 Case Report
Case Report
Tia Leading to the Diagnosis Amelanotic Metastatic Gastric Melanoma
Shaheer Siddiqui1, Tarun Jain2, Zhenjian Cai3 and Scott Larson4*
1Department of Gastroenterology & Hepatology, University of Texas, McGovern School of Medicine, USA
2Department of Resident Internal Medicine, University of Texas, McGovern School of Medicine, USA
3Department of Assistant Professor Pathology, University of Texas, McGovern School of Medicine, USA
4Department of Assistant Professor Gastroenterology &Hepatology, University of Texas, McGovern School of Medicine, USA
Scott Larson, Department of Assistant Professor Gastroenterology &Hepatology, LBJ General Hospital, University of Texas, McGovern School of Medicine, USA.
Received Date: August 07, 2019; Published Date: August 13, 2019
Abstract
Melanoma metastatic to the GI tract is a rare disease. Due to hematogenous spread it usually presents as multiple pigmented lesions in the GI tract. We present a case of a 62 years old gentleman diagnosed with melanoma presenting to the hospital with GI bleed and severe anemia. Endoscopic evaluation revealed a large gastric polypoid mass which proved to be a metastatic melanoma diagnosed 39 months after the initial diagnosis of primary melanoma. The rare presentation of our case is the amelanotic nature of the metastatic melanoma appearing as a gastric mass.
Introduction
The GI tract is one of the most common sites of metastasis of malignant melanoma and can present as an initial diagnosis or discovered years after the initial diagnosis [1]. Only 4% of the patient population with malignant melanoma will have GI involvement during their lives otherwise 60% of metastatic melanomas to the GI tract are discovered postmortem [2]. Amongst all the metastatic sites of the melanoma secondary gastric lesions are only reported to be between 0.2% to 1.7% [3,4, 5].
Case Report
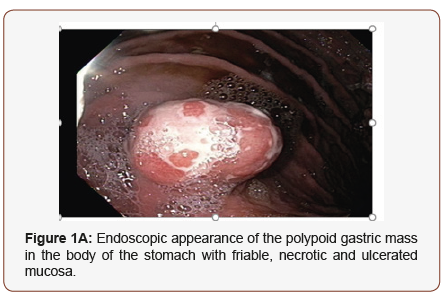
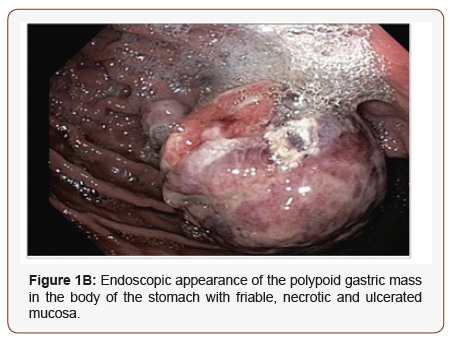
We are presenting a case of a 62 years old gentleman who was initially diagnosed with metastatic melanoma stage IIIb in 4/2015 and underwent wide local excision. Biopsy results revealed negative margins. No nodal metastasis was noted. Because of localized disease the patient underwent radiation therapy that was completed in 7/2015. Patient had a close follow up with oncology and after undergoing comprehensive physical examination, laboratory studies and imaging it was revealed that patient had no evidence of disease. In January of 2018 patient developed a subcutaneous nodule in the left flank area which was biopsied but was negative for malignancy. Patient underwent a CT scan of chest, abdomen and pelvis and PET scan in 2/2018 to look for metastatic disease but did not reveal any significant findings. In 4/2018 patient suffered a stroke and was started on dual antiplatelet therapy. After few months the patient started feeling extremely week and fatigued complaining of having black tarry stools. In 7/2018 patient visited his PCP for evaluation and was found to have severe anemia with a hemoglobin of 4.5 g/dL. Patient was referred to the emergency room for further evaluation. Patient was admitted under the service of Internal Medicine and underwent blood transfusions. Patients anti platelet therapy was put on hold. Gastroenterology was consulted as there was a high suspicion of an upper GI bleed. An EGD revealed a large 6 cm polypoid gastric mass with one satellite lesion with extremely friable, necrotic and ulcerated mucosa (Figure 1A and 1B). Gastric mass was not removed because of the large size and also increased risk of bleeding. A hot snare was used for tissue acquisition which was sent to pathology.
