 Case Report
Case Report
Extensive Multilevel Spinal and Extraspinal Involvement in a Case of Calvarial Tuberculosis: A Rare Disseminated Presentation
Harsh Patel*, Preeti Singh and Abhaya Kumar
Kokilaben Dhirubhai Ambani Hospital and Research Institute, India
Harsh Patel , Kokilaben Dhirubhai Ambani Hospital and Research Institute, Mumbai, Maharashta ,India.
Received Date:May 23,2025; Published Date: May 30, 2025
Calvarial tuberculosis (TB) is an uncommon manifestation of skeletal TB, and its progression to disseminated involvement of multiple systems is exceedingly rare. We report a unique case of a patient initially diagnosed with calvarial TB, who subsequently developed widespread involvement of the cervical and lumbar spine, bilateral paraspinal soft tissues, the right psoas muscle, and pulmonary parenchyma. Imaging studies demonstrated intraosseous abscesses, soft tissue masses, and compressive epidural components, consistent with disseminated TB. The patient was advised to undergo fluid aspiration for microbiological confirmation and drug susceptibility testing, in view of possible drug-resistant TB. This case underscores the need for high clinical suspicion, early diagnosis, and systemic evaluation in patients with skeletal TB to identify and manage potentially disseminated disease.
Keywords:Calvarial tuberculosis; Disseminated TB; Spinal TB; Psoas abscess; Drug-resistant tuberculosis; Vertebral osteolysis
Introduction
Tuberculosis (TB) continues to pose a significant global health challenge, with extrapulmonary forms accounting for approximately 15–20% of all cases. Among these, skeletal TB is relatively uncommon and can present with diverse clinical manifestations depending on the site of involvement. Calvarial tuberculosis is particularly rare, comprising less than 1% of skeletal TB cases, and its dissemination to the spine or soft tissues is even more exceptional [1,2]. In this report, we present a unique case of disseminated TB initially manifesting as calvarial involvement, later progressing to include extensive vertebral, paravertebral, and pulmonary disease.
Case Presentation
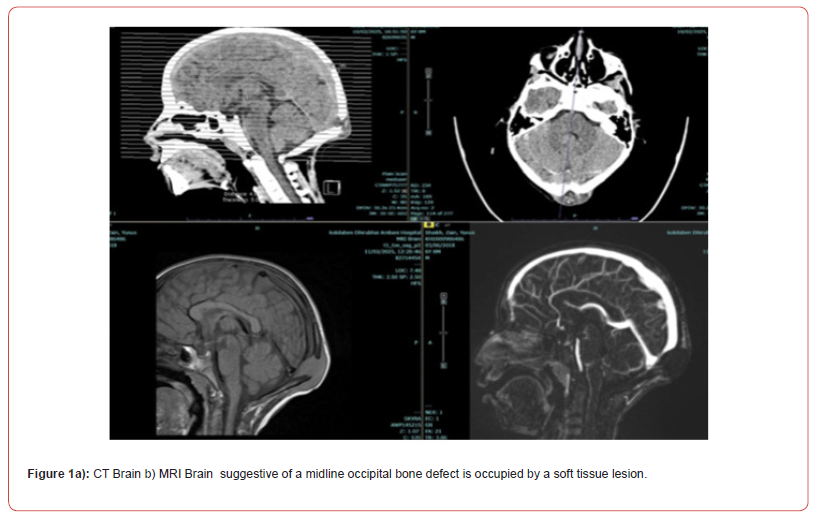
A 6-year-old child presented to the emergency department following a fall from a significant height, landing on the occipital region of the head. At the time of injury, the child was conscious and neurologically intact. A non-contrast computed tomography (CT) scan of the brain was performed, which did not reveal any acute intracranial abnormalities, skull fractures, or significant soft tissue injury. The child was managed conservatively and discharged with instructions for follow-up. Two weeks later, the patient was brought back with a gradually enlarging, non-tender swelling over the occipital region. The parents reported no fever, weight loss, or neurological symptoms, but noted that the swelling had progressively increased in size without signs of redness or warmth. On examination, the swelling was firm, fluctuant, and localized to the midline occipital region, without overlying skin changes or signs of infection. A repeat CT scan of the head, now with bone window settings, revealed a well-defined lytic lesion involving the midline occipital bone. The lesion caused cortical thinning and expansion, with a defect noted in the inner and outer tables of the skull. There was an associated soft tissue component extending extracranially, but no evidence of intracranial extension. Magnetic resonance imaging (MRI) was subsequently performed for further characterization. The lesion appeared hypointense on T1-weighted images and hyperintense on T2-weighted sequences, with no significant post-contrast enhancement. Based on the radiological features and the absence of systemic symptoms, an intradiploic epidermoid cyst was initially considered the most likely diagnosis (Figure 1a).
