Research Article
Research Article
Barefoot Orthotic Allows Barefoot Walking and Running Gait Adaptations
Melissa A Thompson1*, Christopher Bent2, Kelsey Pryor3 and Kristine M Hoffman4
1,2,3Health Sciences Department, Fort Lewis College, Durango, USA
4Department of Orthopedics, Denver Health Medical Center, Denver, CO; Department of Orthopedics, University of Colorado School of Medicine, Aurora, USA
Melissa Thompson, Health Sciences Department, Fort Lewis College, Durango, USA.
Received Date:January 23, 2024; Published Date:February 01, 2024
Use of barefoot orthotic device does not inhibit barefoot walking or running gait adaptations. Foot orthotics are in-shoe devices that aim alter the magnitude and timing of forces that act on the plantar foot to decrease pathologic forces and improve lower extremity function. There are clear benefits of orthotic use in footwear, but also benefits of the barefoot gait. Recently the barefoot orthotic (Stand Strong®) was designed as a modality that allows the benefits of enhanced sensory feedback associated with barefoot gait, while providing the mechanical stability of an orthotic. Gait kinematics and kinetics were analyzed as 12 healthy runners performed 10 over-ground trials of running and walking in running shoes (SHOD), barefoot (BF), and while wearing the barefoot orthotics (BF ORTHO). Kinematic data was obtained with a 3D motion analysis system and was captured in sync with ground reaction force (GRF) data as subjects ran and walked across a runway with embedded force plate. There were no significant differences between the BF and BF ORTHO conditions in terms of walking and running kinematics or kinetics, indicating that the barefoot orthotic does not interfere with the natural barefoot gait. Consistent with previous research, subjects exhibited decreased stride lengths and reduced GRFs in the BF and BF ORTHO conditions when walking and running.
Keywords:Barefoot Walking; Barefoot Running; Orthotic; Gait
Introduction
Numerous pathologies including genetic, traumatic, biomechanical and inflammatory conditions can affect the foot leading to pain and dysfunction. In addition to pain, foot pathologies can have broader implications including gait alteration and functional limitation. Foot pathology can lead to a reduced ability to walk and stand efficiently and effectively. The end result of foot problems can be decreased ability or inability for a person to carry out tasks related to activities of daily living, work and / or recreation.
Foot orthotics are in-shoe medical devices that are designed to alter both the magnitude and timing of forces that act on the plantar foot. These devices aim to improve foot and lower extremity function and decrease pathologic forces that act on the foot and lower extremity [1]. Based on the tissue stress theory, foot orthotics address foot pathomechanics by decreasing pathologic stress to the foot and lower extremity tissues allowing for both injury prevention and rehabilitation of injured tissues [2]. Foot orthotics have been shown to be a successful treatment modality for several lower extremity pathologies including plantar fasciitis [3,4], patellofemoral pain [5], chronic ankle instability [6] and medial knee osteoarthritis [7,8]. Orthotics offer a minimally invasive modality to treat foot pathologies as well as to improve patient function.
While there are clear benefits of orthotic use in footwear, there are also demonstrated benefits of barefoot gait. The barefoot condition has been associated with increased sensory feedback, which leads to gait adaptations that have been shown to have benefits in clinical conditions, as well as resulting in biomechanical alterations that may impact injury prognosis and incidence [9]. In terms of clinical implications, barefoot gait adaptations have been associated with decreased hip and knee loading in osteoarthritis patients [10] and a reduction in lateral ankle sprains [11]. Furthermore, the most consistent gait changes observed with barefoot running are decreased stride length and a fore/mid foot strike pattern [12,13]. Decreasing stride length in running has been shown to reduce ground reaction forces (GRFs) [14,15], joint moments [16], impact accelerations [17], and leg stiffness [18], all factors that have been associated with increased risk of developing overuse injuries. Additionally, barefoot running and minimalist footwear running have been associated with greater activation and strengthening of the intrinsic foot musculature [19,20].
