 Research Article
Research Article
Pilot Study of the Effects of Red Wine Intake in Metabolic Associated Fatty Liver Disease
Thomas Worland1*, Duy Pham1, Sarah Gardner1, Samuel Hui1, Brooke Chapman2,3, Mark Goodwin3,4, Marie Sinclair1,3, Adam Testro1,3, Peter Angus1,3 and Paul Gow1,3
1Liver Transplant Unit, Austin Health, Melbourne, Australia
2Department of Nutrition and Dietetics, Austin Health, Melbourne, Australia
3University of Melbourne, Melbourne, Australia
4Department of Radiology, Austin Health, Melbourne, Australia
Thomas Worland, Monash medical centre, 246 Clayton Road Clayton, Australia
Received Date:April 22, 2024; Published Date:April 29, 2024
Abstract
Background and aims: Metabolic associated fatty liver disease (MAFLD) is the most common cause of liver disease worldwide. The potential
impact of moderate alcohol consumption on MAFLD remains controversial. This pilot randomized controlled study aimed to assess the effect of
moderate red wine consumption on liver steatosis in non-drinkers with MAFLD.
Materials and Methods: Twelve patients were given individualized low caloric dietary advice and randomized to receive red wine or no
alcohol for 12 weeks. Participants underwent hepatic magnetic resonance spectroscopy and transient elastography at baseline and 12 weeks, and
anthropometric measures and blood testing at baseline, week 6, and week 12.
Results: There were no significant differences between groups in terms of demographics, comorbidities, metabolic/steatosis risk, or
biochemistry. No statistically significant differences in any outcomes were seen between groups over the study period.
Discussion: Moderate intake of wine was not associated with any difference in liver related outcomes, compared to control, in patients with
MAFLD. This study serves as a methodologic template for future larger studies investigating moderate alcohol intake in MAFLD.
Keywords: Wine; Fatty liver; Magnetic resonance imaging
Abbreviations: ALT: Alanine Transaminase; ANOVA: Analysis of Variance; AST: Aspartate Transaminase; BGL: Blood Glucose Level; BMI: Body Mass Index; CAP: Controlled Attenuated Parameter; CRP: C-Reactive Protein; dB/m: Decibel per milliwatt; ESR: Erythrocyte Sedimentation Rate; HOMA-IR: Homeostatic Model Assessment for Insulin Resistance; IQR: Interquartile Range; kPa: Kilopascal; MAFLD: Metabolic Associated Fatty Liver Disease; MRI: Magnetic Resonance Imaging; MRS: Magnetic Resonance Spectroscopy; PDFF: Protein Density Fat Fraction
Introduction
Metabolic associated fatty liver disease (MAFLD) is the most common cause of liver disease worldwide [1]. Despite significant advances in our understanding of MAFLD, there are currently no well-established pharmacological therapies with treatment directed primarily at lifestyle interventions. The potential impact of moderate alcohol consumption on MAFLD remains controversial. Observational research in participants with metabolic syndrome has demonstrated improvements in metabolic markers following commencement of moderate alcohol intake [2,3], and a cross sectional study has found less severe histology and fibrosis in those who drank modest alcohol compared with non-drinkers [4]. Other data suggests modest alcohol use is associated with MAFLD progression [3,5]. A randomized controlled trial investigating the effect of modest alcohol, as white and red wine, on metabolic risk in patients with type 2 diabetes found moderate intake of both types of wine to be associated with improvement of cardiovascular risk, with a greater effect seen in the red wine compared with the white wine group [6]. There are currently no published RCTs that explore the effects of moderate alcohol intake in patients with MAFLD. We describe a randomised-controlled pilot study to assess the effect of the commencement of moderate red wine consumption on hepatic fat content, Fibroscan scores, liver biochemistry, and markers of the metabolic syndrome in non-drinkers with MAFLD.
Materials and Methods
A non-blinded randomized controlled trial was conducted. Twelve patients with MAFLD were recruited (six male, six female) and followed for 12 weeks. The study was approved by the local research ethics committee. Patients were considered for study inclusion if they were >18 years of age, were non-alcohol drinkers (defined as one or less standard drink per week), and fulfilled diagnosis for MAFLD (confirmed by cross-sectional imaging of steatosis, liver biopsy, and/or elevated Controlled Attenuated Parameter (CAP) score on transient elastography). Patients were excluded if their baseline Magnetic Resonance Imaging (MRI) revealed <10% hepatic steatosis, if they had cirrhosis/comorbid liver disease other than MAFLD, were pregnant/breastfeeding, or had contraindications to MRI. Participants were randomized by sealed envelope method to alcohol or control groups in a 1:1 ratio. At study commencement all patients were reviewed by a specialist liver dietician. Individualised advice was provided to achieve a target caloric reduction of 500-1000 kcal per day and weight loss of 0.5-1.0 kg per week in accordance with international guidelines [7]. In addition to dietary advice, participants randomized to the intervention arm were provided with red wine. Male participants were instructed to consume 20g alcohol per day with two alcoholfree days per week. Female participants were instructed to drink 10g alcohol per day and two alcohol-free days per week. These quantities were based on Australian alcohol intake guidelines [8]. Red wine was selected due to potential increased metabolic benefits compared to other alcohol types [6].
