Review Article
Review Article
Rehabilitation After Hip Arthroscopy: A Criterion Based Approach
Brian Serrano, Chicago Bulls Basketball Club, USA
Received Date: July 10, 2024; Published Date: July 12, 2024
Hip surgical intervention in the United Stated has grown over the last 20 years. Patients with hip pathology such as femoroacetabular impingement (FAI) and labral tears will usually undergo arthroscopic surgery after failing conservative care. After arthroscopy, a proper rehabilitation protocol is crucial for achieving excellent patient reported outcome measures (PROMs). The current literature regarding PROMs and hip arthroscopy rehabilitation protocols lacks evidence and reproducibility. This makes it difficult to make correlations between surgery, rehabilitation, and PROMs. Other studies that provide descriptive rehabilitation protocols after hip arthroscopy also yield insufficient information for critical appraisal. To improve studies involving PROMs, it is important to describe rehabilitation protocols that are reproducible. The purpose of this paper is to provide a descriptive and reproducible rehabilitation protocol that can be used by clinicians and researchers to improve outcomes following hip arthroscopy. It is evident there is a gap in the published literature regarding hip arthroscopy rehabilitation protocols to date. If rehabilitation protocols could be designed with enough information to be reproducible, this could strengthen the correlation between hip arthroscopy and PROMs.
Keywords:Hip Arthroscopy; FAI; Labral Tear; Labral Repair; Rehabilitation
Introduction
The diagnosis of FAI and labral tears is increasingly common; with an estimated prevalence of 64% in active individuals and 49% in the general population [1,2]. FAI can occur as CAM (49%), Pincer (19%) or a mixed type (40%) [1]. CAM impingement occurs when there is loss of sphericity at the femoral head-neck junction due to excess bone formation [3]. Pincer impingement occurs when there is over coverage of the acetabulum due to a deep or retroverted acetabulum [3]. Mixed impingement is the most common form of FAI and occurs when a patient presents with CAM and Pincer simultaneously [3]. Labral tears of the hip can occur from at least five different etiologies: trauma, FAI, capsular laxity/ hip hypermobility, dysplasia, and degeneration [4]. Labral tears can also stem from repetitive motions of the hip leading to microtrauma and eventual labral injury [5]. The altered joint loading caused by symptomatic FAI may lead to progressive injury of the labrum due to separation from the acetabular rim and subsequent chondral damage [4].
FAI is usually treated with a trial of conservative care involving physical therapy, corrective exercises, and manual therapy [6]. The purpose of conservative care should be to improve hip stability, neuromuscular control, and promote efficient movement patterns [3]. While conservative care may be successful in some populations, surgical intervention may be warranted and necessary in patients who seek to maintain an active lifestyle or participate in sports [7]. Hip surgical techniques have evolved in the United States leading to arthroscopy becoming the prevalent technique in treating patients with FAI and labral tears [4]. Patients with FAI will typically have an acetabular osteoplasty and/or femoral osteoplasty to re-shape the osseous structures and reduce the occurrence of impingement [8]. Patients with labral tears will undergo a labral repair to promote even load bearing at the hip joint and potentially reduce the incidence of secondary hip osteoarthritis [9].
Following hip arthroscopy, a proper rehabilitation protocol is important for patients to achieve excellent PROMs. However, there is a gap in current literature regarding this subject [10-12]. The importance of a well-structured rehabilitation program cannot be understated for patients who seek to return to high levels of physical activity or athletic performance. A recent review by Reiman et al. (2020) found limited and inconsistent reporting of post-operative rehabilitation for FAI [13]. They report that patient reported outcome studies describe surgery in detail; however, most rehabilitation protocols lacked enough information to be suitable for replication [13]. Due to these confounding factors, the authors could not draw conclusions about the extent to which postoperative rehabilitation influences surgical outcomes. We utilized current evidence, high volume hip arthroscopic surgeon expertise, and clinician experience to design a hip arthroscopy rehabilitation protocol that can be used as a benchmark for clinicians and researchers.
Background
This rehabilitation protocol was made using criteria set forth
by Cvetanovich et al. (2017) and Reiman et al. (2020) to ensure
reproducibility and includes:
1. Phase Description
2. Exercises or primary principles for each phase listed
3. Weightbearing (WB) limitations and timeframe
4. Range of Motion (ROM) limitations and timeframe
5. Brace use/no use and timeframe
6. CPM use/no use and timeframe
7. All details are discussed relative to adjustments based on
surgical procedure performed
Rehabilitation
Similar to Kuhns et al. (2017) and Spencer-Gardner et al. (2014) this study describes a six-phase rehabilitation protocol when returning patients to sport after arthroscopic hip surgery [7, 14]. Active patients will likely meet their rehabilitation goals upon completion of phase four, while phase five is necessary for athletes looking to return to sport. If possible, the patient should undergo a prehabilitation (prehab) phase for at least 4 weeks prior to surgery.
