 Case Report
Case Report
Role of Nutritional Rehabilitation in Managing Prolapsed Intussusception in A Malnourished Child in Northwest Nigeria: A Case Report
AKINBODE Akeem Opeyemi1*, MUHAMMAD Daniyan2 and SALIHU Abdullahi3
1Department of Family Medicine, Federal Teaching Hospital, Birnin Kebbi, Nigeria
2Department of Surgery, Ahmadu Bello University Teaching Hospital, Zaria, Nigeria
3Department of Surgery, Federal Teaching Hospital, Birnin Kebbi, Nigeria
AKINBODE Akeem Opeyemi, Department of Family Medicine, Federal Teaching Hospital, Birnin Kebbi, Nigeria
Received Date:March 22, 2025; Published Date:April 08, 2025
Introduction
Intussusception is the condition whereby a part of the bowel folds into the part next to it. It is a surgical disease which involves the small intestine and sometimes the large intestine [1-4]. Intussusception is more common among children, than in adults. Among children, males are more commonly affected than females. The incidence is highest within the age range of 6 to 18 months [5]. Incidence of the condition increases with incidence of viral gastroenteritis within some populations. Infections such as Adenovirus infection, Salmonella, Escherichia, Shigella, Campylobacter, have been observed as a risk factors, with intussusception occurring a month following the infections [6-8]. The exact cause is said to be typically unknown when it occurs in children, unlike in adults whereby a lead point like a cancer in common. Risk factors among children are cystic fibrosis, infections, and intestinal polyps [9].
The symptoms of the condition include abdominal pain (sometimes waxing and waning), vomiting (greenish), bloating, and passage of bloody / red ‘currant’ jelly stool, and lethargy. Examination may reveal pulling of legs to the chest, a ‘sausage-shaped’ mass, and dyspnea with pain paroxysms. Complications that can arise from it are intestinal obstruction, peritonitis, or bowel perforation [1-4]. An ultrasound scan is the preferred diagnostic method for children; however, a CT scan is preferred in adults. Treatment of intussusception in children is typically with the use of enema, followed by surgery [9]. Intussusception is usually, not immediately a life-threatening condition, with treatment with air contrast, barium, or water-soluble enema, for confirmation of diagnosis, and successful treatment with success rate greater than 80%, and up to 10% re-occurring within 24 hours. Rare complications a pyloro-duodeno- jejunal intussusception and prolapsed intussusception. Prolapse of intussusception is an uncommon complication of intussusception [10]..
Case Report
We present a case of H.A., who was a 20-month-old boy of Hausa ethnicity, and of Muslim parents, who was managed at Federal Teaching Hospital, Birnin Kebbi. He was presented (by parents) on account of anal protrusion of five hours duration, and abdominal pain of two hours duration. About five hours prior to presentation, his mother noticed him to be having a protrusion from the anus while going to bath the child in the early hours of the morning. The protruding mass was pushed inside manually after defaecation, but was later noticed few minutes afterwards. It progressively worsened and could not be reduced manually by the mother again, resulting in continuous extrusion of the swelling. This presenting episode was the fifth, as the child has been experiencing similar episodes within the previous two months.
Abdominal pain was colicky, appeared to be lower, as the child was holding his lower abdominal region, with associated crying. There was inability to defaecate in the previous 24 hours (constipation), with associated bilious vomiting. There was no associated fever, and reduction in abdominal size. No yellowness of the eyes. Stool was intermittently stained with blood and child cries during the episode. There was history of recurrent vomiting and diarrhea before the onset of the index symptom. There was no prior respiratory tract infection, no current history of immunization. He was the second child of mother in a monogamous setting. Parents had no formal education.
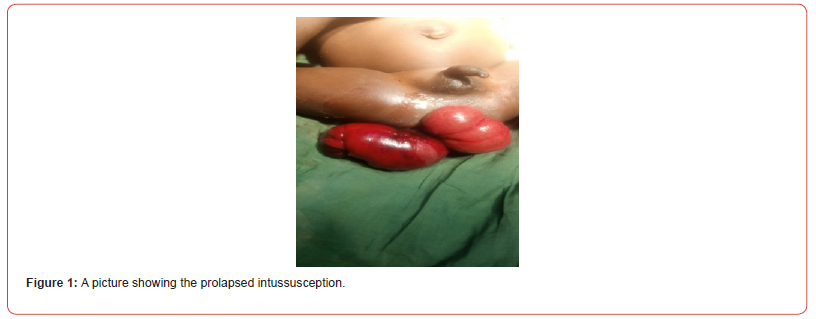
Examination revealed a young child, ill-looking, moderately pale, anicteric, afebrile, and moderately dehydrated. He was not cyanosed, had no significant peripheral lymph node enlargement, and no pedal oedema. His OFC was 45cm (92% of expected). Weight was 10 kg (83% of expected) and Height was 76cm (93% of expected). Pulse rate was 130 bpm, and blood pressure was 90/60 mmHg. Heart sounds were the first and second only. Respiratory rate was 26 cpm, Chest had vesicular breath sound. Abdomen was flat, moved with respiration, with visible peristalsis, but no dance sign. There was no area of tenderness. Bowel sound was hyperactive. Digital ano-rectal examination showed prolapsed bowel through the anus, which finger could be insinuated within the mucocutaneous junction leading to an indefinite and cleft. Prolapsed bowel was oedematous, with area of hypopigmentation, Inner lumen of bowel was appreciable at the peak of the prolapse (Figure 1 & 2). Examining gloved finger was stained with bloody mucoid discharge.