Recently the barefoot orthotic (Hozhoni Balance Rail®, Hozhoni Health Services) was designed as a modality that allows for the benefits of enhanced sensory feedback associated with barefoot gait, but also provides the mechanical stability of an orthotic. The barefoot orthotic attaches to the plantar surface of the foot via a self-adhering, washable material. The design of the Barefoot Orthotic consists of a 1) cuboid pad that stimulates the peroneus longus, helps to plantarflex the first ray and supports the midfoot; 2) balance rail that enhances proprioception and improves pronation and supination misalignments and 3) metatarsal support that decreases loading on the lesser metatarsals (Figure 1). Additionally, the barefoot orthotic is made of a durometer gel material that is stated to provide shock absorption and viscoelastic recoil [21].
Figure 1:Hozhoni Balance Rail® barefoot orthotic.

The development of the barefoot orthotic opens the possibility of maintaining the benefits of the barefoot gait, while allowing for the benefits of orthotic intervention. In order to determine the effectiveness of the barefoot orthotic, it is important to first determine if the barefoot orthotic does or does not interfere with barefoot walking and running adaptations. Therefore, the purpose of the present study was to determine if the commonly observed barefoot gait adaptations were observed in walking and running with the barefoot orthotic.
Methods
Participants: Twelve healthy, physically active, adults participated in this study (7 men and 5 women, age: 25 ± 3.8 yr; height: 1.58 ± 0.15 m; mass: 68.1 ± 8.9 kg). All participants were habitually shod rearfoot strike runners, performed a minimum of 30 minutes of physical activity at least 5 days a week and had no recent or persisting leg or back injuries. The Fort Lewis College Institutional Review Board approved the protocol for this study.
Procedures: Gait kinematics and kinetics were analyzed as participants ran and walked in running shoes (SHOD), barefoot (BF), and while wearing the barefoot orthotics (BF ORTHO). For the SHOD condition participants ran and walked in their personal footwear. All participants ran in traditional running shoes, which was defined as a minimum forefoot stack height 15 mm, rearfoot stack height of 25 mm and 12 mm heel-toe drop. Barefoot orthotics were provided for the BF ORTHO condition, the orthotics were fit and placed according to manufacturer recommendations. Before testing and following a change in footwear (e.g. changing from BF to SHOD), subjects performed a minimum of 5 min of easy running or walking in order to warm up and become familiar with the runway set-up and condition. Subjects were instructed to run and walk in their preferred manner (i.e., self-selected stride length, footstrike position and velocity). Subjects performed 10 trials of walking and 10 trials of running for each footwear condition (SHOD, BF, BF ORTHO). Three strides from each of the ten trials, in which the subject contacted the force plate, were used to calculate participant mean data for each condition. Trials in which velocity or stride length differed by >5% were excluded from analysis.
Kinetics: GRF data was captured as subjects ran over a 20 m runway with a force plate (AMTI, Waterton, MA) located at 15 m. The three orthogonal components of the GRF data [vertical (vGRF), anterior-posterior GRF (apGRF), and medio-lateral GRF (mlGRF)] were captured at 1000 Hz and low-pass filtered at 30 Hz using a second-order Butterworth filter.
Kinematics: Kinematic data was obtained via a 3-dimensional motion analysis system. Participant’s height, weight, leg lengths, and widths of the ankles and knees were measured for appropriate anthropometric scaling. Sixteen retro-reflective markers were attached with double-sided tape to specific anatomical landmarks according to the Modified Helen Hayes Marker Set [22]. Markers were placed bilaterally on the anterior and posterior superior iliac spines, lateral mid-thigh, lateral femoral epicondyle, lateral midshank, lateral malleolus, second metatarsal head and calcaneus. For the SHOD condition, calcaneus and metatarsal head markers were placed on the shoes at the positions overlying the anatomical landmarks. Three-dimensional marker positions were captured at 250 Hz via a Vicon Bonita motion analysis system (Vicon, Oxford Metrics Ltd., UK). Marker trajectory data were filtered via a Woltring filtering routine with predicted mean square error of 4 mm2. Vicon Plug-In Gait was used to calculate 3D joint angles for the ankle, knee and hip. Stride length was measured as the distance between right and left heel marker minima. Velocity was calculated as the average of the anterior superior iliac spine markers horizontal displacement through the capture volume divided by the corresponding time.
