 Case Report
Case Report
Substantial Improvement in Intraoperative Motor Evoked Response During Surgery on the Cervical Spine: A Case Report
Hassan Shehab1, Raja Sawaya2, Ragheb Ismail2, Rosemary Khoury1 and Ghassan Skaf1*
1Division of Neurosurgery, Department of Surgery, American University of Beirut Medical Center, Lebanon
2Department of Neurology, American University of Beirut Medical Center, Beirut, Lebanon
Ghassan Skaf, Professor, Division of Neurosurgery, Department of Surgery, American University of Beirut Medical Center, Riad El Solh, 1107-2020, Beirut, Lebanon.
Received Date:December 20, 2023; Published Date:January 04, 2024
Abstract
Some surgeons believe that intraoperative monitoring during cervical spine surgeries might be an expensive superfluous procedure. In this paper, we would like to report an unexpected improvement in motor-evoked responses amplitude, immediately after the cervical spinal cord was decompressed. The patient showed remarkable improvement directly post-operatively and multiple conclusions were drawn in this case. Surgical spinal cord decompression can result in the reversal of neurological deficits and should be implemented whenever possible; in addition, surgical decompression successfully relieves the pressure on the cord and triggers the opening of the channels, which will lead to re-conduction through the nodes of Ranvier. Most importantly, spine surgeons should perform spinal decompression surgeries instantaneously to achieve better results and avoid any irreversible injury to the spine. We concluded that spine surgeons should embrace the concept of monitoring techniques and adequately interpret intra-op records for better decision-making during surgery in order to yield safe and favorable surgical outcomes.
Keywords:Spinal cord; Iintraoperative monitoring; Motor-evoked potentials
Introduction
Some medical professionals consider intraoperative monitoring during surgery on the cervical spine an unnecessary and expensive procedure. Several authors reported their observation that intraoperative improvement in the motor-evoked potentials (MEPs) correlated with a more favorable postoperative clinical outcome [1,2]. We would like to report an unexpected improvement in motor-evoked responses amplitude, immediately after the cervical spinal cord was decompressed.
Case Report
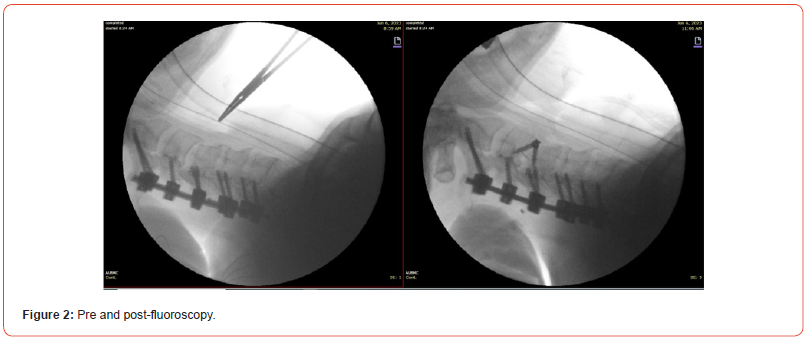
The patient is a 74-year-old male who presented with an incomplete traumatic spinal cord injury and a C3-C4 fracturedislocation. He had undergone C2-C6 posterior decompression and fusion a few weeks prior to the presentation, which resulted in minimal post-operative motor improvement but ongoing diffuse upper and lower extremities numbness and significant spastic gait and imbalance and continued to complain of left-sided hemiparesis and spasticity. On physical examination, he was found to have generalized hyperreflexia and bilateral Hoffman and Babinski signs. Magnetic Resonance Imaging (MRI) of the cervical spine showed prior posterior decompression, fracture dislocation, with perched facets, and anterolisthesis at C3-C4, with upward migrating fragment posterior to C3 vertebral body. The patient underwent a standard anterior cervical discectomy and fusion surgery. The procedure involved cutting the annulus fibrosis, removing the disc material, and drilling down the anterior lip of C3. Later, an insertion was made, using distraction pins, for disc space distraction, and the removal of osteophytes was performed along with the removal of the posterior longitudinal ligament. The superior and inferior endplates were shaved, and the migrated disc fragment, posterior to the vertebral body of C3, was removed. Following the removal of the migrated disc fragment, a relaxed dura was observed, and spinal fusion was executed using a divergence cage.
