Mini Review
Mini Review
Rapid Review on Inflammatory Bowel Disease: Current Management and Future Research
Sepideh Khazeni, Freelance Research Scientist, Australia.
Received Date: October 12, 2021; Published Date: November 02, 2021
Mini Review
Inflammatory bowel disease (IBD) is a chronic and progressive inflammatory condition involving the gastrointestinal (GI) tract with an increased risk for colon cancer. Two main IBD are affecting the GI tract: Crohn’s disease (CD) that the inflammatory conditions that can affect the entire GI tract, and ulcerative colitis (UC), in which the inflammatory conditions only affect colonic mucosa [1]. Since 1990, the prevalence of IBD has been stabilizing in western countries, but the incident has been globally accelerating in newly industrialized countries in Africa, Asia, and South America [3]. The exacerbation of IBD forces an excessive economic burden on the healthcare system [4] and impairs patients’ quality of life [4, 5].
The systematic reviews highlighted the role of genetic and environmental factors as the main risk factors associated with the IBD, but the leading cause of IBD has not yet been fully understood [2]. Studies showed that patients with a family history of IBD have four times the risk of developing the disease [6]. Over 200 risk loci have been identified for IBD. Many loci overlap between IBD and some autoimmune disorders, particularly with psoriasis and ankylosing spondylitis [7]. In addition, some medications, such as oral contraceptives [8] and non-steroidal anti-inflammatory drugs [9], are associated with an increased risk of IBD, while Breastfeeding appears to decrease the risk of IBD [10]. Other than genetics, dietary intake might affect the risk of GI tract inflammation in CD and UC. For example, it has been reported that western diets with a high amount of total fats, total polyunsaturated fatty acids (PUFAs), omega-6 fatty acids, and meat might increase the inflammation in the GI tract and subsequently increase the risk of CD and UC. On the contrary, diets with an abundance of vegetable intake might decrease UC risk, and those richer in fibre and fruit might reduce the risk of CD [11].
Theoretically, the Mediterranean or vegetarian diet is more beneficial for IBD prevention and management than the western diet. Because the Mediterranean and vegetarian diets provide plentiful anti-inflammatory micronutrients, essential fatty acids, and fibres [12]. Further clinical studies can demonstrate the benefit of Mediterranean or vegetarian diets in the prevention, treatment, and management of IBD. Meta-analysis showed that Mediterranean Diet might prevent the development of IBD through gut microbiota [13]. Shifts in microbial composition in IBD patients between remission and active disease might contribute to IBD flare-up [14]. It is known that an increase in Fusobacterium bacterium is associated with IBD [13]. Limited clinical studies showed that probiotics might be as effective as conventional therapies in preventing IBD relapses [12]. However, the solid preclinical data suggested that probiotics can aid patients with IBD management [15]. Further clinical studies can demonstrate the benefit of the probiotics in prevention, treatment, and management of IBD.
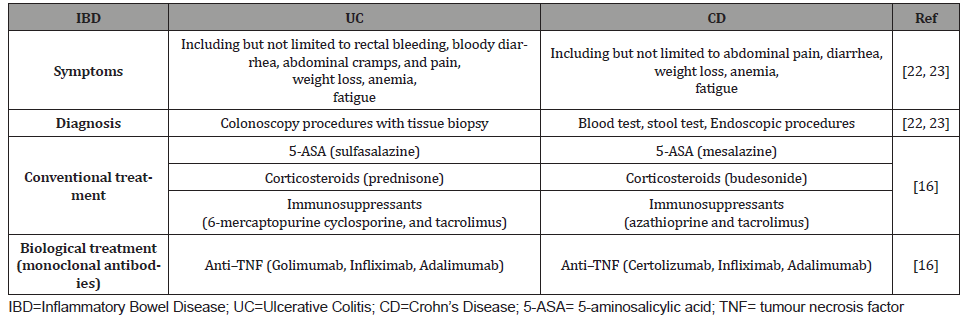
The IBDs are mainly managed with conventional therapy through groups of medications such as 5-aminosalicylic acid (5-ASA) derivatives, Corticosteroids, and immunosuppressants [16]. However, meta-analyses showed that in IBD patients, immunosuppressants such as methotrexate, azathioprine, and 6-mercaptopurine have no statistically significant advantage over placebo for induction of clinical response and remission [17]. Furthermore, meta-analyses showed superior clinical response induced by tacrolimus compared to placebo in patients suffering from UC. Tacrolimus also induced mucosal healing in UC patients [17]. The second-line therapy for IBD patients not responding to conventional treatment is biologic therapy by administrating monoclonal antibodies as anti–tumour necrosis factor [TNF], anti– integrins, and anti–cytokines [18]. The anti–TNF such as Golimumab and Certolizumab is prescribed for treatment or management of UC and CD, respectively. Moreover, other anti–TNFs such as Infliximab (IFX) and Adalimumab (ADA) are approved to manage both UC and CD. However, in severe IBDs, the increased levels of proteases, including matrix metalloproteinases (MMPs) in inflamed bowel, might fail the response to anti–TNFs [19].