Statistical Analysis: Statistical differences in kinetic and kinematic parameters between the SHOD, BF and BF ORTHO conditions for both walking and running were analyzed using repeated measures ANOVA tests conducted in SPSS Version 23 (IBM, Armonk, NY). For significant effects post hoc Bonferroni pairwise, comparisons were performed to determine which conditions were significantly different. Statistical significance was defined as p<0.05.
Results
There were no significant differences between the BF and BF ORTHO conditions in terms of stride length, velocity (Table 1), kinematics (Table 2), or kinetics (Table 3) in either walking or running, indicating that the barefoot orthotic does not interfere with the natural barefoot gait. Consistent with previous research, subjects exhibited decreased stride lengths in the BF and BF ORTHO conditions, as compared to the SHOD condition when walking and running (p = 0.10, Table 1). Velocity did not differ across the three conditions for either walking or running (p = 0.25, Table 1).
The BF and BF ORTHO conditions were associated with reduced peak vGRFs and apGRFs in both walking and running (Table 2). There were no differences in the peak mlGRF across the three conditions for either walking or running (p = 0.31, Table 2). Participants exhibited a more plantarflexed position at ground contact when running in the BF and BF ORTHO conditions, indicating the adoption of a fore/mid foot strike pattern, as compared to SHOD running, which was associated with a heel strike pattern (Table 3). Additionally, when running, participants exhibited greater peak sagittal plane hip angles in the SHOD condition (p = 0.03 vs. BF and p = 0.025 vs BF ORTHO). For walking there were no differences in ankle kinematics at ground contact across the three conditions, with positive values for sagittal plane ankle angle indicating a heel strike pattern in all conditions (p = 0.19, Table 3).
Table 1:Stride length and velocity for walking and running.
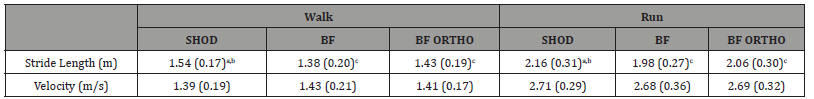
Data are reported as mean (standard deviation). The letter a indicates a significant difference to BF, b indicates a significant difference to BF ORTHO, and c indicates a significant difference to SHOD (p < 0.05).
Table 2:Peak ground reaction forces for walking and running..
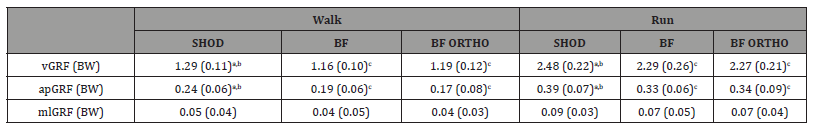
Data are reported as mean (standard deviation). The letter a indicates a significant difference to BF, b indicates a significant difference to BF ORTHO, and c indicates a significant difference to SHOD (p < 0.05). BW = body weight.
Table 3:Lower extremity joint angles at ground contact and peak values for walking and running.
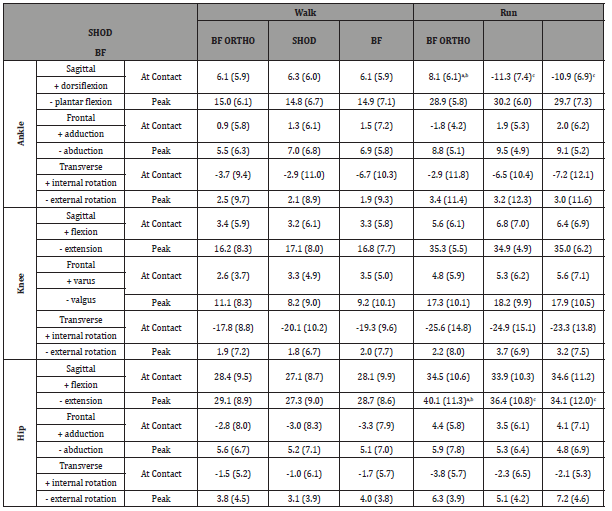
Data are reported as mean (standard deviation). Significant differences are indicated in bold. The letter a indicates a significant difference to BF, b indicates a significant difference to BF ORTHO, and c indicates a significant difference to SHOD (p < 0.05).
