 Research Article
Research Article
Independent C5 And C6 Superior Trunks of The Brachial Plexus with An Anomalous Origin of The Pectoral Nerves
Dominique DiGiacomo1, Paola Pedraza Cruz1, Eric M Lassiter1, Ambika Sood1, Wendy Lackey-Cornelison1 and Adel Maklad1,2*
1Department of Medical Education, College of Medicine and Life Sciences, University of Toledo, Toledo, OH 43614, USA
2Department of Neurosciences, College of Medicine and Life Sciences, University of Toledo, Toledo, OH 43614, USA
Adel Maklad, Department of Medical Education & Department of Neurosciences College of Medicine and Life Sciences, University of Toledo, USA.
Received Date:Febraury 08, 2024; Published Date:February 21, 2024
Abstract
Background: The superior trunk of the brachial plexus provides innervation of the upper arm and shoulder regions, formed from nerve roots
C5 and C6. The suprascapular nerve branches off the upper trunk, supplying innervation to the supraspinatus and infraspinatus muscles. Existing
literature documents variations in the brachial plexus structures. Although the functional impact of these anomalies can vary, it is crucial to document
them to expand on anatomical knowledge of the brachial plexus.
Methods: A unique variation of the superior trunk of the brachial plexus was discovered during a routine educational dissection in a male
cadaver. The current authors present a case of a non-union of the C5 and C6 nerve roots at the upper trunk of the brachial plexus, along with
variations in the structure and branching pattern of downstream nerves.
Discussion: While anatomical variations of the brachial plexus are not uncommon, anomalies of the upper trunk are not well documented.
Specifically, variations in the C5 and C6 nerve roots can have effects such as plexopathies and other clinical disorders. Understanding these variations
is particularly important for surgeons, as the upper trunk is a landmark during shoulder arthroscopy, rotator cuff repair, shoulder replacement
surgery, and nerve blocks.
Conclusion: The current case report documents a variation of the upper trunk with the purpose of expanding current literature and
understanding of anatomical variations within the brachial plexus. Due to the post-mortem nature of the current report, the scope is limited and
there is no certainty regarding the effects of this anomaly on physiology.
Introduction
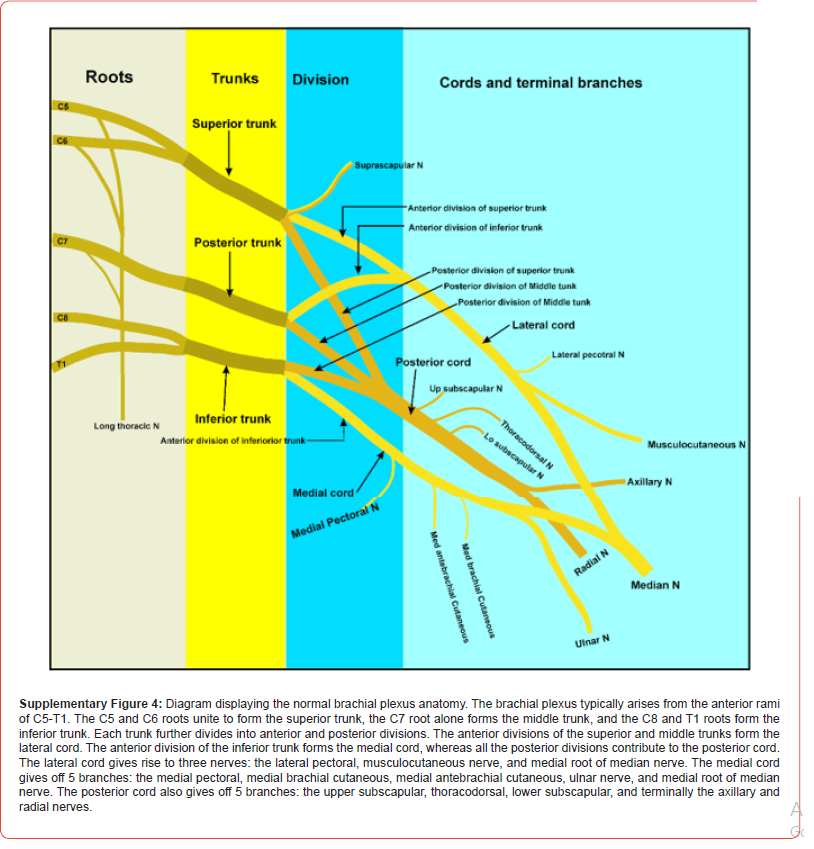
Understanding the upper trunk of the brachial plexus can be the ticket to a successful patient encounter, surgery, or other circumstances that require knowledge of human anatomy. Due to the commonality of anomalies or variations in this region, both motor and sensory innervations to the upper limb may be affected and thus, appreciated by physicians and medical students alike [1]. The brachial plexus is an intricate connection of nerves formed from the ventral rami of nerve roots C5-C8 and the first thoracic spinal nerve, T1. It supplies motor and sensational input to musculature of the upper extremity. The normal anatomical formation of the plexus begins at the posterior triangle of the neck and extends into the axilla at the angle between the clavicle and the lower posterior bor der of the sternocleidomastoid muscle. This allows the nerve fibers, derived from the spinal cord, to be distributed to the nerve trunks supplying various parts of the upper limb [2]. The nerve roots C5 and C6 normally unite to form the upper trunk, while C7 gives rise to the middle trunk, and C8-T1 unite to form the lower trunk. At the level beneath the pectoralis minor, each trunk splits into an anterior and posterior division. The anterior divisions unite to form the lateral and medial cords, and the posterior divisions form the posterior cord. The cords then give rise to the terminal branches that innervate upper limb muscles [3].