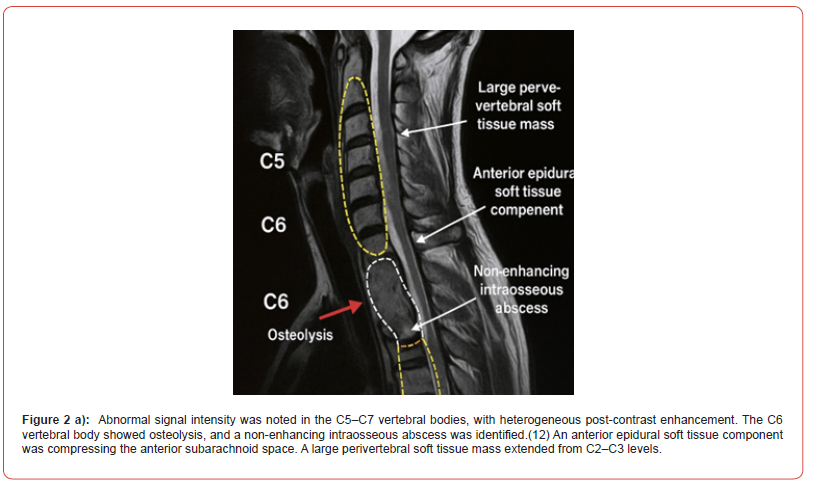
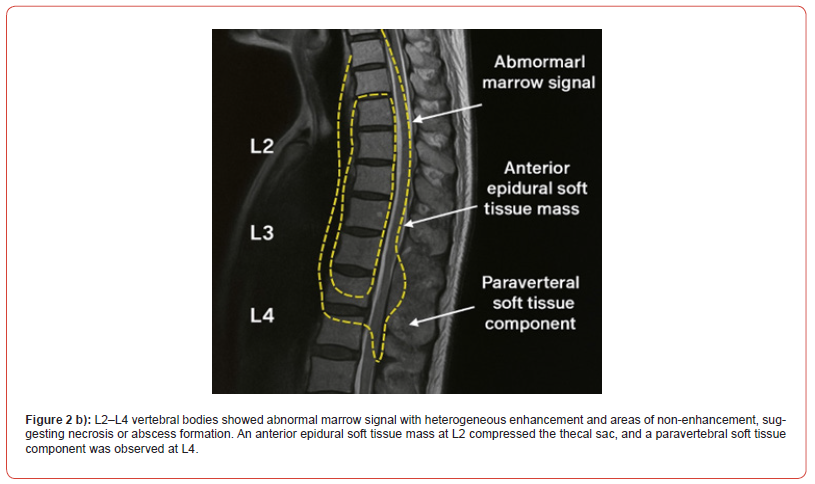
The patient subsequently underwent a suboccipital craniotomy for excision of the occipital lesion. Intraoperatively, a lytic bone defect was noted in the midline occipital bone, containing caseous material. The underlying dura appeared intact, and there was no communication with intracranial structures. The soft tissue mass was excised along with debridement of the affected bone.Histopathological examination of the excised tissue revealed granulomatous inflammation characterized by epithelioid cell granulomas with central caseation necrosis and Langhans-type giant cells, consistent with a diagnosis of tuberculous osteomyelitis of the calvarium. Ziehl-Neelsen staining confirmed the presence of acid-fast bacilli, establishing a definitive diagnosis of calvarial tuberculosis [10,11]. The patient was started on a standard four-drug antitubercular therapy (ATT) regimen, consisting of isoniazid, rifampicin, pyrazinamide, and ethambutol. A follow-up MRI of the brain and skull, performed one month postoperatively, demonstrated near-complete resolution of the extracranial and extradural soft tissue components, with no new lesions or recurrence at the surgical site.Despite the encouraging local response, the clinical team opted to perform a whole-spine MRI to assess for possible systemic dissemination, given the atypical presentation and potential for hematogenous spread in pediatric TB. Surprisingly, the spinal imaging revealed extensive abnormalities involving both the cervical and lumbar regions of the spine. These included: (Figure 2a and Figure 2b).
