 Medical Case Report
Medical Case Report
Episodic Hypothermia Related to Autonomic Dysfunction Improved on Cyproheptadine and Pyridostigmine
Leilani Janay Miranda1,2* and Anna DePold Hohler1
1Department of Neurology, St. Elizabeth’s Medical Center, Brighton, MA, United States
2Tufts School of Medicine, Boston, MA, United Staates
Leilani Janay Miranda, Department of Neurology, St. Elizabeths Medical Center 736 Cambridge Street, CCP8, Brighton, MA 02135, United States.
Received Date:December 12, 2023; Published Date:December 19, 2023
Abstract
Hypothermia is quantified by a basal core temperature that is below 35ºC and can have a variety of causes, most of which are self-limited or resolve when the underlying cause is treated. Some patients may exhibit episodic hypothermia. There are several reports of cyproheptadine being beneficial in the treatment of episodic hypothermia in children and young adults. This case report discusses a 62-year-old woman with underlying autonomic dysfunction who had multiple episodes of neuropathic pain, hypothermia and diaphoresis, all of which responded to cyproheptadine and pyridostigmine treatment. In this patient, the hypothermia was attributed to her autonomic system dysfunction..
Keywords:Autonomic dysfunction; Hypothermia; Cyproheptadine; Pyridostimine; Case Report
Introduction
Hypothermia is quantified by a basal core temperature that is below 35ºC and is often self limited once the underlying cause is treated. Some patients have episodic hypothermia. A variety of causes can lead to this type of thermoregulatory dysfunction such as injury or destruction of the hypothalamus, agenesis of the corpus callosum (Shapiro’s syndrome), multiple sclerosis, or other autonomic dysfunction [1,2]. Patients who experience episodic hypothermia can have physical and cognitive manifestations during an episode. Some of these symptoms can severely hinder a patient’s ability to continue with their activities of daily living. Temperature regulation is maintained by a hippocampal circuit including ventrolateral preoptic GABAergic neurons, and the neural activity of dorsomedial neurons leading to reflexive response temperature dysregulation [3]. Activation of GABAergic vLPO neurons reduce body temperature [3].
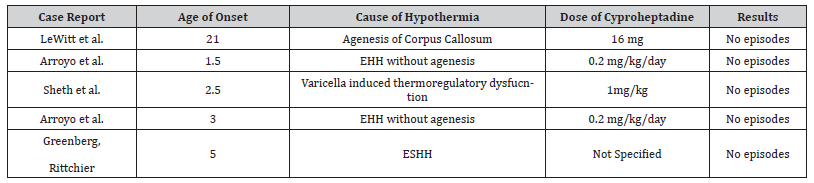
This case report reviews a patient diagnosed with autonomic dysfunction, which contributed to her recurrent episodic hypothermia. This patient responded well to treatment with cyproheptadine and pyridostigmine with improvement of her hypothermia [4]. Reports have indicated that cyproheptadine may be beneficial in the treatment of episodic hypothermia in children and adults summarized in Table 1 [2,5]. Pyridostigmine at a dose of 30 mg twice a day has been reported to optimize thermoregulatory regulation by minimizing the suspectibility to hypothermia, and by maintaining basal body temperature via a peripheral cholinergic mechanism [6]. Pyridostigmine can be used on a long-term basis safely in patients with neurological conditions [7]. Pyridostigmine displays the abilituy to suppress the activation of GABAergic postsynaptic currents, thus possibly affecting the hypothalmus’ role in lowering body temperature [8]. Cyproheptadine appears to affect the hypothamic 5HT2A receptors linked with thermoregulation [9]. There have been no reports of the concomitant treatment of pyridostigmine and cyproheptadine for hypothermia.
Table 1:Reported Treatment of Episodic Hypothermia with Cyproheptadine.