To ensure adherence to dietary advice and assess red wine intake, the study dietician reviewed all participants in person at baseline, week 6 and 12, and contacted them by telephone week 3 and 9. All participants kept an ‘alcohol diary’ to record daily red wine intake. Participants underwent hepatic MR spectroscopy (MRS) and transient elastography with CAP at baseline and 12 weeks. Anthropometric measures and blood testing for metabolic markers and liver biochemistry were performed at baseline, week 6, and week 12. Hepatic steatosis was measured using MRI Protein Density Fat Fraction (PDFF), considered the gold standard for quantification of hepatic steatosis. MR spectroscopy (MRS) to calculate intrahepatic lipid was also calculated. MRI scans were performed on a Siemens Magnetom Skyra 3T magnet (Siemens Medical Solutions, Erlangen, Germany). A high-speed T2 corrected multi echo MRS technique made available by Siemens WIP was utilised. The fat percentage was the fat signal fraction as determined with MRS and MRI Protein Density Fat Fraction (PDFF). Image analysis was performed by a single experienced hepatobiliary radiologist who was blinded to study arm allocation.
Prior dietary intervention studies demonstrating improvements in liver steatosis over 4 weeks were used to inform power calculation for a total patient size population of 12 [9]. Outcome measures included change in liver fat burden on MRS, anthropometry, transient elastography/CAP, and biochemical markers of hepatic injury from baseline to week 12. We also aimed to explore the logistics of using moderate alcohol as an intervention in a population of non-drinkers. One-way ANOVA was used to compare parametric continuous variables. Pearson chi square test was used to compare categorical variables and adjusted residuals. Significance tests were two-tailed with a p value of <0.05 considered statistically significant. Two-way repeated measures ANOVA was used to evaluate changes in continuous data variables.
Results
Thirteen patients were randomised (one patient withdrew consent immediately following randomisation and was excluded). Seven patients were randomised to intervention and five to dietary control. Baseline characteristics are listed in Table 1a. There were no significant differences between groups in terms of demographics, comorbidities, metabolic/steatosis risk, or biochemistry. Eleven patients completed all visits and study interventions and investigations (one patient in the wine intervention arm withdrew following the first visit due to their inability to commit further time to the study). All patients reported excellent compliance to dietary interventions with no difference between groups, and the intervention group had complete compliance with red wine intake. Baseline characteristics were similar between groups (Table 1a). No major numerical changes were seen within groups for all parameters over the study period, and there were no significant differences in degree of change from weeks zero to 12 between the intervention and control groups for all parameters (Table 1b). Change in percentage liver steatosis in each individual as determined by PDFF is displayed in Figures 1a & 1b; change of steatosis over the study time period was not significantly different between groups (P = 0.63). There were no adverse effects associated with interventions and investigations associated with the study.
Discussions
This pilot study did not show any significant effect of moderate red wine intake on changes in liver parameters in patients with MAFLD who were recommended a modest calorie restricted diet for 12 weeks. No detrimental effect was seen in the wine group, nor significant difference in outcomes between groups. Both groups were placed on identical weight loss diets for 12 weeks, however additional caloric intake was unavoidably present in the wine group due to the caloric content of wine. Despite this there was no difference in change in liver parameters between groups over the 12 weeks; it is hence possible that the putative beneficial effect of red wine on fatty liver abrogated the extra caloric load.
Prior observational research investigating moderate alcohol use in patients with MAFLD has had conflicting findings. Some series have found moderate alcohol use to be associated with a worsening of surrogate markers of metabolic syndrome and MAFLD [3,5], other series, however, report long-term beneficial effect on allcause mortality [10] and decreased prevalence of steatohepatitis in patients with baseline MAFLD [4]. These observational studies included modest drinkers of any alcohol type, and thus potential differences of outcome associated with beverage type was not investigated. A randomised-controlled trial that did specify alcohol type did not find any difference between red wine, white wine, and mineral water groups for liver biochemistry.