As this network of nerves is especially complex, anatomical variations in the brachial plexus are not infrequent and have been reported in up to 35% of patients [4]. Brachial plexus variations can arise due to genetic abnormalities, birth defects, or even trauma, and are typically asymptomatic, encountered incidentally during cadaveric dissections or autopsies. Unique anomalous of the brachial plexus can however affect the use of local anesthesia or successful surgical interventions in the axillary region and the arm [1]. An anomalous upper trunk of the brachial plexus, more specifically at nerve roots C5-C6, can develop a plexopathy which simulates a C5 or C6 root lesion, thoracic outlet syndrome, among other clinical disorders [5,6]. Understanding anomalies of the brachial plexus is of great importance, particularly for surgeons, as knowledge of these variations can be crucial during procedures nerve blocks and surgical interventions involving the brachial plexus [7].
The current case presents a failed union of the ventral rami of nerve roots C5 and C6, consequently leading to an anatomical variation of the upper trunk of the brachial plexus. This observation was discovered upon dissection of a donor cadaver during routine medical education. This unique variation of the upper trunk is almost identical to a cadaveric specimen finding that was presented in 2011 by Adam et al. In this paper, we will discuss the implications of such an anomaly and why further awareness of the brachial plexus is imperative.
Methods
Disclaimer Regarding Use of Human Donor Patients
The cadaver referenced in this study was obtained through a university anatomical donation program through which the patient provided written informed consent for the utilization of their remains for the purposes of medical education and research such as this. The dissection of the donor body, specimen preparation, and variation discovery were performed following established university protocols of good practice. The authors of this case report offer their sincerest thanks to all those who have participated in the anatomical donation program. Their donation aids in the education of future physicians and the discovery of anatomical variations and anomalies such as this one, which can improve patient care in the future and further our knowledge in the fields of anatomy and medicine as a whole [8].
Anatomical Dissection
The current case report was discovered during routine dissection in a student medical education anatomy laboratory. After removing the skin and superficial fascia, the pectoralis muscles were reflected, the axillary sheath was opened using blunt dissection. The axillary vein and associated branches were removed for better visualization of the plexus. The musculocutaneous nerve was then identified at the insertion into the coracobrachialis and followed proximally to the lateral cord of the brachial plexus. The remaining branches, cords, trunks, and roots were carefully teased out using blunt dissection [9].