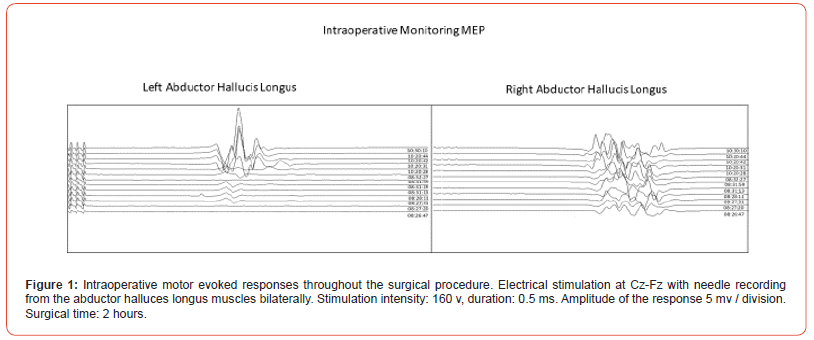
After the surgery, examination revealed decreased arm numbness and partial improvement of the left-sided paresis. Intraoperative sensory (SEP) and MEP were performed during the surgical procedure. The posterior tibial SEPs remained stable, symmetrical, and unchanged throughout the operation. The right MEP, recorded from the extensor halluces longus muscle, had a stable latency and amplitude compared to the preoperative baseline, while the left MEP had a very small amplitude at the onset of the surgery (160 microV). Two hours after the procedure started and when the surgeon was removing the migrated disc fragment, the MEP amplitude increased by 700% to 1123 microvolts at the same magnetic stimulation of the brain (160 volts) (Figure 1).
Case Presentation
A 62 year-old woman with a history of degenerative disc disease, arthritis, neuropathic pain, and a nonruptured 4 mm left M2 aneurysm who presented to the neurology clinic with a reported history of hypertensive crises, lightheadedness with position changes, and a feeling of being cold. The patient’s hypothermic episodes usually began in the evenings, lasted through the night, and she would wake in the early morning hours shivering. These episodes could last between 8 and 12 hours. During the hypothermic episodes the patient reported an experience of “unawareness” of her body. EEG testing was negative for seizures. The patient’s self temperature monitoring on a standard oral thermometer revealed a temperature that was often below 98 degrees F (36.67 degrees C). She frequently reported temperatures of 96 degrees F (35.56 degrees C) and occasionally as low as 94 degrees F (34.44 degrees C) temperarature changes summarized in Table 2. Triggers to the hypothermic episodes included stress and infection. The patient also had difficulties with orthostatic hypotension (drop of SBP >20 when changing positions) with her systolic blood pressure dropping below 100 mmHg when she stood up. Tilt table testing provided no evidence of predispoisiton to neurally mediated syncope or exaggerated postural tachycardia, however tilt testing revealed measure of parasympathetic and sympathetic adrenergic function is abnormal, with normal sympathetic cholinergic function. Her neurological exam revealed normal cognitive testing, cranial nerve function, motor strength, reflexes, coordination and gait. Her sensory exam revealed a small fiber neuropathy; sensory polyneuropathy with a stocking/glove deficit in pinprick sensation. The results of a skin biopsy of PGP9.6 immunolabeled sections showed severe distal small fiber neuropathy with reduction of epidermal innervation with the retention of the dermal and dermal gland innervation. Morphemetric quantitation of epidermal nerve ending yielded epidermal neutirte density of 14 neurites/mm2 skin,. This is below the 5th percentile threshold resulting in a diagnosis of small fiber neuropathy. Diabetes mellitus was ruled out due to the lack of supporting lab results. The diagnosis of multiple system atrophy was also excluded due to a lack of parkinsonism features, cerebellar ataxia and lack of significant imaging such as atrophy of the putamen pons or cerebellum, and no indication of MSA on TILT table testing. An MRI of the brain did not reveal any structural issues and a full endocrine panel including T3,T4, ferritin, B12 and Vitamin D were normal. An EMG ruled out large-fiber peripheral neuropathy. There was no infectious or pharmacological causes identified for the autonomic insuffiency.
Discussion
The administered anesthesia dose remained stable throughout the procedure, and no physiological changes were observed intraoperatively. The changes in motor-evoked responses (MEPs) were limited to the left leg and not the right, indicating that they occurred due to the alleviation of the conduction block at the site of the insult. These changes were noticed instantaneously, ruling out remyelination or axonal sprouting as the cause. Instead, they are attributed to the opening of previously blocked sodium channels at the nodes of Ranvier, caused by focal compression and local edema [3,4].