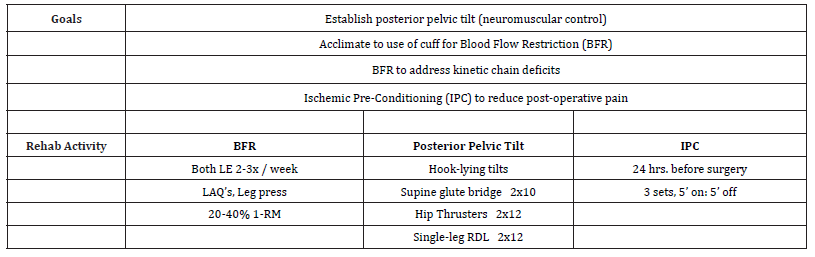
Phase 0 (4-6 weeks before surgery)
Patients are encouraged to perform a trial of prehab at least four to six weeks pre surgery. Topp et al. (2009) found prehab to yield a decrease in pain levels, improved six-minute walk time, and greater leg strength symmetry in patients after a total knee arthroplasty (TKA) [15]. A pilot study by Grant et al. (2017) found a positive trend in knee extension strength, hip flexion strength, and increased general health (EQ-5D-5L) in their prehab group [16]. Personalized Blood Flow Restriction (PBFR) utilizes a pressurized cuff on the proximal limb to reduce blood flow into muscle during resistance exercise. This technique can be used in load compromised limbs to achieve increases in size and strength with loads as light as 20% 1RM [17,74]. Its safety has been examined along with recommendations for parameters [18,31,74,75]. PBFR may be utilized, incorporating large muscle groups two-three times per week to address kinetic chain size and strength reductions from disuse [76,77], Blood flow restriction training may also be used as a means to pre-condition the limb in preparation for the immediate post-op disuse period [78,79]. A cadaveric study by Patel et al. (2019) found that hip impingement occurs earlier in hip internal rotation in the presence of increased anterior pelvic tilt [19]. The authors concluded that abduction and posterior pelvic tilt increased impingement free ROM in the hip. This finding guided our inclusion of exercises focused on increasing posterior pelvic tilt during the prehab phase [19]. Exercises to increase the strength of the hip extensors and abductors like using hip thrusters and single-leg Romanian deadlifts (RDL) were chosen due to their ability in recruiting musculature that improves posterior pelvic tilt as compared to other resistance exercises [20,21]. Lastly, Ischemic Pre-Conditioning (IPC) may be performed 24 hours prior to surgery for its potential effect in reducing post-surgical pain [22]. Pereira et al. (2014) found that an IPC protocol of three sets of a five-minute treatment of limb occlusion, measured by ipsilateral patient specific limb occlusion pressure, and five minutes of rest between each set, led to reduced post-surgical pain [22].
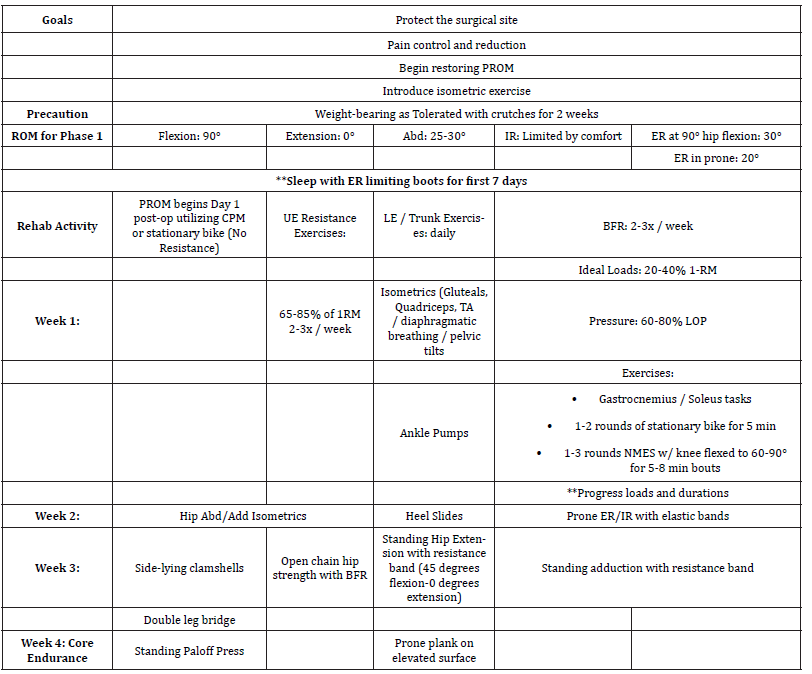
Immediate Post-Surgical Instructions (Week 0-3)
Weightbearing is progressed as tolerated with the use crutches for two weeks post-operatively to provide stability and support during gait [23]. Range of Motion (ROM) is recommended in pain-free limits of motion while avoiding extreme hip flexion and extension [11]. The patient is provided a brace that restricts hip flexion to 90 degrees for use when ambulating with crutches for the first two weeks [26]. From post-operative day one the patient begins gentle ROM using a continuous passive motion machine (CPM) three times per day for 30 minutes [24]. During CPM hip flexion is limited to less than 90 degrees to avoid strain on the repaired labrum and hip capsule. For the first seven nights post-surgery, the patient sleeps with foam boots that limit external rotation which could potentially stress the repaired hip capsule [24, 25]. While literature on efficacy of the boots is scarce, the corresponding author A.C. has seen one case of a patient who was non-compliant with his boots, which could have led to the breakdown of his capsular repair, as evident by his increased resting external rotation compared to contralateral side in the supine position. The patient required revision arthroscopy for capsular closure. Naprosyn (anti-inflammatory) is prescribed 500mg BID for the first 30 days after surgery to both reduce the amount of narcotic medication taken and to reduce the risk of heterotopic ossification [27]. Driving is usually resumed at day 10 post-surgery, and the patient must show good neuromuscular control of the leg prior to driving. The patient’s first post-operative appointment is scheduled 10-12 days after surgery and at that time sutures are removed.
Table 1:Phase 0 (4-6 weeks before surgery).
Phase 1 (Week 0-4)
Phase 1 is primarily concerned with protecting the surgical site to allow for healing of incisions, the repaired labrum, and repaired capsule. There is limited evidence regarding the healing time of the hip capsule, but a time period of three-four weeks seems to be sufficient for motion restriction limits based on clinical guidelines in previous studies [11, 26]. The labrum has a longer healing time to acquire adequate strength, with evidence showing adequate healing in an ovine model by about 12 weeks [28]. Goals of this phase include protecting the surgical site depending on surgical procedure performed, minimizing pain, begin to restore ROM, and beginning strength exercises in an isometric manner. Initially, ROM is limited to 90 degrees of flexion, 0 degrees of extension, 25-30 degrees of abduction, and 30 degrees of external rotation [25]. Resistance exercise in the lower extremity begins as isometrics of the hip musculature, and isotonic strengthening of distal musculature that avoids patient discomfort and co-contraction if hip flexors. PBFR exercise in the early phase of rehab is valuable due to its ability to provide a growth stimulus with very little load. Its safety has been examined, and the ability to limit atrophy as well as strength loss during this temporary disuse period provides for the maintenance of muscular capacity needed for later phases of rehab when the involved tissues can tolerate heavier loads. Exercises with PBFR targeting the quadriceps, hamstrings, and gluteals are of chief importance [31]. Resistance training of the upper extremities can begin immediately after surgery to keep the body active, promote circulation, and reduce muscular atrophy [29]. Weeks two-four include progressions into isotonic strengthening of the hip musculature, such as side-lying clamshells and standing hip extension with light resistance. Week three begins the addition of a double leg-bridging, while week four progresses to more intensive core endurance exercises such as a modified plank [30].