Case Report
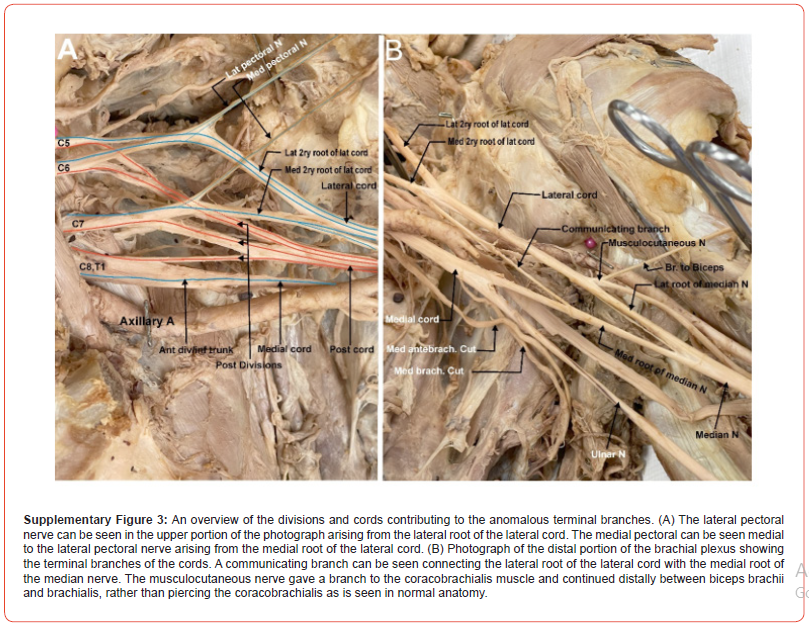
During routine dissection of the right brachial plexus in 87-year-old male (cause of death ischemic cardiomyopathy), we found that the anterior rami of C5 and C6, which normally unite to form the superior trunk, remained separate and each acted as a trunk by dividing into two divisions. The entire plexus was carefully dissected to demonstrate the full details of the variation and identify any additional anomalies that may have resulted from the C5 and C6 variants. An illustration of the brachial plexus described in the current case report is provided in Figure 1 and will be referenced for the majority of the case presentation. Photographs of the cadaveric dissection demonstrating the anomalous plexus can be found in the supplementary figures (Supplementary Figures 1-3). The branching of the anomalous plexus was traced on the original image to facilitate interpretation, with red lines indicating contributions to the posterior divisions and blue lines for contributions to anterior divisions (Supplementary Figure 2 and 3). An illustration demonstrating the normal anatomy of the brachial plexus was included for comparison (Supplementary Figure 4).
Anomalies in roots and trunks:
In contrast to normal brachial plexus, where all roots (C5-T1) emerge between the anterior and middle scalene muscles, C5 and C6 roots emerged by piercing through the anterior scalene muscle while the remaining roots (C7-T1) emerged normally between the anterior and middle scalene muscles (suppl fig. 1). Rather than the anterior rami of C5 and C6 roots joining to form a traditional superior trunk, each root behaves as an independent trunk, giving rise to their own anterior and posterior divisions (figure 1). The anomalous plexus therefore has four true trunks, a superior trunk composed of C5, an upper middle trunk composed of C6, a lower middle trunk composed of C7, and an inferior trunk composed of C8 and T1 (suppl. Fig. 1)..

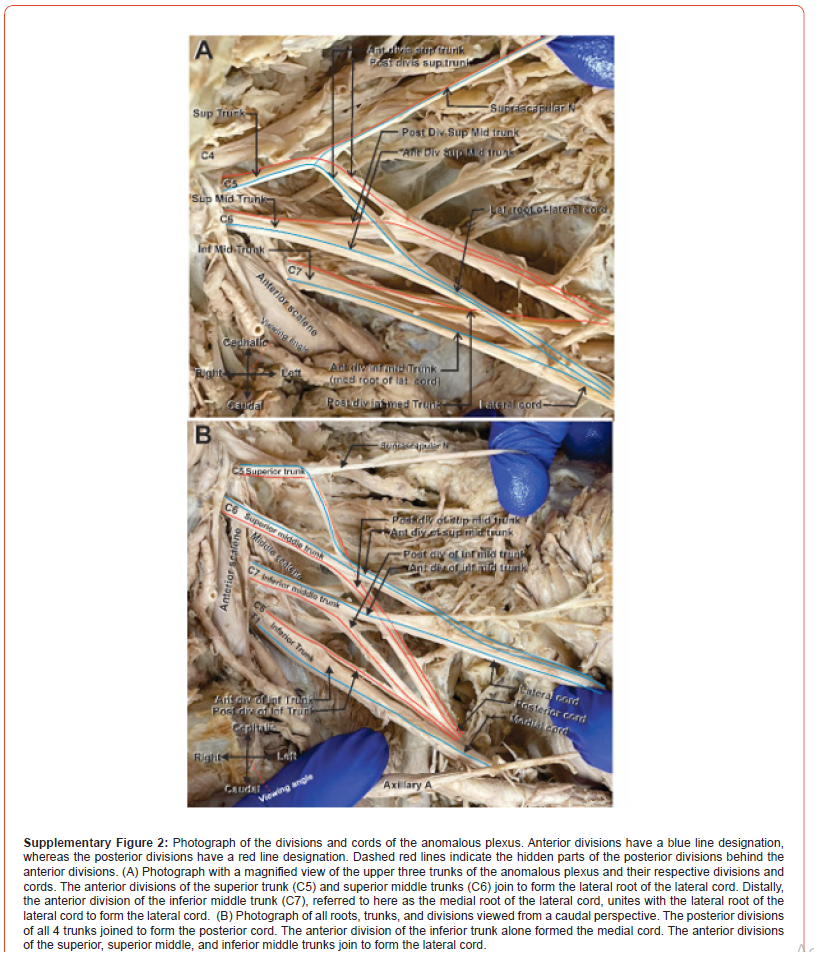

Anomalies in the divisions, cords, and terminal nerves:
Due to the anomalous anatomy of the brachial plexus trunks, eight divisions of the brachial plexus emerged from the four trunks, as opposed to six divisions emerging from three trunks in normal anatomy (Figure 1). The anterior divisions of the superior and upper middle trunks unite to form a portion of the lateral cord, which we refer to here as the lateral root of the lateral cord (C5, C6). The anterior division of the lower middle trunk (C7), which we refer to here as the medial root of lateral cord, joined the lateral root of lateral cord to form the complete lateral cord (Figure 1). Variations in the origin of smaller branching nerves also existed. The lateral pectoral nerve, which typically arises from the lateral cord, arose here from the lateral root of the lateral cord. Furthermore, the medial pectoral nerve, which typically arises from the medial cord, arose here from the medial root of the lateral cord. A communicating nerve branch was also identified, emerging proximally from the medial root of lateral cord, and connecting distally to the medial root of median nerve (Figure 1).