Additional findings included a large right psoas abscess and pulmonary involvement with cervical and mediastinal lymphadenopathy commonly seen in disseminated spinal TB(13). In view of the extensive spinal and paraspinal involvement noted on MRI, and considering the possibility of atypical progression despite first-line therapy, tuberculous drug resistance was suspected. Although the patient had shown partial local response at the calvarial site, the emergence of multifocal spinal lesions raised concern for multidrug- resistant tuberculosis (MDR-TB) or suboptimal drug penetration to extrapulmonary foci.
To further evaluate the microbial sensitivity profile, CT-guided aspiration of a paraspinal abscess was advised. Under sterile conditions and imaging guidance, purulent material was aspirated from one of the lumbar paraspinal collections and sent for GeneXpert MTB/RIF assay, line probe assay, mycobacterial culture, and drug susceptibility testing (DST).
The aspirated paraspinal fluid was positive for Mycobacterium tuberculosis on GeneXpert MTB/RIF assay, which also detected rifampicin resistance, suggesting a multidrug-resistant tuberculosis (MDR-TB) strain. This was later confirmed by line probe assay and conventional culture-based drug susceptibility testing (DST), which demonstrated resistance to both isoniazid and rifampicin, with sensitivity to fluoroquinolones and second-line injectable agents.
In light of these findings, the patient was diagnosed with disseminated
MDR-TB, involving the calvarium, cervical and lumbar
spine, and paraspinal soft tissues. Given the severity of the disease
and the patient’s age, a tailored second-line antitubercular therapy
regimen was initiated in accordance with World Health Organization
(WHO) guidelines for pediatric MDR-TB [14]. The regimen included:
• Levofloxacin (fluoroquinolone)
• Amikacin (aminoglycoside)
• Ethionamide
• Cycloserine
• Pyrazinamide (continued as it remained sensitive)
• Linezolid, added for its CNS penetration and efficacy in
complicated MDR-TB cases
The patient was also started on vitamin B6 (pyridoxine) supplementation to mitigate neurotoxicity associated with cycloserine and linezolid. Close monitoring was instituted for potential drug-related side effects, particularly ototoxicity from amikacin and hematologic suppression from linezolid.A multidisciplinary team comprising pediatric infectious disease specialists, neurologists, and neurosurgeons was involved in the ongoing management. The decision was made to continue conservative management of the spinal lesions as there were no signs of neurological impairment or spinal instability. Serial imaging was planned to monitor the therapeutic response.This case illustrates the critical role of early microbiologic confirmation in atypical TB presentations, particularly in pediatric patients with unusual or rapidly progressive disease patterns. Timely identification of drug resistance allowed for prompt modification of therapy, potentially averting severe complications such as spinal cord compression or systemic dissemination.
Discussion
This case illustrates a rare and aggressive form of disseminated TB that initially presented as localized calvarial tuberculosis. Calvarial TB is a rare entity, accounting for 0.2–1.3% of skeletal TB (4,5). It commonly presents with scalp swelling and punched-out bone defects on imaging (1,2,3,6). MRI plays a crucial role in evaluating extent and complications (8).
Dissemination to multiple spinal levels and extraspinal sites such as the psoas muscle and lungs is exceedingly rare (7,9). Spinal TB usually affects contiguous vertebral segments, and extensive multi-regional involvement—as seen in this case—is atypical (8,9). The presence of a large psoas abscess, epidural extension, and lung involvement raises suspicion of drug-resistant TB or hematogenous spread from a primary pulmonary focus (7). The need for early microbiological confirmation, culture, and drug susceptibility testing is emphasized to guide targeted therapy (9). This case also highlights the importance of considering tuberculosis in differential diagnosis of unusual scalp swellings and skull lesions, especially in endemic regions (6,7).
