 Case Report
Case Report
Cerebrovascular Accident as a First Manifestation of Neuropsychiatric Systemic Lupus Erythematosus; a Comprehensive Review; a Case Report
Saeed Shahbeigi1* and Mojdeh Bolouchian2
1Department of Neurology, Shahid Beheshti Medical University Research Center, Iran
2Department of Medical Sciences, Islamic Azad University, Iran
Dr. Saeed Shahbeigi, Shahid Beheshti Medical University, Tehran, Iran.
Received Date: March 15,2022; Published Date:August 09, 2022
Systemic lupus erythematosus (SLE) is an autoimmune connective-tissue disease that mostly affects women of childbearing age. One of the important symptoms of lupus erythematosus is neuropsychiatric (NP) manifestations that mostly present with neurologic syndromes as well as confusion, lethargy, mood changes, and even psychosis. The case presented in this article is a 38-year-old woman who had progressive left side hemiparesis and cognitive dysfunction. According to the brain MRI and further examinations, she had a cerebrovascular accident (CVA) along with Systemic lupus erythematosus. Due to the definite SLE, the positivity of antiphospholipid antibodies, and the occurrence of CVA, the patient was diagnosed as definite neuropsychiatric systemic lupus erythematosus (NPSLE). NPSLE is a general explanation mentioning a series of neurological and psychiatric features directly related to systemic lupus erythematosus. Due to the scarcity of clinical trials in NPSLE, we obtain most of the data from case series and case reports. Two different mechanisms are recognized to associate to NPSLE: (1) Inflammatory and autoimmune-mediated events (2) Thrombotic and ischemic associated with microangiopathy, and hemorrhage. In the acute phase, management of patients with NPSLE diagnosis does not vary from other non-SLE neurologic subjects which present with the neurological manifestation. High-dose glucocorticoids and intravenous cyclophosphamide or even rituximab are used in patients with inflammatory and autoimmune pathophysiology. Anticoagulation and antiplatelet agents are used in treatment when the patient has vascular thrombosis. Antimalarial medications such as hydroxychloroquine may play a protective role against the worsening of brain lesions. This article supplies a comprehensive review of the literature on the pathophysiology, epidemiology, diagnostic approach, and management of NPSLE. We also explain the most common pharmacological treatments for NPSLE, based on a search of articles as well as a complete mention of an NPSLE case report.
Keywords:Cerebrovascular accident; Neuropsychiatric systemic lupus erythematosus; SLE; NPSLE
Abbreviations:NPSLE: Neuropsychiatric Systemic Lupus Erythematosus; SLE: Systemic Lupus Erythematosus; CVA: Cerebrovascular Accident; NP: Neuropsychiatric; MRI Magnetic Resonance Imaging; MRA: Magnetic Resonance Angiography; MRS: Magnetic Resonance Spectroscopy; APS: Antiphospholipid Syndrome; SS: Sjogren’s Syndrome; aPLs: Antiphospholipid antibodies
Case Report
The patient was a 38-year-old woman who had the left side hemiparesis and agitation with upper 2/5 and lower extremities 3/5. She had the left side central facial paresis as well. She was admitted at the hospital on April 2020 and Para-clinical procedures including laboratory tests, MRI, MRA and MRS was performed for her. The Brain MRI showed a large hyper signal lesion at the right basal ganglia with multiple high signal lesions in the subcortical portion of both frontotemporal lobes, ischemic changes in the both hemisphere and also infarction in the right temporal lobe and right basal ganglia (Figure 1-2). Brain MRS showed no evidence of malignancy (Figure 4); However, brain MRA showed narrowing in the right MCA (Figure 3). On the EEG she had normal findings. Eventually she had cerebrovascular accident (CVA) so she was admitted at the ICU. After checking the laboratory data (Table 1) in order to the positivity of the ANA test, we suspected SLE, hence based on the new diagnostic SLE criteria (EULAR/ACR), definite SLE was confirmed (+ ANA, +Anti- dsDNA 6+, +anti-phospholipid antibodies +2, thrombocytopenia 2+, autoimmune hemolytic anemia +4, proteinuria +4; totally more than 10 scores) (Table 2). Due to the definite SLE, the positivity of anti-phospholipid antibodies and the occurrence of CVA, the patient was diagnosed as definite NPSLE (Figure 6). In addition, 12 weeks later, the antiphospholipid antibodies were checked, which was positive again, so the definitive diagnosis of antiphospholipid syndrome (APS) was also confirmed [1]. Treatment approach varies depending on the mechanism of the disease. In this patient, in order to the ischemic type of NPSLE and the presence of antiphospholipid antibody syndrome, aspirin 100 mg and clopidogrel 75 mg were administered. In addition, prednisolone 10mg, atorvastatin 40 mg and hydroxychloroquine 400 mg daily were added to the treatment (Figure 1-4, Table 1).
