 Case Report
Case Report
Weight Regain after Bariatric Surgery - Argon Plasma Coagulation for Gastrojejunal Anastomosis Decrease
BQ Sander1*, EP Silva2, SR Farfan3, LD Conceição4, SG Godinho5, WCC Vieira6, FMB Pires7, HG Sampaio8, JR Pereira9 and LR Alberti10
1Sander Medical Center, Brazil
2Hospital of Portela, Brazil
3Hospital of Santa Rosália, Brazil
4HC de Alagoinhas, Brazil
5Hospital of Imaculada Conceição, Brazil
6Clínica AMA, Brazil
7Tower Center, Brazil
8HapClínica Pituba, Brazil
9GV Clínicas, Brazil
10HC-UFMG, Brazil
BQ Sander, Sander Medical Center, Brazil.
Received Date: January 24, 2020; Published Date: February 07, 2020
Introduction
The weight regained has been a described growing problem in patients after bariatric surgery, especially at long term. This weight regained is multifactorial and often associated with dilation of Gastrojejunostomy (GJ), allowing a faster gastric emptying and therefore greater food intake [1,2]. For the patients with significant weight regain after failed conservative approach, some revisional procedures had be attempted and more recently endoscopic revisional procedures had being described [3,4].
Aims and Methods
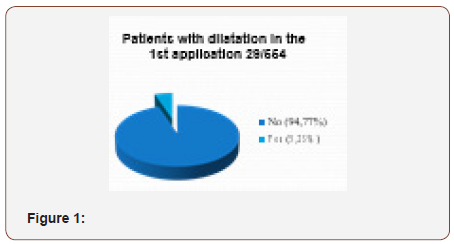
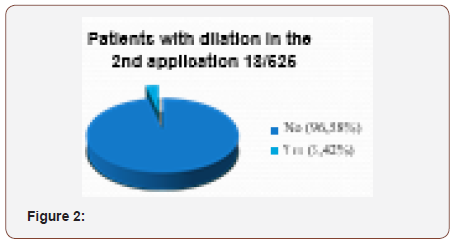
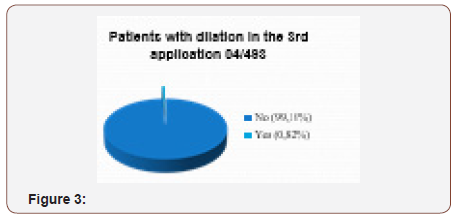
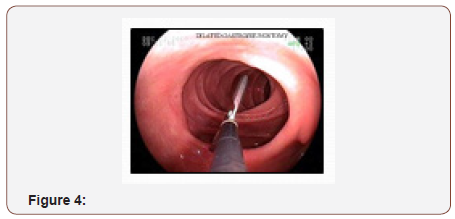
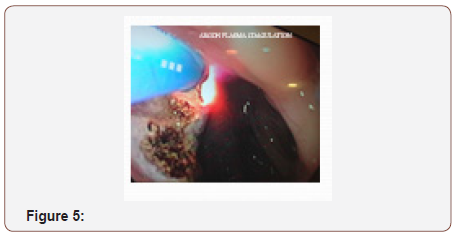
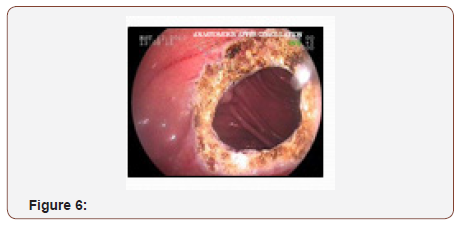
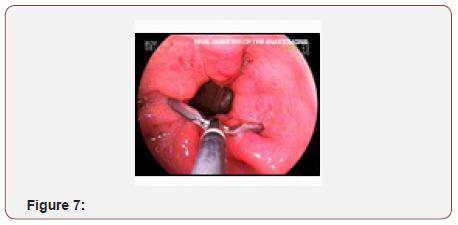
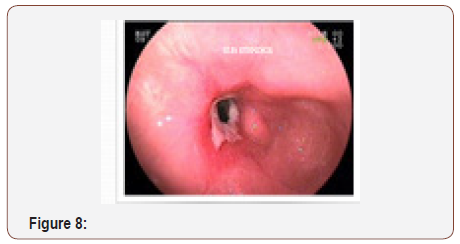
To evaluate the safety and effectiveness of Argon Plasma Coagulation (APC) decreasing the diameter of the gastroenteric anastomosis in patients who have undergone RYGB for morbid obesity and regained weight associated to dilation of the GJ From Jan-2014 to April-2017 554 RYGB subjects with weight regain a dilated anastomosis (>18mm) and at least 2 years from procedure were submitted APC application [5-7]. In relation to the anastomotic diameter, the majority of studies use a diameter of more than 20 mm to define anastomosis dilation, although some studies use