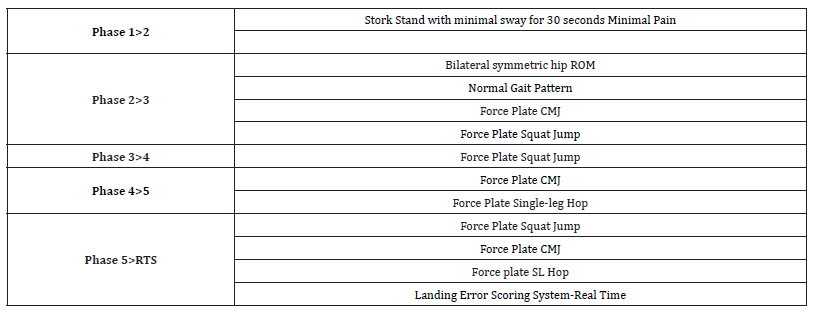
Criteria for progression: The patient should be able to perform a stork stand: standing on one leg with hands on hips and contralateral hip flexed to 90 degrees with eyes open, with minimal sway for 30 seconds [24].
Table 2:Phase 1(Week 0-4).
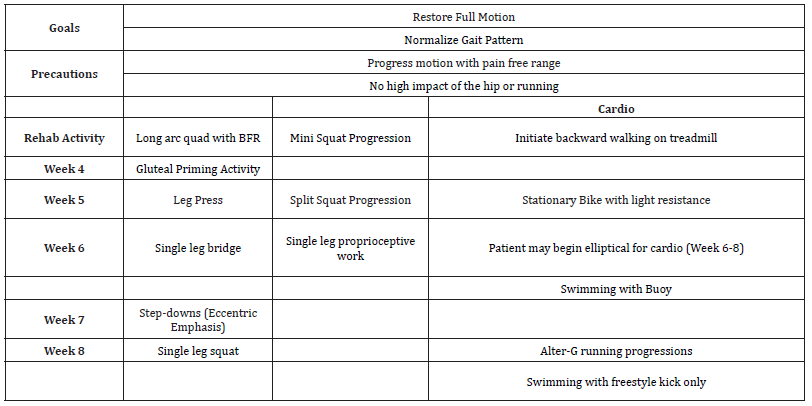
Phase 2 (Week 4-8)
The goals for this phase are to restore full ROM and normalization of gait by emphasizing a heel-toe strike pattern and knee extension [32]. Motion should be progressed in a pain-free manner, while avoiding high impact activity of the hip such as running. Prior to strength activities, a gluteus medius warm-up should be performed to promote hip abduction and proper hip mechanics during the gait cycle [33]. Resistance exercises begin with long arc quad using PBFR in week four, [34] along with mini squats, and progresses to a single leg (SL) bridge in week six, and SL squat in week eight [35]. For cardiovascular training, the patient begins with forward walking on the treadmill in week four [36] and progresses to swimming with a pool buoy to protect the hip against excessive motion during week six [25]. Backward walking is also recommended to impose a different biomechanical and physiological stimulus to the body, which includes an increase in knee extensor muscle activation and greater total muscle activation in the lower extremity as compared to forward walking [64, 65]. As it relates to hip rehabilitation at this stage of labral healing, backward walking induces greater ROM at the ankle and knee, while avoiding overextension of the hip, thus promoting joint movement without excess strain on the labrum [65, 66].
Criteria for progression: Force Plates (Vald Performance; Queensland, AU) are utilized to assess ground reaction forces and strength asymmetries which have been validated in the literature [80, 81]. At this phase, the double-leg squat (squat) is used to assess inter-limb asymmetry and preparedness for progression. The squat is also useful to evaluate compensatory strategies in a safe environment. Sigward et al. (2018) found differences between patients at 3- and 5-month time periods post-ACL reconstruction in knee flexion angles, vertical ground reaction forces, and hip-to-knee extensor ratio [67]. Similarly, Labanca et al. (2015) found that asymmetrical loading during a squat 1 month after ACL reconstruction predicted asymmetrical loading at 6 months during force plate jump testing [68]. By assessing the squat on the force plates early in the rehabilitation process, clinicians can potentially obtain objective information to guide exercise prescription.
Table 3:Phase 2 (Weeks 4-8).
Phase 3 (8-12 weeks)
The goals of phase three are to increase muscular strength and continue to address muscle size deficits. The patient is prepared for change of direction activities and begins an unloaded running progression (either a pool or Alter-G) [37]. During this phase it is important to be mindful of repetitive hip flexion as an isolated resistance exercise to reduce the risk of iliopsoas tendinitis [13]. Due to the muscular imbalance seen in patients with labral tears and FAI, it is important to include exercise to increase strength of the hip extensors and abductors [16]. The exercises within this phase aim to strengthen the hip musculature with incorporation of the entire kinetic chain. During week eight, the Copenhagen plank [38] is added for adductor strengthening, along with pistol squats and the trap bar deadlift. The pistol squat and trap bar deadlift are utilized to promote strength in the hip and the entire limb [39-41]. During week 9, strength in multiple planes of direction is implemented as multidirectional hip strength has been shown to reduce injury risk [14, 42]. Low impact ladder drills begin week 10 which evolve into a base position, this is purposeful to aid in transition to a jumping progression [43]. The jumping progression is taught using a bottom-up approach, where the patient is taught how to land before jumping on two feet, then progresses into singleleg activity. For cardiovascular training, the patient may begin swimming without a pool buoy, using the freestyle stroke only (to limit the increased hip motion against resistance with other kicks), while keeping track of variables such as frequency, intensity, and duration [9]. The utilization of Alter-G in this phase provides an early initiation of running, allowing for safe acceleration of functional activity, while protecting the labrum as it continues to heal [44]. Use of the Alter-G does not alter mechanics at the hip, knee, or ankle, and allows normalized muscle firing patterns [44].