Table 1:This table shows the patient’s serological tests.

Table 2:criteria for diagnosis of SLE.
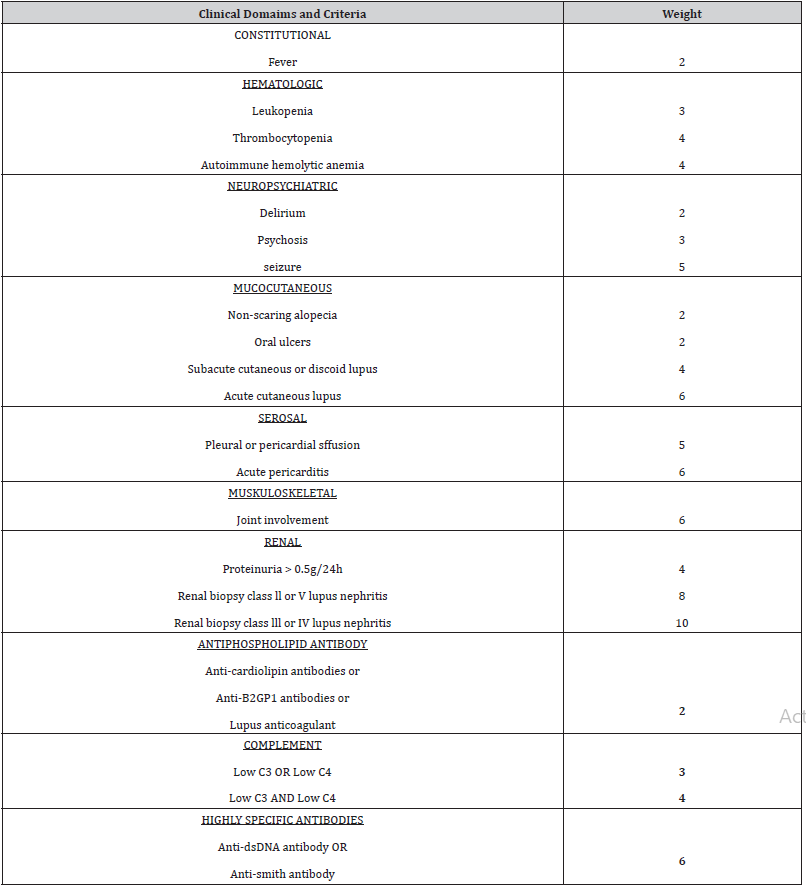
Figure 1:Brain MRI which shows a large hyper signal lesion at the right side.
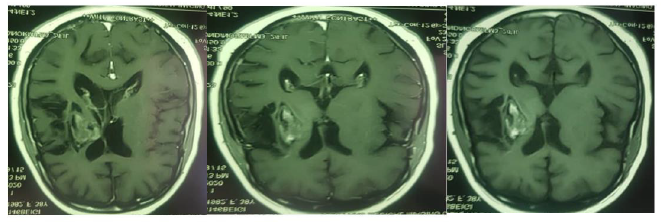
Figure 2:Brain MRI that reveals ischemic change in the both hemispheres, and also previous hemorrhagic infarction in the right temporal lobe and right basal ganglia due to SLE.

Figure 3:Brain MRA shows narrowing in the right MCA.