An assessment of Prolapsed Intussusception in a malnourished child was made.
Management involved counseling parents for exploration and repair of lesion. He was placed on nil per orals. Warm saline-soaked gauze was applied to protect and reduce swelling. Nasogastric tube was inserted. Urethral catheter was placed. Intravenous fluid 4.3% Dextrose saline 300 ml 8 hourly; IV Paracetamol 120 mg 8 hourly; IV Ciprofloxacin 80mg 12-hourly; and IV Metronidazole 120mg 8-hourly were commenced. Place patient in Trendelenburg position. Full blood count (FBC), Electrolyte, Urea, and Creatinine (EUCr), and Serum protein were requested. Full blood count showed: WBC 27.28 X 106/ul; Lym 74.8%; Gra 8.9%; Plt 231 X 106/l; PCV 25.5%; Hgb 8.5g/dl. EUCr showed Na 130mmol/l, K 4.8 mmol/l, Cl 90 mmol/l, Ur 5.5mmol/l, Cr 30mmol/l. Retroviral screening, HBsAg and HCV were all non-reactive. Abdominopelvic Ultrasound scan revealed features of dilated bowels, and no mass of fluid collection was noticed in the abdominal cavity.
Within 48 hours, child had trial of Koch’s procedure in Trendelenburg position which failed as the distal aspect of the protrusion was gangrenous. He then had exploratory laparotomy via a transverse supraumbilical incision, dipping through subcutaneous tissue, rectus sheath, rectus abdominis muscle and into the peritoneal space. Operative findings were long segment ileocolic intussusception; gangrenous terminal ileum (about 10cm), caecum, appendix, ascending colon, and mid-transverse colon and proximal descending colon; dilated proximal small bowel. Multiple inflamed mesenteric lymph nodes and serous ascitic fluid. Subsequently, per rectal ileo-colic resection was done which was then brought out as stoma in the right iliac fossa. Fascia and skin of the primary were closed in layers. Histology of the resected segments showed features of gangrenous tissues.
The post-operative period was smooth, as the patient was placed on parenteral antibiotics, food and fluid therapy, strict fluid input – output charting, and vital signs’ monitoring. Patient was discharged two weeks later and mother was taught above stoma care. He was scheduled for clinic follow up on a monthly basis. He subsequently had Reversal of ileostomy (Ileostomy closure and minimal adhesiolysis) under stable conditions done eight months later. Patient recovered completely and regained normal bowel movements subsequently.

Discussion
Intussusception is a surgical condition manifesting as the telescoping of a part of the bowel into another, usually within the abdominal cavity (Tiexeria, 2022). The index patient presented with a rare complication of intussusception, in the form of prolapse of the mass of intussusception outside of the anus. The patient had a grossly visible bowel mass protruding out of the anus, with difficulty in reducing the mass manually.
Intussusception is more common in children than in adults, and males have incidence (Minney-Smith, 2014). The case occurred in a male infant of 20 months of age. Although the age was slightly higher, the child was reported by parents to have been experiencing protrusion of the mass for 2 months. Therefore, the initial onset of the intussusception could have been when the child was less than 18 months, thus, in support of the age range according to literature stated earlier. The socio-demographic features are in conformity with those found in the literature earlier stated. There was history of recurrent vomiting and diarrhoea, which are likely due to gastroenteritis. Thereby suggesting an infectious aetiology in the patient, which is one of the risk factors according to studies (Pham, 2017; Wu 2019; Shen, 2020; Zhang, 2021). The patient had most of the known symptoms of intussusception, but there was no ‘sausage- shaped mass’, which if found, could have raised suspicion of a separate rectal prolapse from an intra-abdominal intussusception.