Criteria for progression: Force Plates (Vald Performance; Queensland, AU) are utilized for strength measurements looking at three different jumping tasks: Squat Jump (SJ), Counter Movement Jump (CMJ), and the Single Leg Hop (SL) [82-84]. These jumping tasks are used to assess asymmetries that are present, rate of force development, and eccentric rate of force development [84]. Our testing procedure is standardized and includes a warm-up of 5 bodyweight squats, 2 submaximal CMJ, and 2 submaximal SL hops before testing begins. The testing of each jump task includes 3 trials and is then averaged for further analysis based on a similar protocol by de Fontenay et al. (2015) and O’Malley et al. (2018) [72, 73]. Difabrio et al. (2018) use the bilateral vertical drop jump as part of their lower extremity assessment protocol (LEAP) [69]. Baumgart et al. (2015) used the double-leg and single-leg jump tasks to measure vertical ground reaction forces (vGRF), these authors found a correlation between scores on the International Knee Documentation Committee Subjective Form and limb asymmetry [70]. Our protocol uses SJ and CMJ to assess a double-limb task. The SJ is performed by having the subject place their hands on their hips to provide more accurate lower extremity data, by reducing the influence of arm swing and limiting the stretch-shortening cycle. The SL hop is used because it is a sensitive measure of restored function after ACLR [71]. The patient should meet a limb symmetry index (LSI) of at least 80% across all three jump tasks to progress into phase four [62].
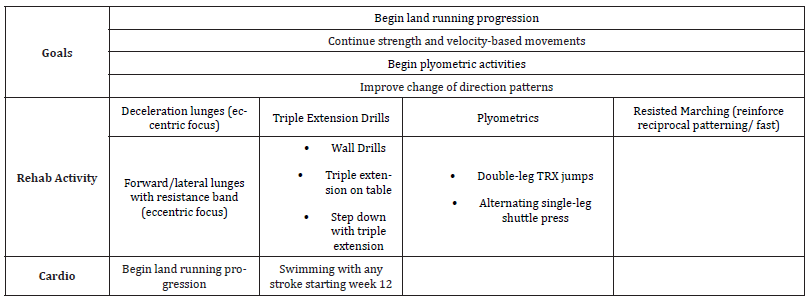
Phase 4 (12-16 Weeks)
The goals of phase four are to begin a land running progression, begin plyometric activities, and to improve change of direction ability. Greater loads may now be progressively increased based on likely healing of the labrum [9]. Eccentric strength of the lower extremity is now emphasized using lunges in the sagittal and frontal plane [45]. Decreased eccentric hip strength has been found to be a risk factor for hamstring injuries [46], adductor injuries [47], and patellofemoral pain [48]. For patients that strive to return to performance [49] or running, the clinician should incorporate triple extension drills. Triple extension drills serve to increase the motor coordination needed to execute the movement patterns critical to running and jumping [50]. Plyometrics started week 12 with double leg TRX jumps and alternating SL leg shuttle press. TRX jumps are utilized to allow the upper extremities to support the integrity of the plyometric exercise (stretch-shortening cycle and short ground contact time) without the patient having to worry about their balance [51, 52]. For cardiovascular training, the patient may begin treadmill running progression and swim with any stroke style, staying mindful of frequency, intensity, and duration.
Criteria for progression: Includes force plate testing using the SJ, max CMJ, and max SL Hop as described in detail in the previous section. Based on the literature by Schmitt et al. (2015), progression into Phase five will be met by an LSI of at least 85% across all three jump tasks [53, 63].
Table 4:Phase 3 (Weeks 8-12).
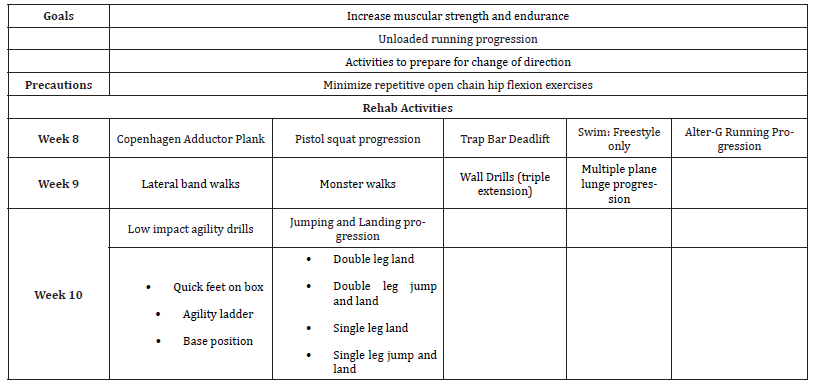
Table 5:Phase 4 (Weeks 12-16).
Phase 5 (16-20 Weeks)
The goals of Phase five are to prepare the athlete for higher levels of physical activity with quick change of direction exercises, and preparation for the different phases of running: acceleration, deceleration, and absolute speed. The acceleration phase of sprinting takes place from about 0-40m while absolute speed occurs from about 40-60m using a 100m sprint as a reference [54, 55]. Thus, the clinician should incorporate sprints using these distances to train acceleration and absolute speed. Deceleration can be trained in a variety of ways and may include having the patient slow down over progressively shorter distances to gradually increase load on the lower extremities. Rehab activity should now include progressive agility drills, lateral box jumps, lateral step-offs, and counter movement jumps (CMJ). Lateral box jumps and CMJs are added to increase power and rate of force development [56].
Criteria for return to performance: Progression will involve three jump tasks on the force plate: max SJ, max CMJ, and max SL Hop. To begin a return to sport progression, while reducing the risk of re-injury there should be an LSI of at least 90% across all three jump tasks [53, 62, 63]. These recommendations come from data used in ACL return to sport criteria given the lack of available evidence in the hip literature.