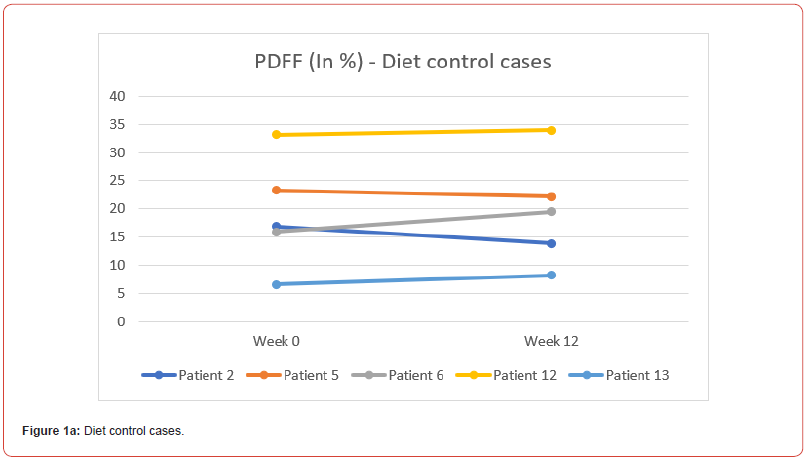
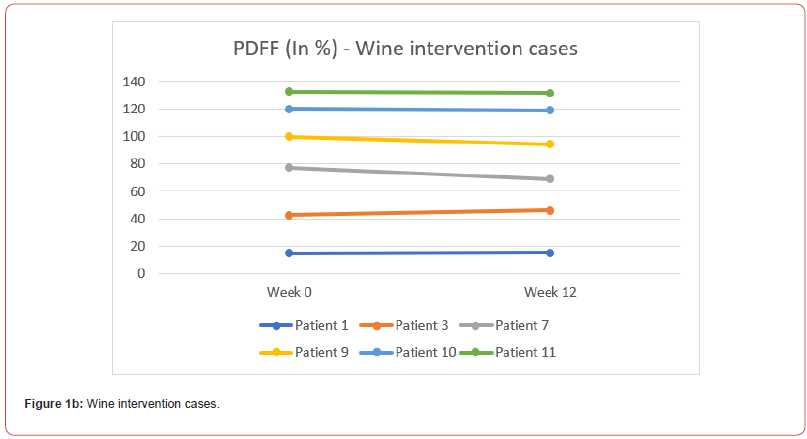
Table 1a:
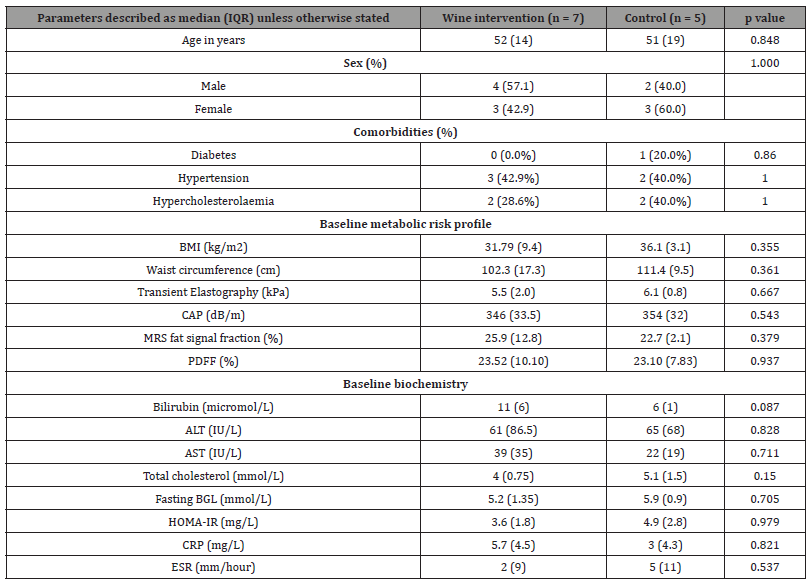
IQR: Interquartile Range, BMI: Body Mass Index, kPa: Kilopascal, CAP: Controlled Attenuated Parameter, dB/m: Decibel per milliwatt, MRS: Magnetic Resonance Spectroscopy, PDFF: Protein Density Fat Fraction, ALT: Alanine Transaminase, AST: Aspartate Transaminase, BGL: Blood Glucose Level, HOMA-IR: Homeostatic Model Assessment for Insulin Resistance, CRP: C-Reactive Protein, ESR: Erythrocyte Sedimentation Rate.