Case Presentation
A 62 year-old woman with a history of degenerative disc disease, arthritis, neuropathic pain, and a nonruptured 4 mm left M2 aneurysm who presented to the neurology clinic with a reported history of hypertensive crises, lightheadedness with position changes, and a feeling of being cold. The patient’s hypothermic episodes usually began in the evenings, lasted through the night, and she would wake in the early morning hours shivering. These episodes could last between 8 and 12 hours. During the hypothermic episodes the patient reported an experience of “unawareness” of her body. EEG testing was negative for seizures. The patient’s self temperature monitoring on a standard oral thermometer revealed a temperature that was often below 98 degrees F (36.67 degrees C). She frequently reported temperatures of 96 degrees F (35.56 degrees C) and occasionally as low as 94 degrees F (34.44 degrees C) temperarature changes summarized in Table 2. Triggers to the hypothermic episodes included stress and infection. The patient also had difficulties with orthostatic hypotension (drop of SBP >20 when changing positions) with her systolic blood pressure dropping below 100 mmHg when she stood up. Tilt table testing provided no evidence of predispoisiton to neurally mediated syncope or exaggerated postural tachycardia, however tilt testing revealed measure of parasympathetic and sympathetic adrenergic function is abnormal, with normal sympathetic cholinergic function. Her neurological exam revealed normal cognitive testing, cranial nerve function, motor strength, reflexes, coordination and gait. Her sensory exam revealed a small fiber neuropathy; sensory polyneuropathy with a stocking/glove deficit in pinprick sensation. The results of a skin biopsy of PGP9.6 immunolabeled sections showed severe distal small fiber neuropathy with reduction of epidermal innervation with the retention of the dermal and dermal gland innervation. Morphemetric quantitation of epidermal nerve ending yielded epidermal neutirte density of 14 neurites/mm2 skin,. This is below the 5th percentile threshold resulting in a diagnosis of small fiber neuropathy. Diabetes mellitus was ruled out due to the lack of supporting lab results. The diagnosis of multiple system atrophy was also excluded due to a lack of parkinsonism features, cerebellar ataxia and lack of significant imaging such as atrophy of the putamen pons or cerebellum, and no indication of MSA on TILT table testing. An MRI of the brain did not reveal any structural issues and a full endocrine panel including T3,T4, ferritin, B12 and Vitamin D were normal. An EMG ruled out large-fiber peripheral neuropathy. There was no infectious or pharmacological causes identified for the autonomic insuffiency.
Table 2:Total Daily Dose of Cyproheptadine and Pyridostigmine with Self Reported Temperature data in F.
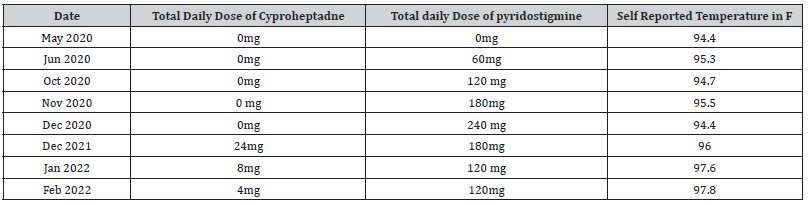
Her orthostatic hypotension improved with pyridostigmine treatment starting at 30mg PO BID and titrating it up to effect. Her hypothermia improved further with the addition of the pyridostigmine. The patient developed gastrointestinal side effects on the pyridostigmine. Once her orthostatic hypotension stabilized, the pyridostigmine was lowered slightly to reduce gastrointestinal side effects. She was maintained at a low level of 30mg twice daily. Cyproheptadine was started for hypothermia with some improvement.
Gradually, the dose of cyproheptadine was increased to 8mg three times a day. On this regimen, the patient had a reduction in the number and intensity of episodes. They decreased from daily episodes to an episode once every few weeks. She did experience some side effects of cognitive slowing 3 months following the in crease of the cyproheptadine dosage. Repeat cognitive testing and MRI of the brain to rule out central causes of hypothermia, provided normal results. Cyproheptadine was gradually tapered without return of her severe hypothermia episodes with the maintenance dose of pyridostigmine. She subsequently moved to a warmer climate that allowed the complete resolution of the hypothermia.
Discussion
This case report discusses a patient with autonomic dysfunction with autonomic neuropathy including hypothermia who had reduction in the severity and frequency of hypothermic episodes on a combination of pyridostigmine and cyproheptadine. Hypothermia can be due to a variety of causes that can include metabolic derangements, neurotransmitter disorders, or brain lesions to the hypothalamus due to tumors, multiple sclerosis, or trauma [10]. The mechanism of temperature regulation is due to a combination of neuroregulatory signals that maintain the reflexes designated to regulate temperature. The most common cause of episodic hypothermia is related to medication side effects. Hypothermia has sometimes been observed with agenesis of the corpus callosum (Shapiro’s syndrome).