(Table 1) summarised the correct IBD management. IBDs might increase the risk of developing extra-intestinal cancers. Meta-analyses demonstrated an increased risk of skin cancer by 2.2 fold and hepatobiliary malignancies by 2.3 fold in IBD patients. Furthermore, the risk of hematologic malignancies increased for CD patients by 2.4 fold and lung cancer by 1.53 fold [20]. The recent systematic review showed that in patients with IBDs, there is no risk associated with SARS-COV-2 infection. Moreover, IBD management by immunosuppressant or biologics might not affect the SARS-COV-2 infection prognosis. In contrast, IBD management by Corticosteroids might increase the risk associated with a worse prognosis of SARS-COV-2 infection [21-23].
Table 1:Summary of current IBD management.
As the current treatment and maintenance of IBD are costly for patients and the healthcare systems, herbal treatments might represent an effective complementary and alternative medicine [24]. In addition, several herbal medications might potentially be effective for the treatment of IBD as they are known to have antiinflammatory effects such as immunomodulatory properties, antimicrobial activities, antioxidant activities, and antiulcer [25]. Clinical studies showed that using herbal medicines such as curcumin, Aloe vera and Boswellia serrata could induce clinical remission or improvement in patients with mild or moderate IBD as effective as conventional therapy [26]. However, randomized controlled trials of herbal therapy for IBD treatment remain limited and heterogeneous [27]. Therefore, we suggest further clinical studies to better demonstrate the benefit of herbal medicines in the prevention, treatment, and management of IBD.
Acknowledgement
None.
Conflict of Interest
No conflict of interest.
References
- Arthur Kaser, Sebastian Zeissig, Richard S Blumberg (2010) Blumberg, Inflammatory Bowel Disease. Annu Rev Immunol 28(1): 573-621.
- Seyed Saeid Seyedian, Forogh Nokhostin, Mehrdad Dargahi Malamir (2019) A review of the diagnosis, prevention, and treatment methods of inflammatory bowel disease. J Med Life 12(2): 113-122.
- Siew C Ng, Hai Yun Shi, Nima Hamidi, Fox E Underwood, Whitney Tang, et al. (2017) Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: a systematic review of population-based studies. Lancet 390(10114): 2769-2778.
- Mike van der Have, Karen S van der Aalst, Ad A Kaptein, Max Leenders, Peter D Siersema, et al. (2014) Determinants of health-related quality of life in Crohn's disease: A systematic review and meta-analysis. J Crohns Colitis 8(2): 93-106.
- Marte L Hoivik, Bjorn Moum, Inger C Solberg, Milada Cvancarova, Ole Hoie, et al. (2011) Health-Related Quality of Life in Patients with Ulcerative Colitis After a 10-year Disease Course: Results from the IBSEN Study. Inflamm Bowel Dis 18(8): 1540-1549.
- Leena Halme, Paulina Paavola-Sakki, Ulla Turunen, Maarit Lappalainen, Martti Farkkila, et al. (2006) Family and twin studies in inflammatory bowel disease. World J Gastroenterol 12(23): 3668-3672.
- Luke Jostins, Stephan Ripke, Rinse K Weersma, Richard H Duerr, Dermot P McGovern, et al. (2012) Host–microbe interactions have shaped the genetic architecture of inflammatory bowel disease. Nature 491(7422): 119-124.
- Julie A Cornish, Emile Tan, Constantinos Simillis, Susan K Clark, Julian Teare, et al. (2008) The risk of oral contraceptives in the etiology of inflammatory bowel disease: a meta-analysis. Am J Gastroenterol 103(9): 2394-2400.
- Ashwin N Ananthakrishnan, Leslie M Higuchi, Edward S Huang, Hamed Khalili, James M Richter, et al. (2012) Aspirin, nonsteroidal anti-inflammatory drug use, and risk for Crohn disease and ulcerative colitis: a cohort study. Ann Intern Med 156(5): 350-359.
- Eyal Klement, Regev V Cohen, Jonathan Boxman, Aviva Joseph, Shimon Reif (2004) Breastfeeding and risk of inflammatory bowel disease: a systematic review with meta-analysis. Am J Clin Nutr 80(5): 1342-1352.