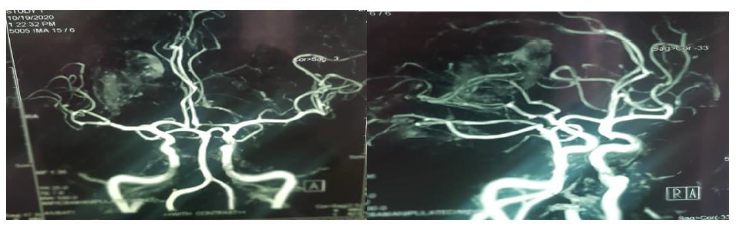
Figure 4:Brain MRS shows no evidence of malignancy.

Introduction
Systemic lupus erythematosus (SLE) is an autoimmune connective-tissue disorder that primarily involved skin and mainly affecting females manifested as multisystem organ involvement in which the body’s immune system attacks its ownself [2]. Neuropsychiatric manifestation of SLE happened in a high percentage of SLE cases [3]. Diagnostic methods for NPSLE, such as laboratory or radiological methods are very limited and non-specific, therefore diagnosis and treatment management is problematic. In clinical practice, a particular multidisciplinary diagnostic and therapeutic technique based on the suspected goal and severity of symptoms is recommended [4]. The total prevalence approximations of NPSLE differs from 14% to 75% of all SLE patients [5]. In SLE cohorts, the incidence of NPSLE has been mentioned to happen at disease-onset in 6-40% of SLE. SLE patients can manifest one single neuropsychiatric (NP) features, however about 17-60 % show at least a second event during their disease progression [3]. This article provides a comprehensive review of the literature on the pathophysiology, classification, diagnosis and management of NPSLE, and explain the most common pharmacological therapies for NPSLE patients.
Approach to diagnosis of SLE
The ACR and EULAR working group in 2017 met to reassessed the criteria for SLE that were used for the prior 35 years. According on the Table 2, When total score is 10 or more, it is classified as Systemic Lupus Erythematosus if entry criterion fulfilled (Table 2). To enter the SLE diagnostic criteria, the ANA titer must be greater than or equal to 1/80 on Hep2 cells; (these cells are used for detection of ANA titer). If a patient develops neuropsychiatric domain consists of delirium OR psychosis OR seizure, we have to consider SLE, when he or she has positive ANA. So as the second step, we have to check the other criteria of SLE (Table 2). If the patient reaches to score 10 or more, the patient was diagnosed as definite SLE [6-8] (Table 2).
According to the new criteria of SLE, in fact our patient was diagnosed as SLE; (+ ANA, + Anti- dsDNA 6+, + APLs +2, thrombocytopenia 2+, autoimmune hemolytic anemia 4+, proteinuria +4, totally more than 10 scores).
NPSLE diagnostic criteria
According to the American College of Rheumatology, NPSLE
syndrome’s manifestations are divided into two groups:
A: Central nervous system manifestations (include 12 items).
B: Peripheral nervous system manifestations (include 7 items)
[9,10].
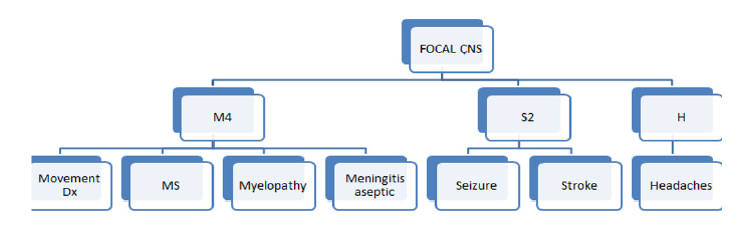
The central nervous system manifestations are also divided into two subdivisions: focal and diffuse symptoms. In the focal symptoms we are encountered with brain Stroke (CVA), demyelinating diseases (MS), Movement diseases including chorea and other types of movements disorders, aseptic Meningitis, Myelopathy, Seizure and Headaches (Figure 1) [9, 11]. For easy memorizing of focal manifestations of NPSLE, we have suggested the following diagram; including 4 M (synonyms for MS, Movement disorder, Myelopathy and Meningitis aseptic), 2S (Stroke and Seizure), and one H (headaches) (Figure 5).
Figure 5:Focal CNS manifestations of NPSLE
In the diffuse symptoms we pose with acute confusional state, anxiety disorder, cognitive disorder, mood disorder and psychosis. In terms of peripheral nervous system manifestations, we can see Guillain Barre, autonomic disorder, myasthenia gravis and other types of neuropathies (Figure 6) [12].