Discussion
The aim of this study was to determine if the commonly observed barefoot gait adaptations were also found when walking and running with the barefoot orthotic. We found no difference between the BF and BF ORTHO conditions in terms of gait kinematics or kinetics in both walking and running, which suggests that the barefoot orthotic does not interfere with barefoot gait adaptations. We did observe significant differences between both the BF and BF ORTHO conditions and the SHOD condition in terms of stride length and GRFs for both walking and running. Further, when running in the SHOD condition, participants exhibited greater peak hip extension, which is likely associated with the longer stride length in the SHOD condition. These results are consistent with previous research comparing barefoot and shod running and walking that have shown that the barefoot condition results in reduced stride length [23]. Our finding of a more plantar flexed position at ground contact when running in the BF and BF ORTHO conditions also agrees with previous literature [24]. However, contrary to previous research [25-28], we did not observe a significant change in ankle joint plantarflexion at ground contact when walking in the BF and BF ORTHO conditions.
The design of the barefoot orthotic allows for cutaneous sensory feedback from the toes, midfoot and heel, which allows for sensorytriggered barefoot gait adaptations. Compared to barefoot running, shod running is thought to decrease cutaneous feedback from the plantar surface of the foot [29] resulting in increased stride length and a rearfoot strike gait pattern at heel contact [30]. The enhanced sensory feedback associated with barefoot running has been found to promote a mid/fore foot strike gait pattern, which is thought to result in a shorter stride length and reduced impact loading [30,31]. The similar gait adaptations of reduced stride length [23,32-34], and a plantarflexed ankle position at ground contact [25-28] that are observed in barefoot walking, suggests that these alterations are also sensory mediated. The results of the present study show that the barefoot gait adaptations remain when walking or running with the barefoot orthotic, which indicates that the orthotic does not interfere with the natural barefoot gait. Thus, the barefoot orthotic has the potential to provide therapeutic benefits of an orthotic, while at the same time allowing for the sensory-triggered adaptations associated with the barefoot gait.
The gait adaptations that occurred with both the BF and BF ORTHO conditions may have implications for injury. Specifically, the barefoot orthotic was associated with a more plantarflexed foot position at ground contact in running, which may be associated with a lower incidence of running related injuries. Up to 89% of runners wearing traditional running shoes, which include a cushioned and elevated heel, land with a rearfoot strike [12, 13], while most barefoot runners land with a fore/mid foot strike pattern [12,13]. A rearfoot strike gait has been associated with higher injury rates in runners [35], whereas there is evidence to suggest that adopting a forefoot strike gait pattern has the potential to lower injury risk [36]. Further, several studies have found increased impact loading to be associated with common running injuries [37-39]. Although impact loading was not evaluated in the present study, the finding that barefoot gait adaptations remained in the BF ORTHO condition is highly suggestive that use of the barefoot orthotic would reduce impact loading.
Orthotics are historically an in-shoe medical device that works by controlling abnormal foot mechanics in order to treat or prevent musculoskeletal injuries. The barefoot orthotic takes a novel approach toward orthotic use by adhering to the bottom of the foot. This innovative approach allows for the orthotic to be used in different types of footwear or even while barefoot. While the effectiveness of the barefoot orthotic to treat pathological conditions of the foot was not evaluated in the present study, previous research has shown that foot orthotics function by improving dynamic stability of the foot and reducing abnormal pronation during the stance phase of gait. Orthotics have been shown to evoke numerous gait changes in both running and walking. For running, orthotic use has been shown to reduce abnormal pronation [40-43], with decreases seen in both the maximum pronation angle and the time period of pronation [42]. Additional gait changes seen with orthotic use in running decreased maximum ankle dorsiflexion and knee flexion during stance [40]. In terms of walking, orthotics have been shown to reduce the degree of pronation throughout stance and increase the duration of stance time [44]. The barefoot orthotic may be able to capitalize on these benefits without requiring footwear or limiting footwear options.