Table 6:Phase 5 (Weeks 16-20).
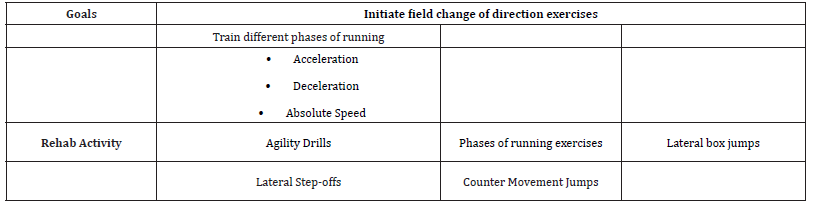
Table 7:Criteria for progression.
Discussion
With evolving technology and emerging techniques in the field of hip arthroscopy, it is important that surgeons and clinicians strive to improve patient outcomes [57]. Over the last 20 years, there has been an exponential increase in the use of arthroscopy for the surgical management of FAI and labral tears [58]. There are currently a multitude of patient reported outcome studies published, however they lack clarity in their rehabilitation protocols for reproduction. This scarcity of specificity in rehabilitation protocols is evident. For example, a systematic review by Rath et al. (2017) found limited evidence-based data in creation of rehabilitation protocols [59]. They also found marked variability exists in the post-op weightbearing practices of hip arthroscopy surgeons [59]. Similarly, Smith et al. (2017) created a 21-question survey that addressed 3 aspects of hip arthroscopy: patient evaluation, intra-operative technique, and post-operative management, this survey was distributed to 150 orthopedic surgeons internationally [60]. The authors found several areas of post-operative management remain without universal agreement such as use of a brace, weight bearing status, and early initiation of muscle activity. Lastly, Cvetanovich et al. (2017) performed an online search of surgeons that yielded 31 out of 111 (27.9%) have available rehabilitation protocols [10]. Within these 31 protocols, there was substantial variation in the activities performed and in time points for initiating activities [10]. These are just a few examples that demonstrate the disparities that exist among post-operative hip arthroscopy rehabilitation protocols. Our findings align with those of Reiman et al. (2020) [13]; that many protocols describe surgical technique in depth but only provide an overview of exercises used in each phase, while criteria for progression of each phase is often vague and references are limited. Creating a rehabilitation protocol with appropriate criteria for replication is of great importance. Surgical and patient reported outcome studies need the following areas to be of strong quality: The surgical technique, patient reported outcome used, and the rehabilitation protocol [61]. The recent review by Reiman et al. (2020) found that only 8% of rehabilitation protocols were classified as exceptional; the protocol could be taken into a clinic by a patient with confidence that any rehab clinician would have enough information for immediate implementation [13]. If out of multitudes of studies only a low number meet this exceptional criterion, this begs the question about the true correlation between hip arthroscopy and patient reported outcomes in existing studies. If correlations are to be made in patient reported outcome studies; there needs to be better detail and reproducibility in the rehabilitation protocol. A noted limitation of this rehabilitation protocol is that not everyone will have access to force plates to assess criteria for progression. While this may be a limiting factor for clinicians implementing this protocol, the evidence behind force plate testing is growing as a more comprehensive and functional manner to assess strength before returning to play [85, 86]. It is recommended for clinicians to strive to test their patients using force plate data in some capacity. The biggest strength of force plate testing is the numerous metrics that can be measured by adding to the information available to the clinician. Metrics such as concentric mean force, eccentric mean force, peak landing force, and inter-limb asymmetry can all be quantified [87, 88]. This may serve to add another layer of protection between the athlete and risk of re-injury as they prepare to return to sport.
Conclusion
The effectiveness of a rehabilitation protocol is critical to improve patient health, well-being, and to achieve excellent outcomes. As surgical techniques evolve, then so should rehabilitation techniques for associated procedures. There is currently no best practice as to how to produce a rehabilitation protocol leading to the substantial variability seen today. Therefore, the authors decided to use a novel criterion that uses seven objective checkpoints. Using this criterion, a rehabilitation protocol for use after hip arthroscopy was created. This rehabilitation protocol is meant to provide clinicians and researchers with a detailed program, created with the best available evidence, and surgeon and clinician expertise, with enough detail to be reproduced for widespread use in practice and patient reported outcome studies.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Mascarenhas VV, Rego P, Dantas P, Morais F, McWilliams J, Collado D, et al (2016) Imaging prevalence of femoroacetabular impingement in symptomatic patients, athletes, and asymptomatic individuals: a systematic review. European journal of radiology 85(1): 73-95.
- Kemp J, Grimaldi A, Heerey J, Jones D, Scholes M, et al. (2019) Current trends in sport and exercise hip conditions: Intra-articular and extra-articular hip pain, with detailed focus on femoroacetabular impingement (FAI) syndrome. Best Practice & Research Clinical Rheumatology 33(1): 66-87.
- Griffin DR, Dickenson EJ, O'donnell J, Awan T, Beck M, et al. (2016) The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med 50(19): 1169-1176.
- Groh MM, Herrera J (2009) A comprehensive review of hip labral tears. Current reviews in musculoskeletal medicine 2(2): 105-117.
- Burnett RS, Della Rocca GJ, Prather H, Curry M, Maloney WJ, et al. (2006) Clinical presentation of patients with tears of the acetabular labrum. JBJS 88(7): 1448-1457.
- Lewis CL, Sahrmann SA (2006) Acetabular labral tears. Physical therapy 86(1): 110-121.
- Spencer-Gardner L, Eischen JJ, Levy BA, Sierra RJ, Engasser WM, et al. (2014) A comprehensive five-phase rehabilitation programme after hip arthroscopy for femoroacetabular impingement. Knee Surgery, Sports Traumatology, Arthroscopy 22(4): 848-859.
- Christopher M Larson, Carlos A Guanche, Bryan T Kelly, John C Clohisy, Anil S Ranawat (2009) Advanced techniques in hip arthroscopy. Instr Curse Lect 58: 423-436.