Figure 6:Neuropsychiatric syndromes according to the American College of Rheumatology

As it clear, anxiety, mood and cognitive disorders and headaches are nonspecific[13].In addition, other important and inclusive CNS manifestations, such as neuromyelitis optica or posterior reversible encephalopathy syndrome (PRES) that not mentioned in the ACR criteria, have been increasingly recognized to be linked to SLE [12, 14-16].
It is important to note that NPSLE could be classified according
on the underlying pathologic events. Two different mechanisms are
recognized to associate to NPSLE:
(1) Inflammatory and autoimmune-mediated events
(2) Thrombotic and ischemic associated with microangiopathy,
and hemorrhage [17].
In a considerable proportion of NPSLE patients, both pathophysiologic changes have been reported to coexist and to manifest as a wide heterogeneous group of NP features [18] (Figure 6).
Based on the findings of various studies, we have suggested the
diagnostic criteria for NPSLE which is as follows:
1-Firstly, the diagnosis of lupus erythematosus must be
confirmed based on ACR/EULAR 2019 criteria for diagnosis of SLE
[6].
2-Secondly, there should be at least one of those 19
neuropsychiatric manifestations. (Figure 6)
If a patient has both items, it is known as suspected NPSLE. To
confirm the diagnosis, the patient must have one of the followings:
-Positivity of at least one of the autoantibodies: antiphospholipid
(APL), anti-ribosomal-p, anti-neuronal, anti-ganglioside 1(GM1)
and anti-Ro-Thromboembolism (including stroke).
If a suspected NPSLE patient has one of the two items mentioned above, it is known as definite NPSLE (Figure 7) [14, 15, 19].
Anti-SSA/Ro antibodies are commonly existing among several autoimmune diseases, such as SLE and Sjogren’s Syndrome (SS). However, anti-SSB/La antibodies are normally existing in patients with SS and if they are found among patients with other autoimmune diseases, anti-SSB/La antibodies are always detected with anti-SSA/Ro antibodies simultaneously. Some researches link the existence of anti-SSA/Ro but not anti-SSB/La antibodies with the progression of NPSLE [20,21] (Figures 7).
Figure 7:NPSLE diagnostic criteria.

Therapeutic Strategies
Best treatment strategy for treating the NP symptoms of SLE, depending on the type and severity of the symptoms, should be started after the other causes have been ruled out [22]. According to the European League against Rheumatism (EULAR) theory, for the management of NPSLE, the general approach to treatment is no different from other non-SLE individuals presenting with the same NP manifestation. Non-pharmacological interventions and symptomatic therapy can also be used in the treatment process [13]. Some therapies (e.g. hydroxychloroquine) can be used in the primary prevention of major NPSLE, especially cerebrovascular disease [23]. Antimalarial drugs prevent recurrence and worsening of nervous system involvement such as seizures (except headaches) and also have a protective role [24]. Signs that are supposed to reveal an immune-inflammatory event or, in the presence of generalized lupus activity, starting of immunosuppressive treatment is warranted (corticosteroids alone or with another immunosuppressant), with the major objective of resolving/ stabilizing features [25]. For secondary prevention after ischemic lupus, especially in the presence of aPL antibodies anticoagulation and antiplatelet agents are used. immunosuppressive and anticoagulation and/or antiplatelet therapy should be considered when both ischemic and inflammatory NPSLE syndromes coexist [25,26]. Although the treatment of NPSLE patients varies from person to person depending on the symptoms and severity, in general for NPSLE patients, the treatment algorithm is based on available evidence and experience (Figure 8) [27].
Figure 8:Approach to treatment of NPSLE.

Symptomatic Therapy
In SLE cases with mood disorders, movement disorders, seizure
disorders, psychosis and headaches, regardless of the fact that these
are caused by SLE, the current drugs which is used to treat these
symptoms, are utilized as the first step. In mild NP features, this
symptomatic therapy can be adequate; however, in severe cases or
if there is no response to symptomatic therapy, additional treatment
with immunosuppressive and/or antithrombotic medication is
needed [13]. Antidepressive and antipsychotic medications, as well
as anxiolytics, are recommended based on the standard indications
in psychiatric disorders [26].