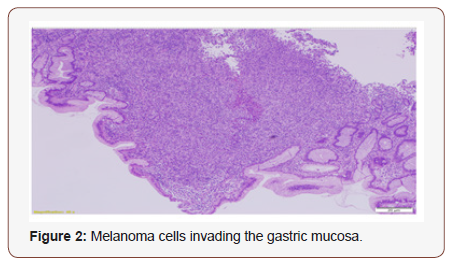
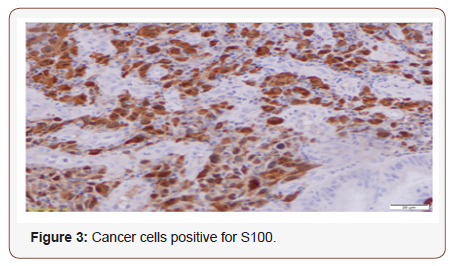
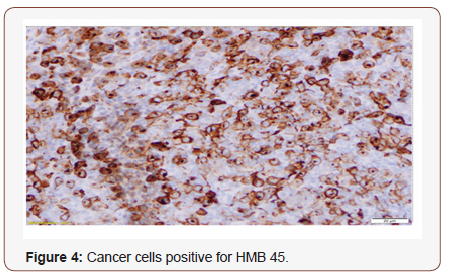
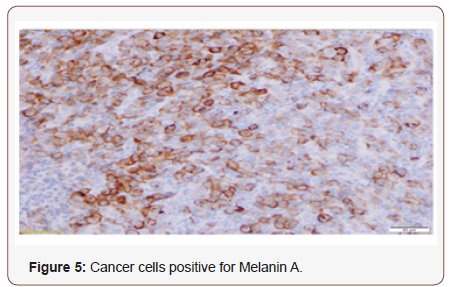
Pathology revealed tumor cells (Figure 2) positive for S100 (Figure 3), HMB45 (Figure 4), and Melanin A (Figure 5), negative for AE1/AE3 and CD34, findings consistent with melanoma. Patient was subsequently referred to oncology for further management. The patient was scheduled to undergo partial gastrectomy, but patient did not follow up for surgical procedure. As the patient did not follow up for surgery, patient was initiated on immune therapy with Nivolumab and Ipilimumab.
Discussion
Amelanotic malignant melanoma accounts for only 2 % of melanomas and metastasis to the stomach is extremely rare [6]. Melanoma of the stomach usually presents with nonspecific symptoms of epigastric pain, nausea, vomiting and abdominal fulness. Melanoma presenting as GI bleed or anemia is an unusual presentation [1, 7]. Our patient presented with severe anemia probably secondary to oozing from the tumor in light of the fact that patient was initiated on dual antiplatelet therapy due to stroke. If it was not for severe anemia and presentation to the hospital, the diagnosis would have been difficult. Also, patient did not complain of having any overt signs of bleeding. Gilg et al. in 2018 noted that metastatic malignant melanoma spreading to the GI tract usually presents as multiple lesions due to hematogenous spread of the disease [8]. Also, amelanotic malignant melanoma present as greyish to whitish lesions that are difficult to differentiate from Gastrointestinal stromal tumors and primary gastric tumors and the diagnosis is made histologically [6]. The presentation of the disease in our patient was a large polypoid necrotic mass instead of multiple lesions and on initial endoscopic evaluation appeared as primary gastric cancer. It was not until the pathology results confirmed the diagnosis of malignant melanoma. Most of the secondary tumors are classified as submucosa type or primary carcinoma type [9]. The endoscopic feature of amelanotic melanoma in our patient did not fit either of the common classification type. Gilg et al. in 2018 also mentioned that it took a mean of 31 months for the secondary tumors to get diagnosed [8]. Our patient got diagnosed with gastric melanoma as a secondary tumor in 39 months after the initial diagnosis of cutaneous melanoma. From no disease on a PET scan to large polypoid gastric mass within 6 months shows an extremely rapid progression of the disease process.