Shoe gear constraints can limit orthotic use and also prevent orthotic users from gaining any of the benefits of barefoot gait. The results of this study show that the barefoot orthotic does not inhibit barefoot gait adaptations, allowing users to gain a forefoot strike pattern with shorter stride length and reduced GRFs, while at the same time potentially affording the stabilizing and pronation control benefits of an orthotic. The technology by which the barefoot orthotic adheres to the bottom of the foot could serve as a base for attaching any type of orthotic to the foot. This approach could greatly improve patient compliance as patients are not restricted to a specific type of footwear and can even use the orthotics while barefoot.
The present study had several limitations. First, the testing session of the present study was relatively short, and participants did not continuously walk or run throughout the entire testing session. Additionally, the trials were completed at a low intensity so there was little perspiration. Future research should evaluate the effectiveness of the barefoot orthotic for long-term use, particularly at an intensity that results in perspiration as this may interfere with skin adhesion. The present study aimed to simply determine if the barefoot orthotic impeded the natural barefoot gait, whereas orthotics are used as a treatment for clinical conditions. Thus, future research should examine the effectiveness of the barefoot orthotic in the treatment of clinical conditions of the foot and ankle. Lastly, we examined the similarity to the barefoot condition, but the barefoot orthotic also allows for novel application in non-supportive shoe gear such as sandals. Further research is needed to determine the effectiveness of the barefoot orthotic in such footwear.
Conclusion
In conclusion, barefoot gait adaptations remain with use of the barefoot orthotic, indicating that it does not interfere with the natural barefoot gait. Thus, the barefoot orthotic has the potential for clinical use while barefoot or without supportive footwear. Additionally, the skin-adhering property of the barefoot orthotic could serve as a basis for attaching any type of orthotic to the plantar surface of the foot.
Acknowledgement
The authors would like to thank Gregory Stillwell, DPM for providing the barefoot orthotics for this study.
Conflict of interest
No Conflict of interest.
References
- Kirby K (2010) Evolution of Foot Orthoses in Sports. In M. K. Werd, EL (Ed.), Athletic Footwear and Orthoses in Sports Medicine pp: 19-35.
- Fuller EA, Kevin AK (2013) Subtalar joint equilibrium and tissue stress approach to biomechanical therapy of the foot and lower extremity. S Albert, Curran SA (Ed.), Biomechanics of the Lower Extremity: Theory and Practice pp: 205-264.
- Lewis RD, Wright P, McCarthy LH (2015) Orthotics Compared to Conventional Therapy and Other Non-Surgical Treatments for Plantar Fasciitis. J Okla State Med Assoc 108(12): 596-598.
- Sinclair J, Isherwood J, Taylor PJ (2015) The effects of orthotic intervention on multisegment foot kinematics and plantar fascia strain in recreational runners. J Appl Biomech 31(1): 28-34.
- Waddington GS (2018) Foot exercise and orthotics more effective than knee exercise in PFJ pain. J Sci Med Sport 21(1): 1.
- Gabriner ML, Braun BA, Houston MN, Hoch MC (2015) The effectiveness of foot orthotics in improving postural control in individuals with chronic ankle instability: a critically appraised topic. J Sport Rehabil, 24(1): 68-71.
- Fantini Pagani CH, Willwacher S, Benker R, Bruggemann GP (2014) Effect of an ankle-foot orthosis on knee joint mechanics: a novel conservative treatment for knee osteoarthritis. Prosthet Orthot Int 38(6): 481-491.
