 Mini Review
Mini Review
Is Sensitive Skin a Disease, a Syndrome, a Disorder or Else?
Kam Tim Michael Chan*
Specialist in Dermatology, Hong Kong Academy of Medicine, Hong Kong SAR, China
Kam Tim Michael Chan, Specialist of Dermatology, Adjunct Professor of Master Course of Common Goods and Public Health, Baptist University of Hong Kong, China, KTM Chan 2128-2129, Pioneer Centre, 750, Nathan Road, Mongkok, Kowloon, Hong Kong SAR, China.
Received Date: February 10, 2020; Published Date: February 18, 2020
Abstract
Sensitive skin is a complex global challenge awaiting upcoming solution. Till now, the exact pathogenetic mechanism, neuro psycho-cognitive pathway of sensitive skin is unknown. One of the difficulties lies on the fact that there is an absence of objective diagnostic test to define the disease. Even worse, authorities have been arguing whether sensitive skin is a disease, disorder, syndrome or simply a psychological symptom with unpleasant sensations. The following is a discussion paper attempting to frame sensitive skin as a syndrome based on the current scientific findings based on a biopsychosocial model.
Keywords: Sensitive skin syndrome; Biopsychosocial model; Epidermis neurological continuum; DSM disease criteria
Introduction
Sensitive skin is a common acute skin condition that prompt patients seeking immediate medical attention in private care clinic setting [1]. The worldwide prevalence is reported to be 40% [2- 5]. It was estimated up to 10% may seek medical consultation and presented with severe sensitive skin symptoms and signs [6]. The most significant triggering factors of sensitive skin according to a systemic literature reviewed are cosmetics, wet air, air conditioning, heat and water. Other triggering factors were physical variations in temperature, cold, wind, solar radiation, air conditioning, dry air, chemical, pollution and emotional factors [7]. Albeit a widely publicized entity, its exact etiology, characteristics and genetics constitution of patients, pathogenesis and treatment of the condition are still obscure. There are general disagreements among neuroscientists, dermatologists and psychologists whether sensitive skin is a real disease, disorder, syndrome or a mere psychological symptom in a normal person.
International Forum for the Study of Itch (IFSI) defined sensitive skin as a syndrome by the occurrence of unpleasant sensations (stinging, burning, pain, pruritus, and tingling sensations) in response to stimuli that normally should not provoke such sensations [5]. These unpleasant sensations cannot be explained by lesions attributable to any skin disease. It significantly affected Quality of Life (QoL) and health of patients and its family members. Despite advancement of science, no diagnostic test and evidenced based treatment study existed for its management. Thus, the diagnosis is clinical or aided by a patient self -reported questionnaires. Inconsistences due to cultural, social and semantic inter-individual variations may give rise to over or underestimation of the true prevalence and incidence of the syndrome; defining a genuine case for in-vivo and in-vitro research study may be inaccurate, imprecise and difficult.
As for the highest order of conceptual scientific understanding under DSM IV definition, sensitive skin based on our current evidence -based knowledge, is not a disease as this is a disorder without a known etiology [8]. However, human diseases like notions of health are highly context-dependent, human diseases only exist in relation to people, and people live in varied cultural contexts [9]. Studies in medical anthropology and sociology have shown that whether people believe themselves to be ill varies with class, gender, ethnic group and less obvious factors such as proximity to support from family members. What counts as a disease also changes over historical time, partly as a result of increasing expectations of health, partly due to changes in diagnostic ability, but mostly for a mixture of social and economic reasons. Hence, one should be intuitive as scientific and clinical experience on sensitive skin advances in future, a physiological natural process may well re-classify as a disease especially in an ever changing contextual, cultural, societal and historical environments.