smaller diameters such as 12 mm, similar to that created manually in the gastrojejunal anastomosis using a 36 Fr Fouchet bougie [8,9]. In the patients in the present study, the minimum cross-section diameter was 18 mm and the maximum measured in the first session 40 mm [10]. This anastomotic diameter was measured using a 33-mm long Olympus® articulated device [11]. Interval between an APC session was 60 days with a maximum of 03 applications. APC set was at 2-3L/m with 65-85W. GJ diameter target was 8-12mm estimated with pre-measured grasper [12-14]. At first APC session, preop weight and BMI, post-op weight nadir, actual weight and BMI and estimated diameter of GJ were the variables collected [15,16]. Complications during treatment were also collected. In the present study, psychological and nutritional evaluations were performed before APC and during treatment and physical activity was strongly recommended [17,18]. Data were analyzed with descriptive statistics, student’s t test and Spearman correlation [19,20] (Figure 1-10).

Results
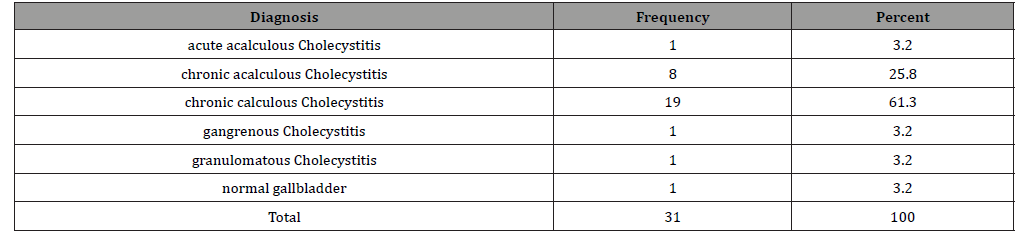
Of the 554 patients, 79.06% were women and 20.94% were men. Average time between bariatric surgery and the first APC was 96.35 months (±42.17) and average weight regained in this interval was 22,08kg (±11,05) [21-23]. The mean diameter of the anastomosis was 24.78mm (±6,04) and the average number of APC sessions were 1.78 times (±0,61). The average reduction of anastomotic diameter was 14.86mm (±7,24) and the final average diameter was 11,79mm (±3,89) [24,25]. The average weight loss between the first and last APC was 13,37kg (±7,82) and the average decrease of BMI was 4,59kg/m2 (±2,78). 122 patients (22,02%) did not achieve the target GJ diameter and 05 patient (0,9%) did not lose weight even with the desired GJ diameter [26-29]. From the 146 subjects (26,36%) followed up to 12 months, the weight regain was less than 20% of the weight loss. Of the 554 patients APC, 51 (9,2%) required dilatation balloon due to symptomatic stenosis at least once (Table 1).