The posterior cord formed from the four posterior divisions of the four trunks, with the posterior divisions of the superior and superior middle trunk joining together first, followed by the posterior division of the inferior middle trunk and finally the posterior division of the inferior trunk. The medial cord was formed from the anterior divisions of C8 and T1 alone, as in the traditional plexus. After formation of the three cords, the plexus in this case report resembled the anatomy of a traditional plexus, except for the musculocutaneous nerve. The musculocutaneous nerve did not pierce the coracobrachialis muscle, instead giving off a branch to innervate the coracobrachialis muscle and traveling distally between the biceps and brachialis muscles.
Discussion
The brachial plexus is an intricate network of nerves usually formed from the ventral primary rami of the nerve roots C5-C8 and T1 and serves as an important landmark for clinical procedures [10]. Variations in the overall structure of the brachial plexus are not uncommon; however, variations at the roots and trunk level are rare [1]. In some cases, anomalies at the root and trunk levels occur without affecting the terminal branches, leading to asymptomatic anatomic variation. Asymptomatic anomalies can be discovered unexpectedly during clinical procedures, such as ultrasound guid ed nerve blocks, causing delays and challenges in patient management. Symptomatic brachial plexopathies are often diagnosed via electrophysiology or ultrasound and may present with an abrupt onset of painful, asymmetric, upper limb weakness with associated wasting of shoulder girdle and arm muscles [5,11]. These more severe symptoms can have debilitating consequences, therefore understanding potential variations in structure can facilitate better clinical decision making [12].
When describing the developmental role of the anomalous brachial plexus, Rao, et al. hypothesize that the embryological brachial plexus is a singular radicular cone within the upper limb bud. The plexus forms via the anastomosis of spinal nerves developing into a solid plate that later divides into separate trunks and divisions [13]. In a 2023 study by Nichols et al., the brachial plexus emerges from one axon extending from the spine into the arm bud. The anatomic obstacles that arise during concurrent embryological development, such as formation of blood vessels and cartilage, guide the development of the brachial plexus [14]. Variations of branching patterns may occur during this time because of anatomical spatial constraints. For instance, as the lateral cord is developing around veins, it may split to allow for the veins to form without interference [15]. This spatial limitation may be the cause of the increasing variability of brachial plexus anomalies in the more distal aspects of the plexus.
