 Case Report
Case Report
Rare Complication of Microvascular Decompression: Delayed Facial Paralysis
Preeti Singh*, Harsh Patel, Abhaya Kumar
Department of Neurosurgery, Kokilaben Dhirubhai Ambani Hospitals & Research Institute, Mumbai
Preeti Singh, Department of Neurosurgery, Kokilaben Dhirubhai Ambani Hospitals & Research Institute, Mumbai
Received Date:April 05,2025; Published Date:May 07, 2025
Microvascular Decompression (MVD) is indeed a highly effective treatment for Trigeminal Neuralgia (TN), especially when there is vascular compression of the trigeminal nerve. We present one such case of a young female presenting with left sided facial pain with V2, V3 distribution from 4 months, illustrates a common clinical scenario where MVD offers significant relief for TN, particularly when the radiological findings, such as a loop of the Superior Cerebellar Artery (SCA) abutting the trigeminal nerve, confirm vascular compression. The development of facial paralysis in the follow-up period, though rare, is a potential complication of MVD, and it highlights the complexities of the procedure. Facial paralysis can result from several mechanisms, including: inadvertent injury to the facial nerve: During the MVD surgery, the facial nerve, which lies in close proximity to the trigeminal nerve, can be at risk. Even a small amount of trauma to the facial nerve can lead to temporary or permanent weakness. Post-surgical swelling or inflammation: Following MVD, the surrounding tissues, including the facial nerve, can experience swelling or inflammation. This may temporarily impair the function of the facial nerve. Anatomical variations: Variations in the anatomy of the vascular structures or the proximity of the facial nerve can increase the likelihood of facial nerve involvement during decompression. The management of post-operative facial paralysis typically involves a thorough evaluation to determine whether the condition is transient (due to inflammation or mild injury) or more persistent, which might require further intervention. Conservative treatments, such as corticosteroids or physical therapy, are often recommended for mild cases, while more severe or persistent cases might necessitate additional surgical approaches.
Keywords:Keywords: MVD microvascular decompression; DFP delayed facial paralysis; trigeminal neuralgia
Case 1
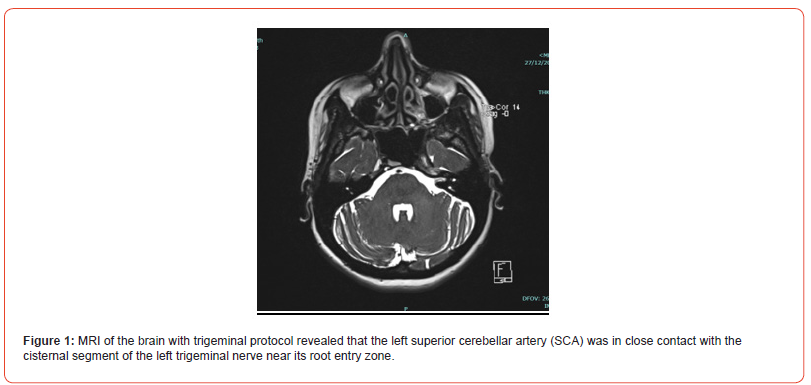
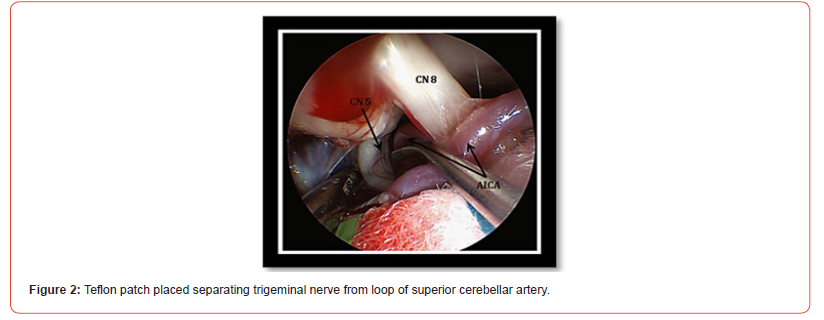
A 44-year-old woman with a history of hypertension and a chief complaint of left-sided facial pain in the V2 and V3 distributions, which had been ongoing for 4 months. MRI of the brain with trigeminal protocol revealed that the left Superior Cerebellar Artery (SCA) was in close contact with the cisternal segment of the left trigeminal nerve near its root entry zone, indicating a potential cause for trigeminal neuralgia. She underwent Microvascular Decompression (MVD) surgery, a common procedure used to relieve trigeminal neuralgia by separating the offending vascular structures from the trigeminal nerve, which led to resolution of her facial pain. However, during follow-up, the patient developed grade 1 facial paralysis, which suggests a complication related to the surgical intervention. (Figure 1 & 2)
Follow up after 1 week

Patient presenting with grade 1 facial paresis and mild imbalance while walking. (Figure3)
Facial Paralysis after MVD
Facial paralysis following microvascular decompression can occur
due to a few possible reasons:
1. Direct Injury to the Facial Nerve: The facial nerve (cranial
nerve VII) runs in close proximity to the trigeminal nerve in the
brainstem and may be inadvertently injured during the surgical
procedure, especially if the decompression requires manipulation
of surrounding structures.
2. Trauma from Retraction: In some cases, retraction of the
cerebellum or the brainstem during surgery may cause mechanical
injury to the facial nerve.
3. Post-operative Edema or Compression: After MVD,
post-operative swelling or hematoma can put pressure on the
facial nerve, leading to temporary or permanent paralysis.
4. Ischemia or Vascular Compromise: There is also a risk of
ischemia to the facial nerve if blood flow is disrupted during the
surgery, although this is less common.