Table 1:
Conclusion
Argon Plasma Coagulation (APC) has been shown to be an effective and safe endoscopic technique for the reduction of gastro enteric anastomosis in patients undergoing bariatric surgery who have regained weight with dilation of the anastomosis. The reintroduction of the patient to the multisciplinary team is mandatory in cases of weight regain and loss to postoperative followup. A psychological and/or psychiatric evaluation is mandatory, as well as nutritional therapy and encouragement of physical activity. The monitoring of food intake and body weight, closer follow up of the operated patients, appropriate choice of technique according to the patient and the experience of the surgeon, and a good learning curve are all factors that can reduce the failure rate of bariatric surgery. The reintroduction of the patient to the multidisciplinary team is mandatory if better results and sustainable weight loss and comorbidity control are to be obtained.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Barhouch AS, Zardo M, Padoin AV, Colossi FG, Casagrande DS, et al. (2010) Excess Weight Loss Variation in Late Postoperative Period of Gastric Bypass. Obes Surg 20(11): 1479-1483.
- Christou N, Look D, Maclean L (2006) Weight Gain After Short and Long-Limb Gastric Bypass in Patients Followed for Longer Than 10 Years. Ann Surg 244(5): 734-740.
- Prachand V, DaVee R, Alverdy J (2006) Duodenal-Switch Provides Superior Weight Loss in the Super-Obese (BMI > 50Kg/m2) Compared with Gastric Bypass. Ann Surg 244(4): 611-619.
- Himpens J, Coromina L, Verbrugghe A, Cadiere GB (2012) Outcomes of Revisional Procedures for Insufficient Weight Loss or Weight Regain after Roux-En-Y Gastric Bypass. Obes Surg 22(11): 1746-1754.
- Spaulding L (2003) Treatment of dilated gastrojejunostomy with sclerotherapy. Obes Surg 13(2): 254-257.
- Thompson CC, Slattery J, Bundga ME, Lautz DB (2006) Peroral endoscopic reduction of dilated gastrojejunal anastomosis after Roux-en-Y gastric bypass: a possible new option for patients with weight regain. Surg Endosc 20(11): 1744-1748.
- Mikami D, Needleman B, Narula V, Durant J, Melvin WS (2010) Natural orifice surgery: initial US experience utilizing the Stomaphyx device to reduce gastric pouches after Roux-en-Y gastric bypass. Surg Endosc 24(1): 223-228.
- Horgan S, Jacobsen G, Weiss D, Oldham JS, Denk PM, et al. (2010) Incisionless revision of post-Roux-en-Y bypass stomal and pouch dilation: multicenter registry results. Surg Obes Relat Dis 6(3): 290-295.
- Galvão Neto M, Rodriguez L, Zundel N (2011) Endoscopic revision of Roux-en-Y gastric bypass stomal dilation with a suturing device: preliminary results of a first out-of-United States series. Bariatric Times 8: 1-34.
- Heylen AMF, Jacobs A, Lybeer M, Prosst RL (2011) The OTSC – Clip in Revisional Endoscopy Against Weight Gain After Bariatric Gastric Bypass Surgery. Obes Surg 21(10): 1629-1633.
- Aly A (2009) Argon Plasma Coagulation and Gastric Bypass – A Novel Solution to Stomal Dilation. Obes Surg 19(6): 788-790.
- Baretta GAP, Alhinho HCAW, Matias JEF (2015) Argon Plasma Coagulation of Gastrojejunal Anastomosis for Weight Regain After Gastric Bypass. Obes Surg 25: 72-79.
- Grund KE, Storek D, Farin G (1994) Endoscopic argon plasma coagulation (APC) first clinical experiences in flexible endoscopy. Endosc Surg Allied Technol 2(1): 42-46.
- Dotti VP, Baretta GAP, Yoshii SO, Ivano FH, Ribeiro HDW, et al. (2009) Endoscopic argon plasma thermo-coagulation of Barrett’s esophagus using different powers: Histopathological and post procedure symptons analysis. Rev Col Bras Cir 36 (2): 110-117.
