicians should be cognizant of the ramifications of the spectrum of clinical and radiological changes of PRESS. Managing patients with PRESS encompasses a great deal of both clinical and scientific knowledge.
Acknowledgments
The authors would like to thank Dr. Adel Elmjrab, a radiologist at Benghazi children hospital for providing the MRI scans. Special thanks to the participants who obtained the patient’s Informed consent which makes report of this case possible.
Conflict of Interest
No conflict of interest.
References
- Hinchey J, Chaves C, Appignani B, Breen J, Pao L, et al. (1996) Reversible posterior leukoencephalopathy syndrome. N Engl J Med 22: 494–500.
- Girişgen I, Tosun A, Sönmez F, Özsunar Y (2010) Recurrent and atypical posterior reversible encephalopathy syndrome in a child with peritoneal dialysis. Turk J Pediatr 52: 416-419.
- Jennifer E Fugate, Alejandro A Rabinstein (2015) Posterior reversible encephalopathy syndrome: clinical and radiological manifestations, pathophysiology, and outstanding questions, The Lancet Neurology 14(9): 914-925.
- McKinney AM, Short J, Truwit CL, McKinney ZJ, Kozak OS, et al. (2007) Posterior reversible encephalopathy syndrome: Incidence of atypical regions of involvement and imaging findings. AJR Am J Roentgenol 189: 904–912.
- Prasad N, Gulati S, Gupta RK, Sharma K, Gulati K, et al. (2007) Spectrum of radiological changes in hypertensive children with reversible posterior leucoencephalopathy. Brit J Radiol 80: 422-429.
- Porcello Marrone LC, Marrone BF, Neto FK, Francisco Cosme Costa, Gustavo Gomes Thomé, et al. (2013) Posterior reversible encephalopathy syndrome following a scorpion sting. J Neuroimaging 23: 535-536.
- Houssam Rebahi, Youssef Mouaffak, Mohamed-Othmane Dilai, Nezha Haimeur, Ahmed-Ghassane Eladib, et al. (2015) Posterior Reversible Encephalopathy Syndrome in a Child Stung by Androctonus mauretanicus Scorpion. J Stroke Cerebrovasc Dis 24(6): e129-32.
- Prendini L (2005) Scorpion higher phylogeny and classification, taxonomic anarchy and standards for peer review in online publishing. Cladistics 21: 446-494.
- Petricevich VL (2010) Scorpion Venom and the inflammatory response. Mediators Inflamm 2010: 903295.
- McCoy B, King M, Gill D, Twomey E (2011) Childhood posterior reversible encephalopathy syndrome. Eur J Paediatr Neurol 15: 91-94.
- Del Brutto OH (2013) Reversible posterior leukoencephalopathy after venomous bites and stings. Neurotoxicology 39: 10.
- Ganqin Du, Xiaoli Yang, Xiaowei Du (2017) Posterior reversible encephalopathy syndrome following multiple wasp stings: a case report. Int J Clin Exp Med 10(1): 1446-1448
- Lee M, Park DG, Kim MS, Seo HI, Kim M, et al. (2014) Posterior Reversible Encephalopathy Syndrome Following Bee Venom Acupuncture.J Korean neurol Assoc 32(4): 304.
- Parakh M, Pilania K, Jangid H, Chaturvedy K, Shroff M (2013) Posterior reversible encephalopathysyndrome - a rare complication of bee stings. Can J Neurol Sci 40(3): 431-432.
- Loh HH, Tan CHH (2010) Acute renal failure and posterior reversible encephalopathy.
-
Abdulhamid ElShiky, Emhemed Mousa, Fatma F Almijbri, Awad Magbri. A Case Report of Posterior Reversible Encephalopathy Syndrome in a Libyan Child Stung by Scorpion and Review of the Literatures. Arch Neurol & Neurosci. 10(3): 2021. ANN.MS.ID.000739.
-
Depression, HPA axis, mitochondrial dysfunction, NMDA receptor, Serotonin, Glutamate.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