5. Pre-existing Subclinical Facial Nerve Dysfunction: In some
cases, a prior undiagnosed issue with the facial nerve (such as
minor compression or preexisting vulnerability) may become
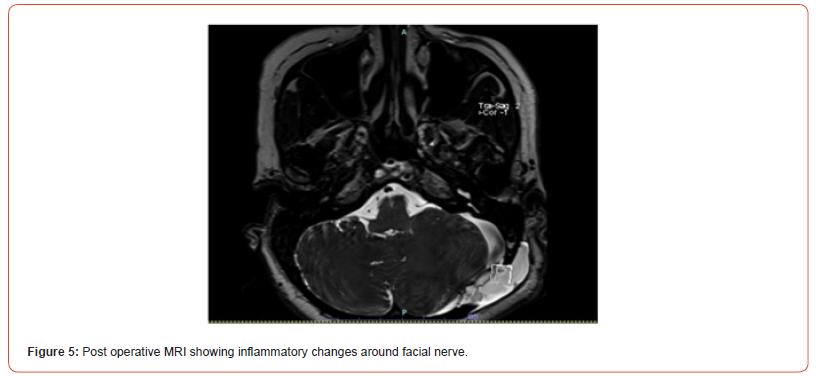
symptomatic postoperatively. Repeat MRI done shows pseudomenigocele
and inflammatory changes around facial nerve.
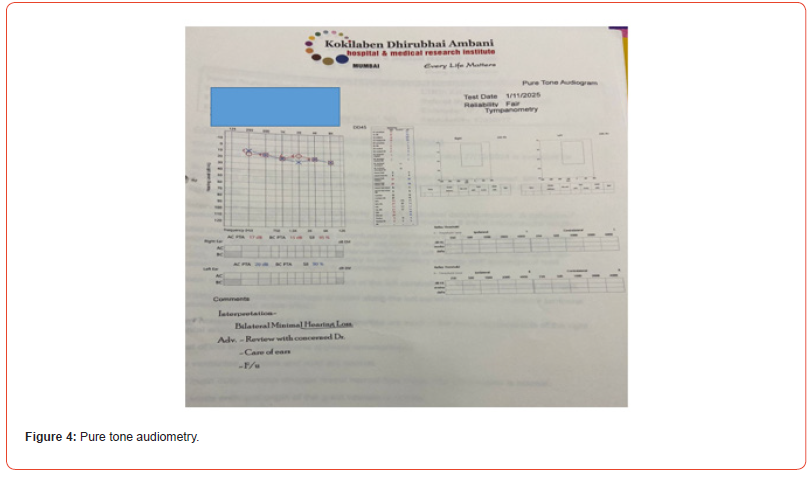
Patient was started on high dose steroid there was gradual improvement
in the facial weakness and gait. Pure tone audiometry
showed bilateral minimal hearing loss. No retraction injury
to auditory nerve. (Figure 4 & 5),
Discussion
It is crucial to thoroughly evaluate and monitor post-surgical conditions. Delayed facial weakness may be attributed to gradual edema occurring after surgery. The use of Teflon to separate nerve tissue and blood vessels, although beneficial, can sometimes be perceived as a foreign body leading to inflammation. [1-4] Facial weakness can be managed with facial muscle exercises without requiring special treatment. [5-7] Several treatments have been proposed to address DFP including steroids, acyclovir, and facial canal decompression. But in most cases spontaneous resolution occurs, and the average duration of improvement is 5.7-9 weeks. [8,9]
Acknowledgement
None.
Conflict of Interest
None
References
- Thomas Günther, Venelin M Gerganov, Lennart Stieglitz, Wolf Ludemann, Amir Samii, et al. (2009) Microvascular decompression for trigeminal neuralgia in the elderly: long-term treatment outcome and comparison with younger patients. Neurosurgery 65(3): 477-482.
- Jae-Suk Han, Jeong-Ah Lee, Doo-Sik Kong, Kwan Park (2012) Delayed cranial nerve palsy after microvascular decompression for hemifacial spasm. J Korean Neurosurg Soc 52(4): 288-292.
- G Lakshmi Prasad, Vinod Kumar, Girish Menon (2017) Delayed facial palsy after microvascular decompression: report of two cases. J Neurosci Rural Pract. 8(3): 461-465.
- Kong DS (2020) Possible Complications of Microvascular Decompression. in Hemifacial Spasm 135-139.
- Gianoli GJ (2002) Viral titers and delayed facial palsy after acoustic neuroma surgery. Otolaryngol Head Neck Surg 127(5): 427-431.
- Bharat Guthikonda, Myles L Pensak, Philip V Theodosopoulos (2010) Delayed facial palsy after the anterior petrosal approach: case report and review of the literature. Neurosurgery 66(4): E845-846.
- D J Rhee, D S Kong, K Park, J A Lee (2006) Frequency and prognosis of delayed facial palsy after microvascular decompression for hemifacial spasm. Acta Neurochir (Wien) 148 (8): 839-843.
- KIM BT (1999) Delayed facial palsy following microvascular decompression in hemifacial spasm patients. J Korean Neurosurg Soc 1332-1336.
- C Scheller, C Strauss, R Fahlbusch, J Romstöck (2004) Delayed facial nerve paresis following acoustic neuroma resection and postoperative vasoactive treatment. Zentralbl Neurochir 65(3): 103-107.
-
Preeti Singh*, Harsh Patel, Abhaya Kumar. Rare Complication of Microvascular Decompression: Delayed Facial Paralysis. Arch Neurol & Neurosci. 17(4): 2025. ANN.MS.ID.000918.
-
Dolichoectasia, Mental Impairment, Hearing Loss, Nevocellular Nevi, Flat Noses, Hypopigmentation, Dolichoectasia, Seizures.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