Any patient diagnosed with cutaneous melanoma in the past presenting with nonspecific GI symptoms including GI bleed and anemia of unknown etiology should raise concerns about metastatic melanoma to the GI tract. Prompt evaluation, endoscopic and histological diagnosis is extremely important in formulating a treatment plan for better outcomes as malignant metastatic melanomas represents a poor overall prognosis.
Conclusion
Our case presents a very rapid progression of the melanoma from apparently no disease to finding of metastatic melanoma presenting as upper GI bleed with discovery of large polypoid gastric mass within six months. The most interesting aspect of our case is amelanotic nature of the gastric mass. On initial endoscopic evaluation it appeared as a gastric polyp and it was the biopsy that proved the gastric mass as malignant melanoma. We might not have even discovered the gastric melanoma if the patient did not present with upper GI bleed which was probably due to initiation of dual anti platelet therapy and oozing of blood form the friable mucosa. Hence the diagnosis of amelanotic malignant melanoma presenting as large polypoid gastric mass which in itself is a rare entity.
Acknowledgment
None.
Conflict of Interest
No Conflict of Interest.
References
- Köklü S, Gültuna S, Yüksel I, Başar Ö, Üsküdar O, et al. (2008) Diffuse Gastroduodenal Metastasis of Conjunctival Malignant Melanoma. The American Journal of Gastroenterology 103(5): 1321-1323.
- Patel JK, Didolkar MS, Pickren JW, Moore RH (1978) Metastatic pattern of malignant melanoma: a study of 216 autopsy cases. The American Journal of Surgery 135(6): 807-810.
- Menuck LS, Amberg JR (1975) Metastatic disease involving the stomach. The American Journal of Digestive Diseases 20(10): 903-913.
- Ga Hee Kim, Ji Yong Ahn, Hwoon-Yong Jung, Young Soo Park, Min Ju Kim, et al. (2015) Clinical and Endoscopic Features of Metastatic Tumors in the Stomach. Gut and Liver 9(5): 615-622.
- Zhao HD, Wang G, Wang T, Liang X, Zhou L, et al. (2014) Gastrointestinal tract metastasis from tubulolobular carcinoma of the breast: a case report and review of the literature. OncoTargets and Therapy 7: 435- 440.
- Suganuma T, Fujisaki J, Hirasawa T, Ishiyama A, Yamamoto Y, et al. (2013) Primary amelanotic malignant melanoma of the small intestine diagnosed by esophagogastroduodenoscopy before surgical resection. Clinical Journal of Gastroenterology 6(3): 211-216.
- Reintgen DS, Thompson W, Garbutt J, Seigler HF (1984) Radiologic, endoscopic, and surgical considerations of melanoma metastatic to the gastrointestinal tract. Plastic and Reconstructive Surgery 75(4): 95(6): 635-639.
- Gilg MM, Gröchenig HP, Schlemmer A, Eherer A, Högenauer C, et al. (2018) Secondary tumors of the GI tract: origin, histology, and endoscopic findings. Gastrointestinal Endoscopy 88(1): 151-158.
- Weigt J, Malfertheiner P (2015) Metastatic Disease in the Stomach. Gastrointestinal Tumors 2(2): 61-64.
-
Shaheer Siddiqui, Tarun Jain, Zhenjian Cai, Scott Larson. Tia Leading to the Diagnosis Amelanotic Metastatic Gastric Melanoma. Acad J Gastroenterol & Hepatol. 1(3): 2019. AJGH.MS.ID.000511.
-
Polypoid gastric mass, Gastric melanoma, Disease, Histological diagnosis, Endoscopic, Polypoid necrotic mass, Epigastric pain, Nausea, Vomiting, Abdominal fulness
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.