- Philippon MJ (2006) New frontiers in hip arthroscopy: the role of arthroscopic hip labral repair and capsulorrhaphy in the treatment of hip disorders. Instr course lect 55: 309-316.
- Gregory L Cvetanovich, Vincent Lizzio, Fabien Meta, Derek Chan, Ira Zaltz, et al. (2017) Variability and comprehensiveness of north american online available physical therapy protocols following hip arthroscopy for femoroacetabular impingement and labral repair. Arthroscopy 33(11): 1998-2005.
- Domb BG, Sgroi TA, VanDevender JC (2016) Physical therapy protocol after hip arthroscopy: clinical guidelines supported by 2-year outcomes. Sports Health 8(4): 347-354.
- Grzybowski JS, Malloy P, Stegemann C, Bush-Joseph C, Harris JD, et al. (2015) Rehabilitation Following Hip Arthroscopy- A Systematic Review. Frontiers in Surgery 2: 21.
- Reiman M, Boyd J, Ingel N, Reichert A, Westhoven M, et al. (2020) Limited and inconsistent reporting of postoperative rehabilitation for femoroacetabular impingement syndrome: a scoping review of 169 studies. Journal of Orthopaedic & Sports Physical Therapy 50(5): 252-258.
- Topp R, Swank AM, Quesada PM, Nyland J, Malkani A (2009) The effect of prehabilitation exercise on strength and functioning after total knee arthroplasty. PM&R 1(8): 729-735.
- Grant LF, Cooper DJ, Conroy JL (2017) The HAPI ‘Hip Arthroscopy Pre-habilitation Intervention’study: does pre-habilitation affect outcomes in patients undergoing hip arthroscopy for femoro-acetabular impingement? Journal of hip preservation surgery 4(1): 85-92.
- Loenneke JP, Wilson JM, Marín PJ, Zourdos MC, Bemben MG (2012) Low intensity blood flow restriction training: a meta-analysis. European journal of applied physiology112(5): 1849-1859.
- Patterson SD, Hughes L, Warmington S, Burr JF, Scott BR, et al. (2019) Blood Flow Restriction: Considerations of Methodology, Application and Safety. Frontiers in physiology 10: 533.
- Patel RV, Han S, Lenherr C, Harris JD, Noble PC (2019) Pelvic Tilt and Range of Motion in Hips with Femoroacetabular Impingement Syndrome. JAAOS-Journal of the American Academy of Orthopaedic Surgeons 28(10): e427-e432.
- Neto WK, Vieira TL, Gama EF (2019) Barbell hip thrust, muscular activation and performance: a systematic review. Journal of sports science & medicine 18(2): 198-206.
- Delgado J, Drinkwater EJ, Banyard HG, Haff GG, Nosaka K (2019) Comparison between back squat, Romanian deadlift, and barbell hip thrust for leg and hip muscle activities during hip extension. The Journal of Strength & Conditioning Research 33(10): 2595-2601.
- Pereira FEC, Mello IL, Pimenta FH de OM, Costo DM, Wong DVT, et al. (2016) A Clinical Experimental Model to Evaluate Analgesic Effect of Remote Ischemic Preconditioning in Acute Postoperative Pain. Pain Research and Treatment.
- Olufemi R Ayeni, Asheesh Bedi, Dean G Lorich, Bryan T Kelly (2011) Femoral neck fracture after arthroscopic management of femoroacetabular impingement: a case report. J Bone Joint Surg, Am 93(9): e47
- Edelstein J, Ranawat A, Enseki KR, Yun RJ, Draovitch P (2012) Post-operative guidelines following hip arthroscopy. Current reviews in musculoskeletal medicine 5(1): 15-23.
- Kuhns BD, Weber AE, Batko B, Nho SJ, Stegemann C (2017) A four-phase physical therapy regimen for returning athletes to sport following hip arthroscopy for femoroacetabular impingement with routine capsular closure. International journal of sports physical therapy 12(4): 683-696.
- Harris JD (2016) Capsular management in hip arthroscopy. Clinics in sports medicine 35(3): 373-389.
- Ma R, Chen GH, Zhao LJ, Zhai XC (2018) Efficacy of naproxen prophylaxis for the prevention of heterotopic ossification after hip surgery: a meta-analysis. Journal of orthopaedic surgery and research 13(1):
- Philippon MJ, Arnoczky SP, Torrie A (2007) Arthroscopic repair of the acetabular labrum: a histologic assessment of healing in an ovine model. Arthroscopy 23(4): 376-380.
- Vasiliadis AV, Maris A, Tsoupli A, Saridis A (2019) Rehabilitation exercise program after surgical treatment of quadriceps tendon rupture: A case report. Physical Therapy in Sport 39: 82-89.
- Voight ML, Robinson K, Gill L, Griffin K (2010) Postoperative rehabilitation guidelines for hip arthroscopy in an active population. Sports Health 2(3): 222-230.
- Hughes L, Paton B, Rosenblatt B, Gissane C, Patterson SD (2017) Blood flow restriction training in clinical musculoskeletal rehabilitation: a systematic review and meta-analysis. Br J Sports Med 51(13): 1003-1011.
- Adler KL, Cook PC, Geisler PR, Yen YM, Giordano BD (2016) Current concepts in hip preservation surgery: part II-rehabilitation. Sports health 8(1): 57-64.
- Kraeutler MJ, Anderson J, Chahla J, Mitchell JJ, Thompson-Etzel R, et al. (2017) Return to running after arthroscopic hip surgery: literature review and proposal of a physical therapy protocol. Journal of hip preservation surgery 4(2): 121-30.
- Bowman EN, Elshaar R, Milligan H, Jue G, Mohr K, et al. (2019) Contralateral Effects of Blood Flow Restriction Training on the Lower Extremities: A Randomized Controlled Trial. Sports health 11(2): 149-156.
- Hyland DE, Winkelmann ZK, Games KE (2018) Evidence-Based Rehabilitation for Hip Arthroscopy. Athletic Training and Sports Health Care 11(3): 103-104.
- Lee M, Kim J, Son J, Kim Y (2013) Kinematic and kinetic analysis during forward and backward walking. Gait & Posture 38(4): 674-678.