The current case describes the phenomenon of a non-union of C5 and C6 at the upper trunk of the brachial plexus. Our observations describe the inherent variability and potential deviations in the anatomical configuration that can present in the upper trunk in individuals, despite its rare occurrence. While there is abundant literature discussing the phenomenon of brachial trunk anomalies, there were a total of two studies reporting an anomaly of the superior trunk of the brachial plexus. Adam et al., described their findings of an “absent” superior trunk, with the provided photograph of the cadaver specimen appears almost identical to the findings of our donor cadaver [2]. From our observations, however, we argue that the upper trunk is not absent but instead lacks the union of C5 and C6 at the trunk level. We believe this better describes this anatomical variation, as an observed “absent” superior trunk would result in an anomalous or failed formation of the terminal branches. This theory derives from a study conducted by Singla et al., where upon dissection they discovered two trunks instead of three. The upper trunk was formed by the normal fusion of the C5 and the C6 roots [16]. However, the C7 root, instead of continuing as the middle trunk, joined with the roots of C8 and T1 to form a single trunk (which was termed the lower trunk in this case). The “absence” of the middle trunk led to downstream anomalous configurations of the cords coming off the trunks. Additionally, Fazan et al. reported a right sided variation of the superior trunk on two cadaveric plexuses. In both plexuses, it was noticed that the C5 and C6 roots were split into anterior and posterior divisions. The anterior divisions joined to give rise to an “anterior superior trunk” and the posterior divisions gave rise to a “posterior superior trunk” [17].
The presence of our upper trunk variation was rarely reported, with only one case report found discussing a similar variation. By investigating this phenomenon and exploring underlying mechanisms, researchers can gain insight into how the occurrence of brachial plexus anomalies arise as well as how to successfully approach them during surgical procedures. One such example is a case of a 71-year-old male who presented for a revision rotator cuff repair surgery. When evaluating the right supraclavicular fossa, it was observed that the brachial plexus divisions were anteromedial to the subclavian artery rather than posterolateral. This led the surgical team to place the brachial plexus catheter using a more proximal, instead of distal, interscalene approach, where the anatomical structure appeared normal, which provided adequate postoperative analgesia to the patient [4]. This case report serves to document an anomaly of the upper trunk with the purpose of furthering the importance of understanding the anatomical variations of the brachial plexus, particularly for surgeons performing procedures in the neck or shoulder region. Surgical interventions such as nerve sheath tumor resection or ultrasound guided nerve blocks may improve due to enhanced understanding or abnormal anatomy [18,19]. Moreover, clinical trials aimed to enhance anesthetic or surgical techniques will continue to form as we advance our knowledge of the brachial plexus and possible anomalies. Increasing the base of knowledge surrounding normal and abnormal brachial plexus anatomy has the potential to improve clinical outcomes, such as improved pain control, shorter hospitalization periods, and reduced systemic toxicity from errors during anesthetic injections [20]. The current case report is limited in scope due to the observations stemming from a single donor cadaver. Given that it was a post-mortem case report, there is no certainty regarding the effects of this anomaly for the patient. Further studies detailing these anomalies in live patients would be needed to establish definitive conclusions regarding the experienced effects, if any.
Conclusion
Variations in the brachial plexus are not a rare occurrence, but this paper highlights one such rare case involving the non-union of the ventral rami of nerve roots C5 and C6 at the upper trunk level. Understanding this anomaly can provide clinical significance during various medical procedures..
Informed Consent Statement
All donors contributing to the cadaver lab at The University of Toledo College of Medicine and Life Sciences have been required to complete documentation before donating their remains for educational purposes.
Data Availability Statement
The original contributions presented in the study are included in the article, further inquiries can be directed to the corresponding author/s.
Acknowledgement
The authors are thankful to all those involved in medical education at the University of Toledo, and specifically those who work in the gross anatomy lab. The work performed by these individuals is paramount to a robust medical education curriculum, and the les sons learned through gross dissection are difficult to obtain from any other medium.
Conflict of Interest
No Conflict of Interest.
References
- Emamhadi M, Chabok SY, Samini F, Alijani B, Behzadnia H, et al. (2016) Anatomical Variations of Brachial Plexus in Adult Cadavers; A Descriptive Study. Arch Bone Jt Surg 4(3): 253-258.
- Patel NT, Smith HF (2023) Clinically Relevant Anatomical Variations in the Brachial Plexus. Diagnostics (Basel) 13(5): 830.