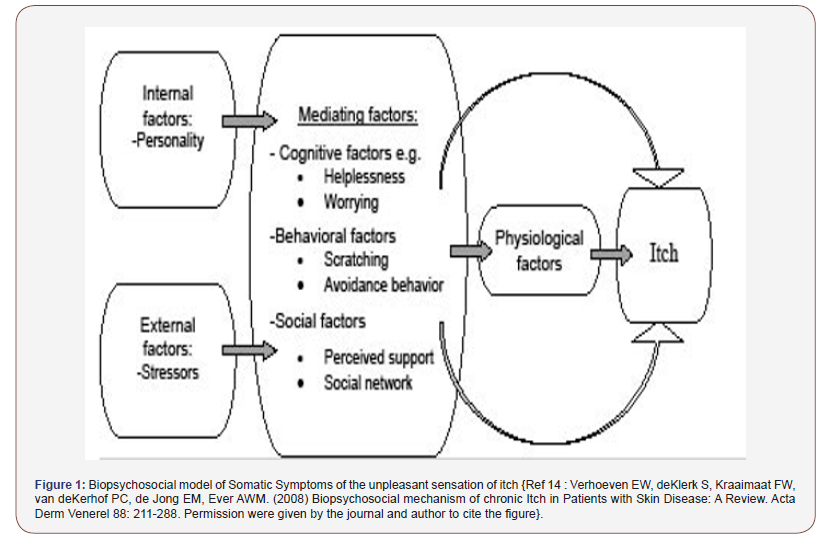
How about is sensitive skin a disorder? A disorder referred to a cluster of symptoms but the concept includes the idea that the set of symptoms is not accounted for by a more pervasive condition [8]. As part of DSM criteria, a disorder is usually defined as something that is of longer duration (at least 3 – 6 months); causes significant impairments of daily activities and is usually not very prevalent. As mentioned, sensitive skin syndrome is a prevalent condition reported worldwide up to 40% or even higher in some countries and culture. The high prevalence may not satisfy the DSM IV criteria as a disorder. However, in some documented epidemiological studies, very sensitive and sensitive skin has a lower prevalence of up to 12% and in some clinic based prospective study, the prevalence is around 7% [10-12]. In addition, in this sub-group of sensitive skin sufferers who seek medical care or who may well have very sensitive and sensitive skin has significant dysfunctional sensation especially over but not limited to the face, negative percept and psychological complications [13]. Sensitive skin may be regarded as a disorder under such circumstances especially in a clinic setting through the mediating cognitive factors of helplessness, worrying, behavioral factors like scratching, avoidance behavior and social factors like lack of perceived support and social network (Figure 1) [14].
Finally, IFSI definition of sensitive skin provide us the broadest or open-ended level of definition which future knowledges may be built upon. Syndrome under DSM IV is applied to a constellation of symptoms that occur together or co-vary over time. Syndrome carries no direct implications in terms of underlying pathology. Whether certain sets of symptoms co-vary with one another is an empirical question. In the community based and public health setting; summarizing our current incomplete picture of this interesting sensitive skin phenomena, sensitive skin syndrome might still be the best definition for the problem of sensitive skin. The validity of this definition of sensitive skin will be testify through time, vigilant psychometric, neurological, dermatological clinical test-retest trial and researches.
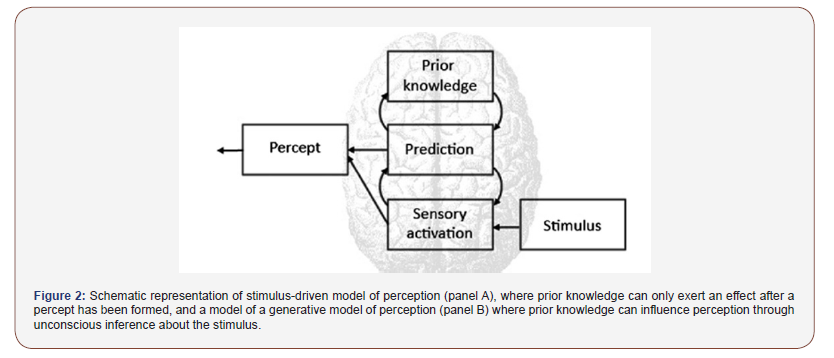
While whether sensitive skin syndrome is a syndrome, physiological condition or pathological disorder is still debatable. Sensitive skin syndrome maybe regarded as a spectrum of skin epidermis neurological continuum with stimulus, cognitive and patient distinct perceptive involvement. SSS based on an established biopsychosocial model and perspective [14] (Figure 1). Based on this biopsychosocial model focusing on psychoneurobiological mechanisms; perhaps; may serve as one of the better approaches of this syndrome [15] (Figure 2).