Conclusion
This case highlights the critical need for a high index of suspicion and comprehensive systemic evaluation in cases of skeletal tuberculosis, especially when initial lesions are detected in uncommon sites such as the calvarium. Calvarial tuberculosis is an exceedingly rare manifestation, often misdiagnosed due to its nonspecific presentation and radiologic resemblance to other benign lesions, such as epidermoid cysts or Langerhans cell histiocytosis. Our patient’s progression from an isolated calvarial lesion to widespread vertebral, paraspinal, and pulmonary involvement illustrates the potential for hematogenous dissemination and the multifocal nature of extrapulmonary TB, particularly in pediatric populations. This underscores the importance of whole-body imaging, including spinal MRI, in the workup of skeletal TB—even when the primary lesion appears localized. Most crucially, this case demonstrates the necessity of early microbiological confirmation, including GeneXpert MTB/RIF testing and full drug susceptibility profiling, in any patient with progressive or multifocal TB, to detect drug-resistant strains. Early detection of MDR-TB allowed for timely initiation of second-line therapy, likely preventing severe complications such as spinal cord compression, neurological deficits, or deformity. Multidisciplinary collaboration and adherence to WHO guidelines for MDR-TB management are essential for optimizing outcomes in such complex cases. Clinicians should remain vigilant for atypical presentations of TB and initiate prompt, individualized therapy based on microbiologic data to reduce morbidity and improve prognosis.
Declaration
a. Funding The authors did not receive support from any organization
for the submitted work.
b. Conflicts of interest/Competing interests (include appropriate
disclosures) The authors have no conflicts of interest to
declare that are relevant to the content of this article
c. Ethics approval and consent to participate The study is
approved by institutional ethics committee (IEC). Written consent
has been taken from the participant parent to publish the
study.
d. Availability of data and material : not applicable
e. Consent for publication All authors have reviewed and approved
the final version of the manuscript
f. Authors’ contributions Dr Harsh : conceived and designed
the study Dr Preeti : contributed to the data analysis and wrote
the manuscript Dr Abhaya Kumar : provided critical feedback
and revised the manuscript
g. Acknowledgement : We acknowledge our department of
neurosurgery.
References
- Ramdurg SR, Gupta DK, Suri A, et al. (2010) Calvarial tuberculosis: uncommon manifestation of common disease—a series of 21 cases. Br J Neurosurg 24(5): 572–577.
- Diyora B, Kumar R, Modgi R, et al. (2009) Calvarial tuberculosis: a report of eleven patients. Neurol India 57(5): 607.
- Barton CJ (196) Tuberculosis of the vault of the skull. Br J Radiol 34(401): 286–290.
- Mukherjee KK, Kaushik R, Nada R, et al. (2002) Calvarial tuberculosis. Surg Neurol 57(3): 195–202.
- (2024) Calvarial tuberculosis in patient with cervical tuberculous lymphadenitis: a case report. Cureus.
- (2020) Skull base and calvarial tuberculosis: a rare presentation. Clin Radiol. Available at: https://www.sciencedirect.com/science/article/pii/S0019570720300111
- (2019) Calvarial tuberculosis: an unusual presentation. BMJ Case Rep 12(4):e226967.
- MRI findings in spinal tuberculosis. Orthobullets. Available at: https://www.orthobullets.com/spine/2027/spinal-tuberculosis
- (2020) Atypical spinal tuberculosis: a case report. Exp Ther Med 20(6):163.
- Turgut M (2001) Spinal tuberculosis (Pott’s disease): its clinical presentation, surgical management, and outcome. A survey study on 694 patients. Neurosurg Rev 24(1):8–13.
- Bernaerts A, Vanhoenacker FM, Parizel PM, et al. (2003) Tuberculosis of the central nervous system: overview of neuroradiological findings. Eur Radiol 13(8): 1876–90.
- Jain A (2010) Tuberculosis of the spine: a fresh look at an old disease. J Bone Joint Surg Br 92(7): 905–13
- Garg RK, Somvanshi DS (2011) Spinal tuberculosis: a review. J Spinal Cord Med 34(5): 440–54.
- World Health Organization (2020) WHO consolidated guidelines on drug-resistant tuberculosis treatment. Geneva: WHO. [Available at: https://www.who.int/publications/i/item/9789240007048]
-
Harsh Patel*, Preeti Singh and Abhaya Kumar.Extensive Multilevel Spinal and Extraspinal Involvement in a Case of Calvarial Tuberculosis: A Rare Disseminated Presentation. Arch Neurol & Neurosci. 17(5): 2025. ANN.MS.ID.000922.
-
Dolichoectasia, Mental Impairment, Hearing Loss, Nevocellular Nevi, Flat Noses, Hypopigmentation, Dolichoectasia, Seizures.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