Non-pharmacological Intervention
Cognitive dysfunction which is usually mild, is common in
patients with SLE. Most studies have reported prevalence ranging
from 17 to 66 % and immunosuppressive has no indication in
its treatment [26]. Cognitive impairment has been accompanied
by psychosocial features such as pain, sleep deprivation, fatigue,
depression, and anxiety. There is no definite symptomatic therapy
for cognitive dysfunction in SLE. It has been observed that some SLE
patients who has depression with cognitive dysfunction may take
advantage of antidepressants [27]. In SLE patients with cognitive
dysfunction whose neuropsychological tests were not completely
impaired, the positive impact of an 8-week psychoeducational
group intervention was reported to improve memory self-efficacy,
memory function, and the ability to accomplish daily activities [27-
29].
A practical approach to treatment of NPSLE is as follows:
1. Firstly, SLE must be confirmed according to the ACR/
EULAR 2019 diagnostic criteria. After definitive confirmation
of SLE, the patients need an optimal control of cerebrovascular
risk factors. In this way, if the patients smoke, they should
quit and should be prescribed hydroxychloroquine, and in the
presence of LAC or isolated persistent medium-high titers of
acl, they should be prescribed ASA 100 mg/d.
2. If the NPSLE is confirmed, it should be determined
whether the patient is in the ischemic or inflammatory NPSLE
group, depending on the type of neuropsychiatric symptoms. If
it is in the inflammatory group, the treatment approach varies
depending on whether the symptoms are mild or severe.
If the patient’s symptoms are mild, symptomatic therapy is usually sufficient, or low doses of glucocorticoids (<0.5mg/kg/day) with or without azathioprine (2mg/kg) may be used, depending on the patient’s condition. After 3-6 months the patient should be reevaluated.
If the patient’s symptoms are severe, high doses of corticosteroid (pulses of methylprednisolone 1g/day IV for 3 days) and monthly IV cyclophosphamide for six months (0.5-1 g/m2) are prescribed and the patient needs to be re-evaluated after six months.
If the patients respond completely to the treatment, they will be given maintenance therapy for one year, which will be selected according to the patient’s conditions from the following: Azathioprine 2mg/kg/d, mycophenolate 3g/d, cyclosporine 500 mg/d and prednisone.
If the patient responds partially to treatment with high doses of glucocorticoids with cyclophosphamide, intravenous cyclophosphamide (0.5-1 g/m2) is given quarterly for 18 months. If the patient responds to this therapy, maintenance therapy which is mentioned above, is given. However, if the patient does not respond to this treatment or has a recurrence, we will be treated same as a patient who has not responded to high-dose glucocorticoids with cyclophosphamide which will be explained.
If the patient does not respond to high doses of intravenous
glucocorticoid with cyclophosphamide, rituximab 375 mg/m2 is
given weekly for up to two weeks or 1 gram with two weeks apart.
And if this therapy is not efficient, plasmapheresis daily or every
other day (1-1.5 total plasma volumes) for 3-6 days or IVIG (2g/
kg for 2-5 days) are the other options. And finally, if the patient
does not respond to these treatments the autologous stem cell
transplantation is the last option.
3. The NPSLE patients, who are categorized in the ischemic
group according to the type of NP symptoms the clinical
approach is different. All of these patients need intensive
control of the risk factors for cerebrovascular diseases, for
example statins (goal LDL-cholesterol<70 mg/dl) and ACE
inhibitors should be prescribed.
4. If the diagnostic findings are in favor of the
atherothrombotic events, the patient should be evaluated for
APL antibodies and if a definitive diagnosis of APS is confirmed,
the patient will be given long term oral anticoagulants. ASA
100 mg (antiplatelet) may need to be added to treatment if
recurrent vascular events occur or previous vascular lesions
worsen.
5. But, ASA 100mg (antiplatelet) should be prescribed if the
patient is not definitively diagnosed as APS or has negative APL
antibodies. If second ischemic events occur, another antiplatelet
should be given instead of aspirin such as clopidogrel 75 mg
(Figure 7) [27, 28, 30].