- Brethauer SA, Nfonsam V, Sherman V, Udomsawaengsup S, Schauer PR, et al. (2006) Endoscopy and upper gastrointestinal contrast studies are complementary in evaluation of weight regain after bariatric surgery. Surg Obes Relat Dis 2(6):643-648.
- ASGE/ASMBS Task Force on Endoscopic Bariatric Therapy (2011) A pathway to endoscopic therapies. Surg Obes Relat Dis 7(6): 672-82.
- Henegan HM, Yimcharoen P, Brethauer SA, Kroh M, Chand B (2012) Influence of pouch and stoma size on weight loss after gastric bypass. Surg Obes Relat Dis 8(4): 408-415.
- Abu Dayyeh BK, Lautz DB, Thompson CC (2011) Gastrojejunal stoma diameter predicts weight regain after Roux-en-Y gastric bypass. Clin Gastroenterol Hepatol 9(3): 228-33.
- Malick KJ (2006) Clinical applications of argon plasma coagulation in endoscopy. Gastroenterol Nurs 29(5): 392-393.
- Storek D Grund KE, Gronbach G, Farin G, Becker HD (1993) Endoscopic argon gas coagulation – Initial clinical experience. Z Gastroenterol 31(11): 675-679.
- Garrido T (2002) Análise histopatológica do efeito da eletrocoagulação bipolar e da aplicação de plasma de argônio em espécimes cirúrgicos do trato digestó ABCD Arq Bras Cir Dig 15 (2): 116-120.
- Pinotti AC, Cecconello I, Filho FM, Sakai P, Gama-Rodrigues JJ, et al. (2004) Endoscopic ablation of Barrett’s esophagus using argon plasma coagulation: A prospective study after fundoplication. Dis Esophagus 17(3): 243-246.
- Dayyeh BKA, Jirapinyo P, Weitzner Z, Barker C, Flicker M, et al. (2012) Endoscopic sclerotherapy for the treatment of weight regain after Roux-en-Y gastric bypass: outcomes, complications and predictors of response in 575 procedures. Gastroint Endosc 76(2): 275-282.
- Catalano MF, Rudic R, Anderson AJ, Chua TY (2007) Weight gain after bariatric surgery as a result of a large gastric stoma: endotherapy with sodium morrhuate may prevent the need for surgical revision. Gastroint Endosc 66(2): 240-247.
- Thompson CC, Jacobsen GR, Schroder GL, Horgan S (2012) Stoma size critical to 12-month outcomes in endoscopic suturing for gastric bypass repair. Surg Obes Relat Dis 8(3): 282-287.
- Kumar N, Thompson CC (2014) Comparison of a superficial suturing device with a full-thickness suturing device for transoral outlet reduction. Gastrointest Endosc 79(6): 984-989.
- Herron DM, Birkett DH, Thompson CC, Bessler M, Swanstrom LL (2008) Gastric bypass pouch and stoma reduction using a transoral endoscopic anchor placement system: a feasibility study. Surg Endosc 22(4):1093-1099.
- Yimcharoen P, Heneghan HM, Singh M, Brethauer S, Schauer P, et al. (2011) Endoscopic findings and outcomes of revisional procedures for patients with weight regain recidivism after gastric bypass. Surg Endosc 25(10): 3345-3352.
- Dakin GF, Eid G, Mikami D (2013) AACE / TOS / ASMBS Guidelines. Endoluminal revision of gastric bypass for weight regain – a systematic review. Surg Obes Relat Dis 9: 335-343.
-
BQ Sander, EP Silva, SR Farfan, LD Conceição, SG Godinho, et al. Weight Regain after Bariatric Surgery - Argon Plasma Coagulation for Gastrojejunal Anastomosis Decrease. Acad J Gastroenterol & Hepatol. 1(5): 2020. AJGH.MS.ID.000522.
-
Bariatric Surgery, Gastrojejunal, Endoscopic, Psychological, Symptomatic stenosis, Argon plasma coagulation, Anastomosis decrease
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