- Fu HC, Lie CW, Ng TP, Chen KW, Tse CY, et al. (2015) Prospective study on the effects of orthotic treatment for medial knee osteoarthritis in Chinese patients: clinical outcome and gait analysis. Hong Kong Med J 21(2): 98-106.
- Robbins SE, Hanna AM (1987) Running-related injury prevention through barefoot adaptations. Med Sci Sports Exerc 19(2): 148-156.
- Shakoor N, Block JA (2006) Walking barefoot decreases loading on the lower extremity joints in knee osteoarthritis. Arthritis Rheum 54(9): 2923-2927.
- Robbins S, Waked E (1998) Factors associated with ankle injuries. Preventive measures. Sports Med 25(1): 63-72.
- Lieberman DE, Venkadesan M, Werbel WA, Daoud AI, D'Andrea S, et al. (2010) Foot strike patterns and collision forces in habitually barefoot versus shod runners. Nature 463(7280): 531-535.
- Squadrone R, Gallozzi C (2009) Biomechanical and physiological comparison of barefoot and two shod conditions in experienced barefoot runners. J Sports Med Phys Fitness 49(1): 6-13.
- Divert C, Baur H, Mornieux G, Mayer F, Belli A, et al. (2005) Stiffness adaptations in shod running. J Appl Biomech 21(4): 311-321.
- Divert C, Mornieux G, Baur H, Mayer F, Belli A, et al. (2005) Mechanical comparison of barefoot and shod running. Int J Sports Med 26(7): 593-598.
- Kerrigan DC, Franz JR, Keenan GS, Dicharry J, Della Croce U, et al. (2009) The effect of running shoes on lower extremity joint torques. PM R 1(12): 1058-1063.
- Thompson M, Seegmiller J, McGowan CP (2016) Impact Accelerations of Barefoot and Shod Running. Int J Sports Med 37(5): 364-368.
- Bishop M, Fiolkowski P, Conrad B, Brunt D, Horodyski M, et al. (2006) Athletic footwear, leg stiffness, and running kinematics. J Athl Train 41(4): 387-392.
- Johnson AW, Myrer JW, Mitchell UH, Hunter I, Ridge ST, et al. (2016) The Effects of a Transition to Minimalist Shoe Running on Intrinsic Foot Muscle Size. Int J Sports Med 37(2): 154-158.
- Miller EE, Whitcome KK, Lieberman DE, Norton HL, Dyer RE, et al. (2014) The effect of minimal shoes on arch structure and intrinsic foot muscle strength. J Sport Health Sci 3(2): 74-85.
- (2018) Hozhoni Balance Rail.
- Kadaba MP, Ramakrishnan HK, Wootten ME (1990) Measurement of lower extremity kinematics during level walking. J Orthop Res 8(3): 383-392.
- Franklin S, Grey MJ, Heneghan N, Bowen L, Li FX, et al. (2015) Barefoot vs common footwear: A systematic review of the kinematic, kinetic and muscle activity differences during walking. Gait Posture 42(3): 230-239.
- Jenkins DW, Cauthon DJ (2011) Barefoot running claims and controversies: a review of the literature. J Am Podiatr Med Assoc 101(3): 231-246.
- Chard A, Greene A, Hunt A, Vanwanseele B, Smith R, et al. (2013) Effect of thong style flip-flops on children's barefoot walking and jogging kinematics. J Foot Ankle Res 6(1): 8.
- Morio C, Lake MJ, Gueguen N, Rao G, Baly L, et al. (2009) The influence of footwear on foot motion during walking and running. J Biomech 42(13): 2081-2088.
- Oeffinger D, Brauch B, Cranfill S, Hisle C, Wynn C, et al. (1999) Comparison of gait with and without shoes in children. Gait Posture 9(2): 95-100.
- Zhang X, Paquette MR, Zhang S (2013) A comparison of gait biomechanics of flip-flops, sandals, barefoot and shoes. J Foot Ankle Res 6(1): 45.
- Robbins S, Hanna A, Jones L (1988) Sensory attenuation induced by modern athletic footwear. J Test Eval 16(4): 412-416.