This case and its results lead to several important conclusions. Firstly, surgical spinal cord decompression can lead to the reversal of neurological deficits and should be pursued whenever feasible. Although the improvement may not be immediately evident postoperatively, the normalization of motor-evoked responses during surgery indicates potential clinical improvement. Voulgaris et al. demonstrated significant recovery from motor dysfunction at one-year follow-up in 17 patients who experienced a greater than 50% increase in MEP amplitude during 25 lumbar laminectomies for lumbar spinal canal stenosis [5]. Similarly, Wang et al. revealed that improvements in MEP amplitude after cervical spine decompression are indicative of a favorable prognosis in patients with cervical compression myelopathy [6]. Secondly, this study highlights the importance of extending surgical decompression to its limits, ensuring complete relief of compression on the spinal cord. By doing so, the opening of channels and re-conduction through the nodes of Ranvier can be triggered. We hypothesize that, in conjunction with intraoperative neuro-monitoring, deliberate efforts to decompress the areas both cephalad and caudal to the segmental compression site should become a fundamental practice in anterior cervical decompression. Failure to reach this critical point in decompression could result in procedural failure.
Thirdly, intraoperative MEP monitoring should be performed in all spinal cord surgeries to detect and attempt to reverse any asymmetry or pathology noticed at baseline. Collaboration between the surgeon and the electrophysiologist is vital in achieving this goal. Implementing MEP monitoring intra-operatively ensures that subtle changes, which may result in future clinical improvement, are detected and addressed. The benefits of MEPs in assessing the functional integrity of descending motor pathways, from the motor cortex to peripheral muscles, have been recognized by Park and Hyun [7]. Lastly, surgical decompression of the spinal cord should be performed without delay as the changes we observed, in this case, could not have occurred if the decompression was delayed and the injury would have become irreversible. Intraoperative monitoring should be performed in all spine surgeries for a safer and better surgical outcome.
Finally, the findings of this case report are specific to the individual patient described and may not be broadly generalizable to all cases of cervical spinal cord compression. The purpose of this case report is to highlight a unique improvement in MEPs following surgical decompression and the potential implications of such findings. Furthermore, we suggest the need for further research involving larger patient cohorts to establish the broader clinical relevance and applicability of these observations.
Acknowledgments
The author and co-authors have nothing to disclose in terms of financial grants or funding and have no competing interests regarding the submitted article. We also authorize to reproduce figures, tables, or a substantial block of text in both print and electronic forms. All participating authors have read the manuscript, agreed the work is ready for submission to a journal, and accepted responsibility for the manuscript’s contents.
Conflict of Interest
No Conflict of interest.
References
- Akbari KK, Badikillaya V, Venkatesan M, Hegde SK (2022) Do Intraoperative Neurophysiological Changes During Decompressive Surgery for Cervical Myeloradiculopathy Affect Functional Outcome? A Prospective Study. Global Spine J 12(3): 366-372
- Park MK, Lee SJ, Kim SB, Kyeong Woo Lee, Hye-Jeong Lee, et al. (2018) The effect of positive changes during intraoperative monitoring of the functional improvement in patients with cervical compressive myelopathy. Clin Interv Aging 13:1211-8
- Jamaludin MR, Wee Lai K, Chuah JH, Muhammad Afiq Zaki, Yan Chai Hum, et al. (2021) Transcranial Electrical Motor Evoked Potential in Predicting Positive Functional Outcome of Patients after Decompressive Spine Surgery: Review on Challenges and Recommendations towards Objective Interpretation. Behav Neurol: 2684855.
- Visser J, Verra WC, Kuijlen JM, Horsting PP, Journee HL (2014) Recovery of TES-MEPs during surgical decompression of the spine. J Clin Neurophysiol 31(6): 568-574
- Voulgaris S, Karagiorgiadis D, Alexiou GA, Evaggelos Mihos, Andreas Zigouris, et al. (2010) Continuous intraoperative electromyographic and transcranial motor evoked potential recordings in spinal stenosis surgery. J Clin Neurosci 17(2): 274-276.
- Wang S, Tian Y, Wang C, Xin Lu, Qianyu Zhuang, et al. (2016) Prognostic value of intraoperative MEP signal improvement during surgical treatment of cervical compressive myelopathy. Eur S J 25(6): 1875–1880.
- Park JH, Hyun SJ (2015) Intraoperative neurophysiological monitoring in spinal surgery. World J Clin Cases 3(9): 765-773
-
Hassan Shehab, Raja Sawaya, Ragheb Ismail, Rosemary Khoury and Ghassan Skaf*. Substantial Improvement in Intraoperative Motor Evoked Response During Surgery on the Cervical Spine: A Case Report. Arch Neurol & Neurosci. 16(3): 2024. ANN.MS.ID.000888.
-
Acute Polyradiculoneuritis, Neurology, Guillain-barre; Fann teaching hospital, neuropathy, cranial nerves, immunotherapy, Neuroscience, neurogenic syndrome, epidemiological, Dysphonia.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