- Peebles LA, O’Brien LT, Dekker TJ, Kennedy MI, Akamefula R, et al. (2019) The Warrior Athlete Part 2—Return to Duty in the US Military: Advancing ACL Rehabilitation in the Tactical Athlete. Sports medicine and arthroscopy review 27(3): e12-e24.
- Ishøi L, Sørensen CN, Kaae NM, Jørgensen LB, Hölmich P, et al. (2016) Large eccentric strength increase using the Copenhagen Adduction exercise in football: A randomized controlled trial. Scandinavian journal of medicine & science in sports 26(11): 1334-1342.
- Claiborne TL, Armstrong CW, Gandhi V, Pincivero DM (2016) Relationship between hip and knee strength and knee valgus during a single leg squat. Journal of applied biomechanics 22(1): 41-50.
- Blanchard J, Berning J, Adams KJ, DeBeliso M (2016) Effects of the trap bar deadlift and leg press on adolescent male strength, power and speed. Journal of Physical Education Research 2: 11-22.
- Moon BH, Lim YJ, Kim JW (2020) Effects of Various Deadlifts on the Muscle Activity of the Trunk and Lower Extremity. Medico Legal Update 20(1): 2203-2207.
- Baker RL, Souza RB, Fredericson M (2011) Iliotibial band syndrome: soft tissue and biomechanical factors in evaluation and treatment. PM&R 3(6): 550-561.
- Shaw KA, Jacobs JM, Evanson JR, Pniewski J, Dickston ML, et al. (2017) Functional outcomes of hip arthroscopy in an active duty military population utilizing a criterion-based early weight bearing progression. International journal of sports physical therapy 12(5): 840-847.
- Draovitch P, Maschi RA, Hettler J (2012) Return to sport following hip injury. Current reviews in musculoskeletal medicine 5(1): 9-14.
- Cheatham SW, Kolber MJ (2012) Rehabilitation after hip arthroscopy and labral repair in a high school football athlete. International journal of sports physical therapy 7(2): 173-184.
- Sugiura Y, Saito T, Sakuraba K, Sakuma K, Suzuki E (2008) Strength deficits identified with concentric action of the hip extensors and eccentric action of the hamstrings predispose to hamstring injury in elite sprinters. Journal of orthopaedic & sports physical therapy 38(8): 457-464.
- Hrysomallis C (2009) Hip adductors' strength, flexibility, and injury risk. The Journal of Strength & Conditioning Research 23(5): 1514-1517.
- Ramskov D, Barton C, Nielsen RO, Rasmussen S (2015) High eccentric hip abduction strength reduces the risk of developing patellofemoral pain among novice runners initiating a self-structured running program: a 1-year observational study. journal of orthopaedic & sports physical therapy 45(3): 153-161.
- Buckthorpe M, Frizziero A, Roi GS (2019) Update on functional recovery process for the injured athlete: return to sport continuum redefined 53(5): 265-267.
- Lorenz D (2016) Facilitating power development in the recovering athlete: Triple extension in rehabilitation. Strength & Conditioning Journal 38(1): 48-50.
- Flanagan EP, Comyns TM (2008) The use of contact time and the reactive strength index to optimize fast stretch-shortening cycle training. Strength & Conditioning Journal 30(5): 32-38.
- Bubke CJ, Shim A, Ruppert TARA, Waller M (2019) Adaptations to balance training using the Shuttle TNT System in female NAIA athletes. Medicina Sportiva: Journal of Romanian Sports Medicine Society 15(1): 3030-3035
- Schmitt LC, Paterno MV, Ford KR, Myer GD, Hewett TE (2015) Strength asymmetry and landing mechanics at return to sport after ACL 47(7): 1426-1434.
- Nagahara R, Mizutani M, Matsuo A, Kanehisa H, Fukunaga T (2018) Association of sprint performance with ground reaction forces during acceleration and maximal speed phases in a single sprint. Journal of Applied Biomechanics 32(2): 104-110.
- Manzer S, Mattes K, Holländer K (2016) Kinematic Analysis of Sprinting Pickup Acceleration versus Maximum Sprinting Speed. Biology of Exercise 12(2): 55-67.
- McLellan CP, Lovell DI, Gass GC (2011) The role of rate of force development on vertical jump performance. The Journal of Strength & Conditioning Research 25(2): 379-385.
- Bozic KJ, Chan V, Valone FH, Feeley BT, Vail TP (2013) Trends in hip arthroscopy utilization in the United States. The Journal of arthroplasty 28(8 Suppl): 140-143.
- Clohisy JC, Baca G, Beaulé PE, Kim YJ, Larson CM, et al. (2013) Descriptive epidemiology of femoroacetabular impingement: a North American cohort of patients undergoing surgery. The American journal of sports medicine 41(6): 1348-1356.
- Rath E, Sharfman ZT, Paret M, Amar E, Drexler M, et al. (2017) Hip arthroscopy protocol: expert opinions on post-operative weight bearing and return to sports guidelines. Journal of hip preservation surgery 4(1): 60-66.
- Smith KM, Gerrie BJ, McCulloch PC, Lewis BD, Mather RC, et al. (2017) Arthroscopic hip preservation surgery practice patterns: an international survey. Journal of hip preservation surgery 4(1): 18-29.
- Bennell KL, O’Donnell JM, Takla A, Spiers LN, Hunter DJ, et al. (2014) Efficacy of a physiotherapy rehabilitation program for individuals undergoing arthroscopic management of femoroacetabular impingement–the FAIR trial: a randomised controlled trial protocol. BMC musculoskeletal disorders 15: 58.
- Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA (2016) Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL cohort study. British journal of sports medicine 50(13): 804-808.
- Welling W, Benjaminse A, Lemmink K, Dingenen B, Gokeler A (2019) Progressive strength training restores quadriceps and hamstring muscle strength within 7 months after ACL reconstruction in amateur male soccer players. Physical Therapy in Sport 40: 10-18.
- Cipriani DJ, Armstrong CW, Gaul S (1995) Backward walking at three levels of treadmill inclination: an electromyographic and kinematic analysis. Journal of Orthopaedic & Sports Physical Therapy 22(3): 95-102.