Illiteracy of the parents, was a contributory social factor, as they were unable to see the symptom as an emergency requiring attending health facility immediately. Thus, the delay in presentation must have added to the complications of prolapse and gangrene in the patient. Other social problems included long distance from the tertiary health centre, where the patient had treatment, and lack of capable facility close to patient’s home.
The patient, at presentation appeared malnourished, with the anal-prolapsing mass looking darkish-brown in colour (it was actually gangrenous on examination pre- and intra-operatively). The child on examination held his legs around the chest, although typical/ classical of intussusception, could be due to avoidance of the mass with his legs.
Reduction was attempted on the operative table, but failed due to the adhesive nature of the clump/mass into which waves of bowel have entered. Laparotomy was therefore done, and per-rectal ileo- colic resection of the gangrenous bowel was done, with ileostomy done. Reversal of ileostomy was done after 12 weeks, when the child has regained previously lost physiologic status.
Mother was counselled on the use of locally available food products for preparing nutritious diets for the child. The patient was referred to the nutritionist for the commencement of nutritional rehabilitation in the hospital before the patient was discharged.
Conclusion
Intussusception occurs majorly in male under-five children, presenting as a gastrointestinal surgical emergency. The index patient had delayed presentation of his intussusception, which had become prolapsed through the anus, and became gangrenous in some segments. Patient had resection of gangrenous bowel, ileostomy, reversal of ileostomy, and nutritional rehabilitation as core components of management with successful outcome. Peculiar features in the patient were prolapse and gangrene of the intussusception. Initial malnutrition made the condition to be complicated in him, although optimal care helped in positive outcome.
Declaration of Patient Consent
The authors hereby certify that appropriate consent was obtained using the patient consent form. Patient’s mother gave consent for the patient’s clinical information to be reported in a journal. The patient’s mother understood that the patients name and other identifying details would not be published, and due efforts to ensure concealment of identity would be made.
Conflicts of Interest
The authors declare no conflict of interest.
Funding
Nil.
References
- McRae JE, Quinn HE, Saravanos GL, Mcminn A, Britton PN, et al. (2019) Paediatric Active Enhanced Disease Surveillance (PAEDS) annual report 2016: Prospective hospital-based surveillance for serious paediatric conditions. Commun Dis Intell 43.
- Jia Y, Fu H, Li N, Kang Q, Sheng J (2018) Diagnosis and treatment for 46 cases of Peutz-jeghers syndrome. 43(12): 1323-1327.
- Restivo V, Costantino C, Giorgianni G, Guccia M, Tramuto F, et al. (2018) Case-control study on intestinal intussusception: implications for anti-rotavirus vaccination. Expert Rev Vaccines 17(12): 1135-1141.
- Teixeira H, Hauswirth F, Romer N, Muller MK, Baechtold M (2022) An ileo-colic intussusception reaching down to the descending colon – A case report. Int J Surg Case Rep 93: 107009.
- Minney Smith CA, Levy A, Hodge M, Jacoby P, Williams SH, et al. (2014) Intussusception is associated with the detection of adenovirus C, enterovirus B, and rotavirus in a rotavirus vaccinated population. J Clin Virol 61(4): 579-584.
- Pham T, La Paglia D, Pitcher M (2017) Salmonella enteritis: a rare cause of adult intussusception. Ann Coloproctol 33(5): 201-203.
- Wu PW, Wang CC (2019) Concurrent Campylobacter jejuni bacteremia and intussusception in an immunocompromised five-year-old child. J Microbiol Immunol Infect 52(2): 367-369.
- Shen G, Liu H, Guan Z, Shang X, Li J, et al. (2020) Clinical features and clinical factors leading to early recurrence of intussusception after saline reduction. J Pak Med Assoc 70(10): 1727-1730.
- Zhang B, Wu D, Liu M, Bai J, Chen F, et al. (2021) The diagnosis and treatment of retrograde intussusception: a single centre-experience. BMC Surg 21(1): 398.
- Bogdanovic M, Blagojevic M, Kuzmanovic J, Jecmenica D, Alempijevic D (2025) Fat intussusception in infancy: forensic implications. Forensic Science.
-
AKINBODE Akeem Opeyemi*, MUHAMMAD Daniyan and SALIHU Abdullahi. Role of Nutritional Rehabilitation in Managing Prolapsed Intussusception in A Malnourished Child in Northwest Nigeria: A Case Report. Acad J Gastroenterol & Hepatol. 4(2): 2025. AJGH.MS.ID.000583.
-
Nutritional Rehabilitation; Malnourished Child; Intussusception; surgical disease; large intestine; abdominal pain
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Track Your Article
Refer a Friend
Advertise With Us
Feedback
 a Creative Commons Attribution 4.0 International License. Based on a work at www.irispublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.irispublishers.com.
Best viewed in