Table 1b:
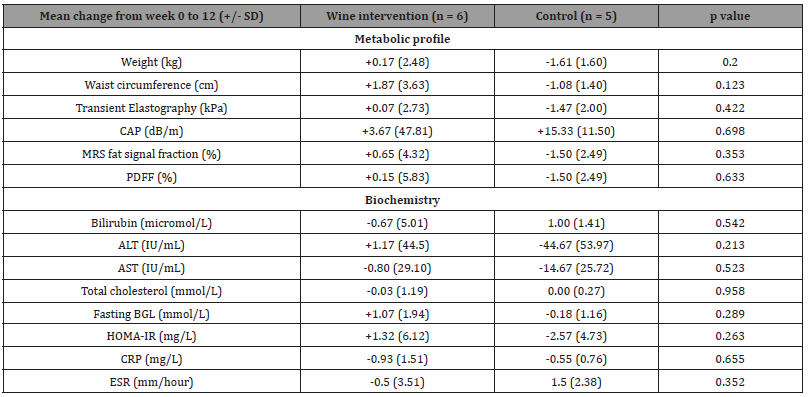
SD: standard deviation, kPa: Kilopascal, CAP: Controlled Attenuated Parameter, dB/m: Decibel per milliwatt, MRS: Magnetic Resonance Spectroscopy, PDFF: Protein Density Fat Fraction, ALT: Alanine Transaminase, AST: Aspartate Transaminase, BGL: Blood Glucose Level, HOMA-IR: Homeostatic Model Assessment for Insulin Resistance, CRP: C-Reactive Protein, ESR: Erythrocyte Sedimentation Rate
Due to conflicting literature regarding the impact of moderate alcohol on MAFLD, there is a need for a well-designed randomised controlled trial investigating alcohol as a therapy for MAFLD; red wine appears the form of alcohol most likely to have a potential metabolic beneficial effect. Type 2 errors are potentially present; a greater number of participants may have found statistically significant separation of groups. We demonstrated the feasibility of randomizing non-drinkers to a moderate alcohol intervention with good compliance and no adverse safety signals, in particular no worsening of liver biochemistry, non-invasive measures of liver fat, or metabolic markers. This pilot study addresses a major gap in the literature, and provides clear methodology for designing an adequately powered study with robust endpoints to further investigate the impact of moderate alcohol in this population. Our study provides the foundation for larger similarly conducted trials on red wine that could potentially provide a therapy for patients with early stage MAFLD, and provide data to allow clinicians to safely counsel their patients in regards to safe levels of alcohol intake.
Funding Statement
No external funding was sought for this investigator-initiated study.
Conflict of Interest Statement
None declared for all authors
Ethics Approval Statement
This study was approved by the local ethics committee. Written patient consent was gained for all participants.
References
- Gan L, Chitturi S, Farrell GC (2011) Mechanisms and implications of age-related changes in the liver: nonalcoholic Fatty liver disease in the elderly. Curr Gerontol Geriatr Res 2011: 831536.
- Di Castelnuovo A, Costanzo S, Bagnardi V (2006) Alcohol dosing and total mortality in men and women: an updated meta-analysis of 34 prospective studies. Arch Intern Med 166(22): 2437-2445.
- Chang Y, Cho YK, Kim Y (2019) Nonheavy Drinking and Worsening of Noninvasive Fibrosis Markers in Nonalcoholic Fatty Liver Disease: A Cohort Study. Hepatology 69(1): 64-75.
- Dunn W, Brunt EM, Unalp-Arida A (2012) Modest alcohol consumption is associated with decreased prevalence of steatohepatitis in patients with non-alcoholic fatty liver disease (NAFLD). Hepatology 57(2): 384-391.
- Ajmera V, Belt P, Wilson L (2018) Among Patients with Nonalcoholic Fatty Liver Disease, Modest Alcohol Use Is Associated with Less Improvement in Histologic Steatosis and Steatohepatitis. Clin Gastroenterol Heptaol 16(9): 1511-1520.
- Gepner Y, Golan R, Harman Boehm I (2015) Effects of Initiating Moderate Alcohol Intake on Cardiometabolic Risk in Adults with Type 2 Diabetes: A 2-Year Randomized, Controlled Trial. Ann Intern Med 163(8): 569-579.
- Chalasani N, Younossi Z, Lavine J (2018) The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology 67(1): 328-357.
- (2020) NHMRC. Alcohol | NHMRC.
- Dunn W, Xu R, Schwimmer J (2008) Modest wine drinking and decreased prevalence of suspected nonalcoholic fatty liver disease. Hepatology 47(6): 1947-1954.
- Åberg F, Puukka P, Salomaa V (2020) Risks of Light and Moderate Alcohol Use in Fatty Liver Disease: Follow-Up of Population Cohorts. Hepatology 71(3): 835-848.
-
Thomas Worland*, Duy Pham, Sarah Gardner, Samuel Hui, Brooke Chapman, Mark Goodwin, Marie Sinclair, Adam Testro, Peter Angus and Paul Gow. Pilot Study of the Effects of Red Wine Intake in Metabolic Associated Fatty Liver Disease. Acad J Gastroenterol & Hepatol. 3(5): 2024. AJGH.MS.ID.000572.
-
Wine; Fatty liver; Magnetic resonance imaging; Iris Publishers; Iris Publishers Indexing Sites
-

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Track Your Article
Refer a Friend
Advertise With Us
Feedback
 a Creative Commons Attribution 4.0 International License. Based on a work at www.irispublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.irispublishers.com.
Best viewed in