- Gilcrease-Garcia BM, Deshmukh SD, Parsons MS (2020) Anatomy, Imaging, and Pathologic Conditions of the Brachial Plexus. Radiographics 40(6): 1686-1714.
- Porter SB, Garner HW, Schoch BS, Murray PM, Robards CB, et al. (2022) Anomalous Course of the Brachial Plexus Identified During Ultrasound-Guided Brachial Plexus Nerve Block. Turk J Anaesthesiol Reanim 50(4): 312-314.
- Khadilkar SV, Khade SS (2013) Brachial plexopathy. Ann Indian Acad Neurol 16(1): 12-18.
- Natsis K, Totlis T, Tsikaras P, Anastasopoulos N, Skandalakis P, et al. (2006) Variations of the course of the upper trunk of the brachial plexus and their clinical significance for the thoracic outlet syndrome: a study on 93 cadavers. Am Surg 72(2): 188-192.
- Yadav N, Saini N, Ayub A (2014) Anatomical variations of interscalene brachial plexus block: Do they really matter? Saudi J Anaesth 8(1): 142-143.
- Iwanaga J, Singh V, Ohtsuka A, Hwang Y, Kim HJ, et al. (2021) Acknowledging the use of human cadaveric tissues in research papers: Recommendations from anatomical journal editors. Clinical Anatomy 34(1): 2-4.
- Detton AJ, Tank PW (2017) Grant's dissector, Sixteenth edition ed.; Wolters Kluwer Philadelphia: Philadelphia.
- Adam A, Mohammed A, Grebballa A, Rizig S (2011) Absence of upper trunk of the brachial plexus. International journal of applied and basic medical research 1(2): 123-124.
- Chin KJ, Niazi A, Chan V (2008) Anomalous brachial plexus anatomy in the supraclavicular region detected by ultrasound. Anesth Analg 107(2): 729-731.
- Yildiz S, Cömert A, Ozan H (2011) A case of connected superior and middle trunks of the brachial plexus or with abnormal upper trunk. Rom J Morphol Embryol 52(3): 1157-1159.
- Prasada Rao PV, Chaudhary SC (2000) Communication of the musculocutaneous nerve with the median nerve. East Afr Med J 77(9): 498-503.
- Nichols AM, Patel DB, Geske NL, McMillan W (2023) A Case Report on Brachial Plexus Anomaly, Embryological Basis, and Clinical Implications. Cureus 15(11): e49504.
- Leijnse JN, de Bakker BS, D'Herde K (2020) The brachial plexus-explaining its morphology and variability by a generic developmental model. J Anat 236(5): 862-882.
- Singla R, Sharma RK, Shree B (2013) A Two Trunked Brachial Plexus: A Case Report. Journal of clinical and diagnostic research: JCDR 7(4): 704-705.
- Fazan V, Souza A, Adilson L C, Andrade R (2003) Brachial plexus variations in its formation and main branches. Acta Cirurgica Brasileira 18(5).
- Mian A, Chaudhry I, Huang R, Rizk E, Tubbs RS, et al. (2014) Brachial plexus anesthesia: A review of the relevant anatomy, complications, and anatomical variations. Clin Anat 27(2): 210-221.
- Gulam Anwer K, Shekhar KY, Khatiwoda S, Chetri R Cadaveric Study of Variation in the Formation of Trunks of Brachial Plexus, Embryological Basis and its Clinical Significance. International Archives of BioMedical and Clinical Research: 2(5).
- Neal JM, Gerancher JC, Hebl JR, Ilfeld BM, McCartney CJ, et al. (2009) Upper extremity regional anesthesia: essentials of our current understanding, 2008. Reg Anesth Pain Med 34(2): 134-170.
-
Dominique DiGiacomo, Paola Pedraza Cruz, Eric M Lassiter, Ambika Sood, Wendy Lackey-Cornelison and Adel Maklad*. Independent C5 And C6 Superior Trunks of The Brachial Plexus with An Anomalous Origin of The Pectoral Nerves. Arch Neurol & Neurosci. 16(4): 2024. ANN.MS.ID.000891.
-
Acute Polyradiculoneuritis, Neurology, Guillain-barre; Fann teaching hospital, neuropathy, cranial nerves, immunotherapy, Neuroscience, neurogenic syndrome, epidemiological, Dysphonia.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