Conclusion
Systemic lupus erythematosus (SLE) is a chronic autoimmune disorder characterized by antibodies to nuclear and cytoplasmic antigens, in which the immune system attacks its own tissues, leading to extensive inflammation and tissue damage in the affected organs. SLE is more common in women than men by nearby 10 to 1. Neuropsychiatric manifestations are a frequent event in SLE patients, and considered as a diagnostic and therapeutic problem to the physician. Despite diagnosis and management of NPSLE patients has not developed considerably recently, the early diagnosis of NPSLE and use of empirical treatments have been considered as a life-saving tool. It seems reasonable that elevated understanding of the pathogenesis of NPSLE and any of its symptoms will boost the probability of finding targeted treatments and an evidence-based method to management.
Acknowledgement
None.
Conflict of Interest
No Conflict of interest.
References
- Ricarte I, LA Dutra, FF Abrantes, FF Toso, OGP Barsottini, et al. (2018) Neurologic manifestations of antiphospholipid syndrome. Lupus 27(9): 1404-1414.
- Lam GK, M Petri (2005) Assessment of systemic lupus erythematosus. Clinical and experimental rheumatology 23(5): S120.
- de Amorim JC, Renan Bazuco Frittoli, Danilo Pereira, Mariana Postal, Sergio San Juan Dertkigil, et al. (2019) Epidemiology, characterization, and diagnosis of neuropsychiatric events in systemic lupus erythematosus. Expert review of clinical immunology 15(4): 407-416.
- Zirkzee EJ, Gerda M Steup-Beekman, Roos C van der Mast, Eduard L E M Bollen, Nic J A van der Wee, et al. (2012) Prospective study of clinical phenotypes in neuropsychiatric systemic lupus erythematosus; multidisciplinary approach to diagnosis and therapy. The Journal of rheumatology 39(11): 2118-2126.
- Bortoluzzi A, CA Scirè, M Govoni (2018) Attribution of neuropsychiatric manifestations to systemic lupus erythematosus. Frontiers in medicine 5: 68.
- Aringer M, Karen Costenbader, David Daikh, Ralph Brinks, Marta Mosca, et al. (2019) European League Against Rheumatism/American College of Rheumatology Classification Criteria for Systemic Lupus Erythematosus. Arthritis Rheumatol 71(9): 1400-1412.
- Bertsias, G, JPA Ioannidis, M Aringer, E Bollen, S Bombardieri, et al. (2010) EULAR recommendations for the management of systemic lupus erythematosus with neuropsychiatric manifestations: report of a task force of the EULAR standing committee for clinical affairs. Annals of the rheumatic diseases 69(12): 2074-2082.
- Hanly J (2004) ACR classification criteria for systemic lupus erythematosus: limitations and revisions to neuropsychiatric variables. Lupus 13(11): 861-864.
- Hermosillo Romo, D, RL Brey (2002) Diagnosis and management of patients with neuropsychiatric systemic lupus erythematosus (NPSLE). Best Practice & Research Clinical Rheumatology 16(2): 229-244.
- Lynall M (2018) Neuropsychiatric symptoms in lupus. Lupus 27(1_suppl): 18-20.
- Fujieda Y (2020) Diversity of neuropsychiatric manifestations in systemic lupus erythematosus. Immunol Med 43(4): 135-141.
- Shaban A, EC Leira (2019) Neurological Complications in Patients with Systemic Lupus Erythematosus. Curr Neurol Neurosci Rep 19(12): 97.
- Govoni M, JG Hanly (2020) The management of neuropsychiatric lupus in the 21st century: still so many unmet needs? Rheumatology 59(Supplement_5): v52-v62.
- Barber CE, Renée Leclerc, Dafna D Gladman, Murray B Urowitz, Paul R Fortin (2011) Posterior reversible encephalopathy syndrome: an emerging disease manifestation in systemic lupus erythematosus. Semin Arthritis Rheum 41(3): 353-63.
- Monov S, D Monova (2008) Classification criteria for neuropsychiatric systemic lupus erythematosus: do they need a discussion? Hippokratia 12(2): 103.