In sum, the above discussion may not be agreeable to all scientists working in this syndrome, the short discourse hope to serve as a starting point to address the basic definition of a common condition with escalating prevalence in industrialized society. 16 More questions are raised in contemplating this sensitive subject: is sensitive skin a pathological, physiological or psychological phenomenon? What is the relationship between the cause and events of the unpleasant sensational sufferings? Are the neurological unpleasant sensations a result of cognitive, emotional sufferings? Reduced to basics, our dermatological experts would like to dichotomous is sensitive skin a dermatological disease, cosmetic disease, a mixture of both or neither of these.
Acknowledgement
Professor Laurent Misery, University of Brest, France and Professor A.W.M. Evers, University of Leiden, Netherlands for their discourse.
Conflict of Interest
No conflict of interest.
References
- Chan KTM (2018) Clinical Review on Sensitive Skin: History, Epidemiology, Pathogenesis and Management. J Clin Exp Dermatol Res 9: 453.
- Misery L, Myon E, Martin N, Verrière F, Nocera T, et al. (2005) Sensitive skin in France: An epidemiological approach. Ann Dermatol Venereol. 132: 425-429.
- Misery L, Boussetta S, Nocera T, Perez-Cullell N, Taieb C (2009) Sensitive skin in Europe. J Eur Acad Dermatol Venereol 23: 376-381.
- Misery L, Sibaud V, Taïeb C (2011) Sensitive skin in the American population; Prevalence, clinical data and role of the dermatologist. Int J Dermatol 50: 961-967.
- Misery L, Stander S, Szepietowski JC, Reich A, Wallengren J, et al. (2017) Definition of sensitive skin: An expert position paper from the special interest group on sensitive skin of the international forum for the study of itch. Acta Derma Venereol 97: 4-6.
- Chan KTM (2019) A Prospective Study on the Characteristics of Sensitive Skin Patients Attending a Private Clinic-Based Setting in Hong Kong. Itch 4: e30 p54-PP78.
- Brenaut E, Barnetche T, Le Gall-Ianotto C, Roudot AC, Misery L, et al. (2019) Triggering factors in Sensitive Skin from the worldwide patient’s point of view: a systematic literature review and meta-analysis. J Eur Acad Dermatol Venereol 34(2): 230-238.
- Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, 1994 (DSM-IV)
- Scully JL (2004) What is a disease? EMBO reports 5(7): 650-653.
- Xu F, Yan S, Wu M, et al. (2013) Self – declared sensitive skin in China. A community -based study in three top metropolises. J Eur Acad Dermatol Venereol 27: 370-375.
- Chan KTM, Cheung AHN (2019) A Community epidemiological survey on the prevalence and risk factors of sensitive skin syndrome in Hong Kong using a validated sensitive scale (SS-10) questionnaire. Itch 4: e30 p24.
- Chan KTM, Cheung AHN (2019) A Prospective study on the characteristics of sensitive skin patients attending a private - clinic based setting in Hong Kong. Itch 4: e30 p54; PP78.
- Misery L1, Myon E, Martin N, Consoli S, Boussetta S, et al. (2007) Sensitive Skin: Psychological effects and seasonal changes. J Eur Acad Dermatol. Venereol 21: 620-628.
- Verhoeven EW, de Klerk S, Kraaimaat FW, van de Kerkhof PC, de Jong EM, et al. (2008) Biopsychosocial Mechanism of Chronic itch in Patients with Skin Disease: A Review. Acta Derm Venereol 88: 211-218.
- Henningsen P, Gündel H, Kop WJ, Löwe B, Martin A, et al. (2018) Persistent Physical Symptoms as Perceptual Dysregulation: A Neuropsychobehavioral Model and Its Clinical Implications 80(5): 422-431.
-
Is Sensitive Skin a Disease, a Syndrome, a Disorder or Else?. Arch Neurol & Neurosci. 7(1): 2020. ANN.MS.ID.000655.
-
Sensitive skin syndrome, Biopsychosocial model, Epidermis neurological continuum, DSM disease criteria, Dermatology, Physiological, Psycho neurobiological, Cosmetic disease.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