The most common treatment for episodic hypothermia is dependent on the cause. Medications that have been reported to helpin the treatment of episodic hypothermia include clonidine, clomipramine and cyproheptadine [11]. To our knowledge, this is the first case reported with concomitant use of pyridostigmine and cyproheptadine with beneficial effects for episodic hypothermia. Cyproheptadine acts at a serotonin 2A and histamine receptor antagonist, thus may be useful in reglualting temperature modulation via the regulation of the neurotransmitters responsible for temperature modulation. Pyridostigmine may be combined with cyproheptadine in the management of autonomic patients with thermoregulatory dysfunction to optimize recovery (Table 1 & 2).
Statement of Ethics
This study protocol was reviewed and determined to be exempt by the St. Elizabeth’s Medical Center IRB, on February 15th, 2022. Written informed consent was obtained from the patient for publication of the details of their medical case and any accompanying images.
Conflict of Interest
The authors have no conflict of interest to declare.
Funding Sources
Department of Neurology
Author Contributions
Conceptualization: A.H; Writing of manuscript: L.M; Data Collection: L.M, A.H; Formal Analysis: L.M; Review and Editing: A.H,.
Data Availabiltiy
Details are found in the patient’s medical record and on no other publicly accessible website. All data generated or analyzed during the study are included in the article. Further enquiries can be directed to the corresponding author.
References
- Blondin NA (2014) Diagnosis and management of periodic hypothermia. Neurol Clin Pract 4(1): 26-33.
- LeWitt PA, Newman RP, Greenberg HS, Rocher LL, Calne DB, et al. (1983) Episodic hyperhidrosis, hypothermia, and agenesis of corpus callosum. Neurology 33(9): 1122-1129.
- Zhao ZD, Yang WZ, Gao C, Xin Fu, Wen Zhang, et al. (2017) A hypothalamic circuit that controls body temperature. Proceedings of the National Academy of Sciences 114(8): 2042-2047.
- Matthew CB, Glenn JF, Bowers WD Jr, Navara DK (1994) Cholinergic drug interactions and heat tolerance. Life Sci 54(17): 1237-1245.
- Rowsey PJ, Yang YL, Gordon CJ (2002) Peripheral cholinergic pathway modulates hyperthermia induced by stress in rats exposed to open-field stress. Journal of Applied Physiology 92(2): 789-794.
- Hugo A, A. Di Blasi M, Grinszpan GJ (1990) A syndrome of hyperhidrosis, hypothermia, and bradycardia possibly due to central monoaminergic dysfunction. Neurology 40(3 Part 1): 556-557.
- Maggi L, Mantegazza R (2011) Treatment of myasthenia gravis: focus on pyridostigmine. Clin Drug Investig 31(10): 691-701.
- Santos MD, Pereira EFR, Aracava Y, Newton G Castro, William P Fawcett, et al. (2003) Low concentrations of pyridostigmine prevent soman-induced inhibition of GABAergic transmission in the central nervous system: involvement of muscarinic receptors. J Pharmacol Exp Ther 304(1): 254-265.
- Won SJ, Lin MT (1988) 5-Hydroxytryptamine receptors in the hypothalamus mediate thermoregulatory responses in rabbits. Naunyn Schmiedebergs Arch Pharmacol 338(3): 256-261.
- Sheth RD, Barron TF, Hartlage PL (1994) Episodic spontaneous hypothermia with hyperhidrosis: implications for pathogenesis. Pediatr Neurol 10(1): 58-60.
- Greenberg RA, Rittichier KK (2003) Pediatric nonenvironmental hypothermia presenting to the emergency department: Episodic spontaneous hypothermia with hyperhidrosis. Pediatr Emerg Care 19(1): 32-34.
-
Leilani Janay Miranda* and Anna DePold Hohler. Episodic Hypothermia Related to Autonomic Dysfunction Improved on Cyproheptadine and Pyridostigmine. Arch Neurol & Neurosci. 16(2): 2023. ANN.MS.ID.000885.
-
Acute Polyradiculoneuritis, Neurology, Guillain-barre; Fann teaching hospital, neuropathy, cranial nerves, immunotherapy, Neuroscience, neurogenic syndrome, epidemiological, Dysphonia.
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