- Altman AR, Davis IS (2012) Barefoot running: biomechanics and implications for running injuries. Curr Sports Med Rep 11(5): 244-250.
- Thompson M, Hoffman K (2016) Cutaneous Sensory Feedback is a Primary Determinant of Gait Changes Observed in Barefoot Running. Paper presented at the American Society of Biomechanics Annual Meeting, Raleigh NC.
- Lythgo N, Wilson C, Galea M (2009) Basic gait and symmetry measures for primary school-aged children and young adults whilst walking barefoot and with shoes. Gait Posture 30(4): 502-506.
- Moreno-Hernandez A, Rodriguez-Reyes G, Quinones-Uriostegui I, Nunez-Carrera L, Perez-Sanpablo AI, et al. (2010) Temporal and spatial gait parameters analysis in non-pathological Mexican children. Gait Posture 32(1): 78-81.
- Wolf S, Simon J, Patikas D, Schuster W, Armbrust P, et al. (2008) Foot motion in children shoes: a comparison of barefoot walking with shod walking in conventional and flexible shoes. Gait Posture 27(1): 51-59.
- Daoud AI, Geissler GJ, Wang F, Saretsky J, Daoud YA, et al. (2012) Foot strike and injury rates in endurance runners: a retrospective study. Med Sci Sports Exerc 44(7): 1325-1334.
- Davis IS, Rice HA, Wearing SC (2017) Why forefoot striking in minimal shoes might positively change the course of running injuries. J Sport Health 6(2): 154-161.
- Milner CE, Ferber R, Pollard CD, Hamill J, Davis IS, et al. (2006) Biomechanical factors associated with tibial stress fracture in female runners. Med Sci Sports Exerc 38(2): 323-328.
- Pohl MB, Hamill J, Davis IS (2009) Biomechanical and anatomic factors associated with a history of plantar fasciitis in female runners. Clin J Sport Med 19(5): 372-376.
- Pohl MB, Mullineaux DR, Milner CE, Hamill J, Davis IS, et al. (2008) Biomechanical predictors of retrospective tibial stress fractures in runners. J Biomech 41(6): 1160-1165.
- Bates BT, Osternig LR, Mason B, James LS (1979) Foot orthotic devices to modify selected aspects of lower extremity mechanics. Am J Sports Med 7(6): 338-342.
- Donatelli RA, Hurlburt C, Conaway D, St Pierre R (1988) Biomechanical foot orthotics: a retrospective study. J Orthop Sports Phys Ther 10(6): 205-212.
- Rodgers MM, Leveau BF (1982) Effectiveness of foot orthotic devices used to modify pronation in runners*. J Orthop Sports Phys Ther 4(2): 86-90.
- Smith LS, Clarke TE, Hamill CL, Santopietro F (1986) The effects of soft and semi-rigid orthoses upon rearfoot movement in running. J Am Podiatr Med Assoc 76(4): 227-233.
- McCulloch MU, Brunt D, Vander Linden D (1993) The effect of foot orthotics and gait velocity on lower limb kinematics and temporal events of stance. J Orthop Sports Phys Ther 17(1): 2-10.
-
Melissa A Thompson*, Christopher Bent, Kelsey Pryor and Kristine M Hoffman. Barefoot Orthotic Allows Barefoot Walking and Running Gait Adaptations. Aca J Spo Sci & Med. 1(4): 2024. AJSSM.MS.ID.000520.
-
Barefoot Orthotic, Barefoot Walking, Gait Adaptations, Traumatic, Medial Knee Osteoarthritis, Musculoskeletal Injuries
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
- Abstract
- Introduction
- Materials and Methods
- The Basic Tools of Scientific Inquiry
- Literature Review
- Theoretical Framework
- Research Design
- Findings and Discussion
- Conclusion and Recommendations
- Based on the findings, the following recommendations are considered:
- Declaration Statements
- Funding
- Data Availability Statement (DAS)
- Compliance with Ethical Standards
- Acknowledgement
- Conflict of Interest
- References