- Valdez-López, M, Eduardo Aguirre-Aguilar, Sergio Iván Valdés-Ferrer, Francisco M Martínez-Carrillo, Antonio Arauz, et al. (2021) Posterior reversible encephalopathy syndrome: a neuropsychiatric manifestation of systemic lupus erythematosus. Autoimmunity Reviews 20(2): 102739.
- Hanly JG, Elizabeth Kozora, Steven D Beyea, Julius Birnbaum (2019) Nervous system disease in systemic lupus erythematosus: current status and future directions. Arthritis & rheumatology 71(1): 33-42.
- Schwartz N, AD Stock, C Putterman (2019) Neuropsychiatric lupus: new mechanistic insights and future treatment directions. Nat Rev Rheumatol 15(3): 137-152.
- Medhat BM, A Moghazy, M Eissa (2020) Prevalence and characteristics of neuropsychiatric involvement in an Egyptian cohort of systemic lupus erythematosus patients: a single-center retrospective cohort. Egyptian Rheumatology and Rehabilitation 47(1): 1-8.
- Manca E (2021) Autoantibodies in Neuropsychiatric Systemic Lupus Erythematosus (NPSLE): Can They Be Used as Biomarkers for the Differential Diagnosis of This Disease? Clinical Reviews in Allergy & Immunology: 1-16.
- Sciascia S, Maria Laura Bertolaccini, Dario Roccatello, Munther A Khamashta, Giovanni Sanna, et al. (2014) Autoantibodies involved in neuropsychiatric manifestations associated with systemic lupus erythematosus: a systematic review. Journal of neurology 261(9): 1706-1714.
- Fanouriakis A, DT Boumpas, GK Bertsias (2013) Pathogenesis and treatment of CNS lupus. Current opinion in rheumatology 25(5): 577-583.
- Petri M (2011) Use of hydroxychloroquine to prevent thrombosis in systemic lupus erythematosus and in antiphospholipid antibody–positive patients. Current rheumatology reports 13(1): 77-80.
- Zhang Y, H Han, L Chu (2020) Neuropsychiatric lupus Erythematosus: future directions and challenges; a systematic review and survey. Clinics 75.
- Nikolopoulos D, A Fanouriakis, G Bertsias (2021) Treatment of neuropsychiatric systemic lupus erythematosus: clinical challenges and future perspectives. Expert Review of Clinical Immunology 17(4): 317-330.
- Papachristos D, S Oon, J G Hanly, M Nikpour (2021) Management of inflammatory neurologic and psychiatric manifestations of systemic lupus erythematosus: A systematic review. in Seminars in Arthritis and Rheumatism Elsevier 51(1): 49-71.
- Magro-Checa C, Elisabeth J Zirkzee, Tom W Huizinga, Gerda M Steup-Beekman (2016) Management of neuropsychiatric systemic lupus erythematosus: current approaches and future perspectives. Drugs 76(4): 459-483.
- Sarwar S Alaa S Mohamed, Sylvette Rogers, Shah T Sarmast, Saurabh Kataria, et al. (2021) Neuropsychiatric Systemic Lupus Erythematosus: A 2021 Update on Diagnosis, Management, and Current Challenges. Cureus 13(9): e17969.
- Seet D, Nur Azizah Allameen, Sen Hee Tay, Jiacai Cho, Anselm Mak, et al. (2021) Cognitive Dysfunction in Systemic Lupus Erythematosus: Immunopathology, Clinical Manifestations, Neuroimaging and Management. Rheumatology and Therapy: 1-29.
- Sanna G, ML Bertolaccini, MA Khamashta (2008) Neuropsychiatric involvement in systemic lupus erythematosus: current therapeutic approach. Current pharmaceutical design 14(13): 1261-1269.
-
Saeed Shahbeigi* and Mojdeh Bolouchian. Cerebrovascular Accident as a First Manifestation of Neuropsychiatric Systemic Lupus Erythematosus; a Comprehensive Review; a Case Report. Arch Neurol & Neurosci. 12(5): 2022. ANN.MS.ID.000799.
-
Cerebrovascular, Neuropsychiatric, Erythematosus, Comprehensive Review, Pathophysiology, Pathophysiology, Epidemiology, Diagnostic Approach, Cerebrovascular Accident; Neuropsychiatric Systemic Lupus Erythematosus; SLE; NPSLE
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