- Jason K Hou, Bincy Abraham, Hashem El-Serag (2011) Dietary intake and risk of developing inflammatory bowel disease: a systematic review of the literature. Am J Gastroenterol 106(4): 563-573.
- Rosa Reddavide, Ornella Rotolo, Maria Gabriella Caruso, Elisa Stasi, Maria Notarnicola, et al. (2018) The role of diet in the prevention and treatment of Inflammatory Bowel Diseases. Acta Biomed 89(9-S): 60-75.
- Illescas O, M Rodríguez Sosa, M Gariboldi (2021) Mediterranean Diet to Prevent the Development of Colon Diseases: A Meta-Analysis of Gut Microbiota Studies. Nutrients 13(7): 2234.
- Edgar S Wills, Daisy MAE Jonkers, Paul H Savelkoul, Ad A Masclee, Marieke J Pierik, et al. (2014) Fecal microbial composition of ulcerative colitis and Crohn's disease patients in remission and subsequent exacerbation. PloS one 9(3): e90981.
- Campieri M, P Gionchetti (1999) Probiotics in inflammatory bowel disease: New insight to pathogenesis or a possible therapeutic alternative. Gastroenterology 116(5): 1246-1249.
- Pithadia AB, S Jain (2011) Treatment of inflammatory bowel disease (IBD). Pharmacol Rep 63(3): 629-642.
- Adérson Omar Mourão Cintra Damião, Matheus Freitas Cardoso de Azevedo, Alexandre de Sousa Carlos, Marcela Yumi Wada, Taciana Valéria Marcolino Silva, et al. (2019) Conventional therapy for moderate to severe inflammatory bowel disease: A systematic literature review. World J Gastroenterol 25(9): 1142-1157.
- Ole Haagen Nielsen, Mark Andrew Ainsworth (2013) Tumor Necrosis Factor Inhibitors for Inflammatory Bowel Disease. N Engl J Med 369(8): 754-762.
- Paolo Biancheri, Randall J Brezski, Antonio Di Sabatino, Allison R Greenplate, Keri L Soring, et al. (2015) Proteolytic Cleavage and Loss of Function of Biologic Agents That Neutralize Tumor Necrosis Factor in the Mucosa of Patients With Inflammatory Bowel Disease. Gastroenterology 149(6): 1564-1574.e3.
- Bobby Lo, Mirabella Zhao, Ida Vind, Johan Burisch (2021) The Risk of Extraintestinal Cancer in Inflammatory Bowel Disease: A Systematic Review and Meta-analysis of Population-based Cohort Studies. Clin Gastroenterol Hepatol 19(6): 1117-1138.e19.
- Fabio Salvatore Macaluso, Ambrogio Orlando (2020) COVID-19 in patients with inflammatory bowel disease: A systematic review of clinical data. Dig Liver Dis 52(11): 1222-1227.
- Brian Veauthier, Jaime R Hornecker (2018) Crohn's Disease: Diagnosis and Management. Am Fam Physician 98(11): 661-669.
- Karsten Conrad, Dirk Roggenbuck, Martin W Laass (2014) Diagnosis and classification of ulcerative colitis. Autoimmun Rev 13(4-5): 463-466.
- Joos S (2011) Review on efficacy and health services research studies of complementary and alternative medicine in inflammatory bowel disease. Chin J Integr Med 17(6): 403-409.
- Roja Rahimi, Mohammad Reza Shams-Ardekani, Mohammad Abdollahi (2010) A review of the efficacy of traditional Iranian medicine for inflammatory bowel disease. World J gastroenterol 16(36): 4504-4514.
- Aikaterini Triantafyllidi, Theodoros Xanthos, Apostolos Papalois, John K Triantafillidis (2015) Herbal and plant therapy in patients with inflammatory bowel disease. Ann of gastroenterol 28(2): 210-220.
- SC Ng, YT Lam, KKF Tsoi, FKL Chan, JJY Sung, et al. (2013) Systematic review: the efficacy of herbal therapy in inflammatory bowel disease. Aliment Pharmacol Ther 38(8): 854-863.
-
Sepideh Khazeni, Bahareh Bigdeli. Rapid Review on Inflammatory Bowel Disease: Current Management and Future Research. Acad J Gastroenterol & Hepatol. 3(1): 2021. AJGH.MS.ID.000555.
-
Inflammatory bowel disease, Corticosteroids, Immunosuppressants, Extra-intestinal cancers, Skin cancer, Lung cancer, Conventional therapy, Hepatobiliary malignancies
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.