- Uthoff A, Oliver J, Cronin J, Harrison C, Winwood P (2018) A new direction to athletic performance: Understanding the acute and longitudinal responses to backward running. Sports Medicine 48(5): 1083-1096.
- Uthoff A, Oliver J, Cronin J, Winwood P, Harrison C (2019) Backward Running: The Why and How to Program for Better Athleticism. Strength & Conditioning Journal 41(5): 48-56.
- Sigward SM, Chan MS, Lin PE, Almansouri SY, Pratt KA (2018) Compensatory strategies that reduce knee extensor demand during a bilateral squat change from 3 to 5 months following anterior cruciate ligament reconstruction. journal of orthopaedic & sports physical therapy 48(9): 713-718.
- Labanca L, Laudani L, Menotti F, Rocchi J, Mariani PP, et al. (2016) Asymmetrical lower extremity loading early after anterior cruciate ligament reconstruction is a significant predictor of asymmetrical loading at the time of return to sport. American journal of physical medicine & rehabilitation 95(4): 248-255.
- DiFabio M, Slater LV, Norte G, Goetschius J, Hart JM, et al. (2018) Relationships of functional tests following ACL reconstruction: exploratory factor analyses of the lower extremity assessment protocol. Journal of sport rehabilitation 27(2): 144-150.
- Baumgart C, Schubert M, Hoppe MW, Gokeler A, Freiwald J (2017) Do ground reaction forces during unilateral and bilateral movements exhibit compensation strategies following ACL reconstruction? Knee Surg, Sports Traumatology, Arthrosc 25(5): 1385-1394.
- Alexander Gustavsson, Camille Neeter, Pia Thomeé, Karin Grävare Silbernagel, Jesper Augustsson, et al. (2006) A test battery for evaluating hop performance in patients with an ACL injury and patients who have undergone ACL reconstruction. Knee Surg Sports Traumatology Arthrosc 14(8): 778-788.
- de Fontenay BP, Argaud S, Blache Y, Monteil K (2015) Contralateral limb deficit seven months after ACL-reconstruction: an analysis of single-leg hop tests. The Knee 22(4): 309-312.
- O'Malley E, Richter C, King E, Strike S, Moran K, et al. (2018) Countermovement jump and isokinetic dynamometry as measures of rehabilitation status after anterior cruciate ligament reconstruction. Journal of athletic training 53(7): 687-695.
- Slysz J, Stultz J, Burr JF (2016) The efficacy of blood flow restricted exercise: A systematic review & meta-analysis. Journal of Science and Medicine in Sport/Sports Medicine Australia 19(8): 699-675.
- Brandner CR, May AK, Clarkson MJ, Warmington SA (2018) Reported Side-effects and Safety Considerations for the Use of Blood Flow Restriction During Exercise in Practice and Research 33(2): 1.
- Shad BJ, Thmpson JL, Holwerda AM, Stocks B, Elhassan YS, et al. (2019) One week of Step Reduction Lowers Myofibrillar Protein Synthesis Rates in Young Men. Medicine and Science in Sports and Exercise 51(10): 2125-2134.
- Krogh-Madsen R, Thyfault JP, Broholm C, Mortensen OH, Olsen RH, et al. (2010) A 2-wk reduction of ambulatory activity attenuates peripheral insulin sensitivity. Journal of Applied Physiology 108(5): 1034-1040.
- Grapar Žargi T, Drobnič M, Stražar K, Kacin A (2018) Short–Term Preconditioning with Blood Flow Restricted Exercise Preserves Quadriceps Muscle Endurance in Patients after ACL Reconstruction. Frontiers in Physiology 9: 1150.
- Franz A, Queitsch FP, Behringer M, Mayer C, Krauspe R, et al. (2018) Blood flow restriction training as a prehabilitation concept in total knee arthroplasty: A narrative review about current preoperative interventions and the potential impact of BFR. Medical Hypotheses 110: 53-59.
- Baumgart C, Hoppe MW, Freiwald J (2017) Phase-specific ground reaction force analyses of bilateral and unilateral jumps in patients with ACL reconstruction. Orthopaedic journal of sports medicine 5(6):
- Jordan MJ, Aagaard P, Herzog W (2015) Lower limb asymmetry in mechanical muscle function: A comparison between ski racers with and without ACL reconstruction. Scandinavian journal of medicine & science in sports 25(3): e301-e309.
- Hart LM, Cohen DD, Patterson SD, Springham M, Reynolds J, et al. (2019) Previous injury is associated with heightened countermovement jump force‐time asymmetries in professional soccer players. Translational Sports Medicine 2(5): 256-262.
- Cohen D, Clarke N, Harland S, Lewin C (2014) Are force asymmetries measured in jump tests associated with previous injury in professional footballers? Br J Sports Med 48(7): 579-580.
- Simon AM, Ferris DP (2008) Lower limb force production and bilateral force asymmetries are based on sense of effort. Experimental brain research 187(1): 129-138.
- Chan MS, Sigward SM (2019) Loading Behaviors Do Not Match Loading Abilities Post-anterior Cruciate Ligament Reconstruction. Medicine and science in sports and exercise 51(8): 1626-1634.
- Bishop C, Brashill C, Abbott W, Read P, Lake JP, et al. (2021) Jumping asymmetries are associated with speed, change of direction speed, and jump performance in elite academy soccer players. Journal of strength and conditioning research 35(7): 1841-1847.
- Paterno MV, Ford KR, Myer GD, Heyl R, Hewett TE (2007) Limb asymmetries in landing and jumping 2 years following anterior cruciate ligament reconstruction. Clinical Journal of Sport Medicine 17(4): 258-262.
-
Brian Serrano*. Rehabilitation After Hip Arthroscopy: A Criterion Based Approach. Aca J Spo Sci & Med. 2(2): 2024. AJSSM. MS.ID.000532.
-
Rehabilitation, Hip Arthroscopy, Labral Repair, FAI, Labral Tear, Hip Hypermobility, Physical Activity
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.